To identify the existing literature on mothers’ perception towards the impact of expressing breast milk for their premature infant in the neonatal intensive care unit.
MethodGuided by the PRISMA Statement review checklist, a systematic review of the Scopus and Web of Science database has identified 10 related studies. The articles were assessed and analyzed after evaluated using The Joanna Briggs Institute Critical Appraisal tools (JBI). Thematic analysis was obtained after using Nvivo software as a tool for data analysis by author.
ResultFurther review of these articles resulted in three main themes—maternal changes during expressing breast milk, pumping challenges and impact of motivation factors to initiating lactation.
ConclusionExpressing breast milk should be recognized as an important way to restructure motherhood with a preterm infant in NICU. However, maintaining expressed breast milk during preterm infants’ treatment period in NICU may increase stress and difficulties for some mothers. Some recommendations are emphasized in relation to the need for more qualitative studies in this issue, which is to have a specific and standard systematic review method for guide research synthesis in context of climate change adaptation.
The growing advancement of technology and treatment in medical will increase the prevalence survival of premature infants worldwide. Infants that are delivered before 37 weeks of gestation categorizes as premature infants and most of them would require observation and intensive treatment.1 The organization reported that India has the highest rate of premature births with 3,519,100 infants and 15.5 per 100 live birth, while Indonesia is in the 10 countries with the highest rate of premature delivery.1 Meanwhile, the impact of preterm birth can lead to poorer long-term health outcomes for the baby, including neurodevelopmental, cognitive and behavioural problems.2,3
Breast milk is the main source of nutrition for all infants, especially preterm infants and ill newborns.4–6 The beneficial effects of breast milk are related to improvements in an infant's antibody, rich of nutrients, enteral tolerance, and better neurodevelopmental outcome and recommends for all newborn infants.7 Breastfeeding also enhances the maternal involvement and mother–infant interaction and bonding, which can be compromised in the neonatal intensive care unit (NICU) setting. Worldwide efforts are underway to encourage and support mothers’ milk feeding in the NICU. Mothers of premature infant play an important role in the supply of expressed breast milk for their infant. However, mothers of preterm infants encounter a variety of unique breastfeeding barriers and challenges that result in a decreased rate of breastfeeding in preterm infants compared with term infants.8
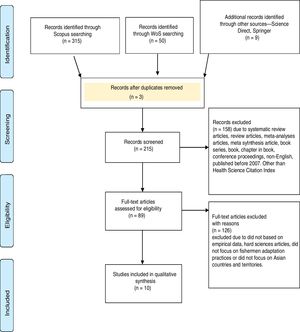
MethodThe reviewers used the method called PRISMA, which includes resources (Scopus and Web of Science) to run the systematic review, eligibility and exclusion criteria, steps of the review process (identification, screening and eligibility), and data abstraction and analysis.
Systematic review processIdentificationFour stages were involved in the systematic review process and the review process was performed on June 2018. The first phase identified keywords used for the search process. Relying on previous studies and thesaurus, keywords similar and related to climate change, adaptation and farming community were used (Table 1). At this stage, after careful screening, two duplicated articles were removed.
The inclusion and exclusion criteria.
| Criteria | Eligibility | Exclusion | Keywords and searching information strategy |
|---|---|---|---|
| Literature type | Journal (research articles) | Journals (systematic review), book series, book, chapter in book, conference proceedings | ALL (“expressed breast” OR “breast milk expression”) AND (“premature infant” OR “preterm”) AND (“neonatal intensive care unit”) |
| Language | English | Non-English | |
| Timeline | Between 2007 and 2018 | Before 2007 | |
| Indexes | Health Science Citation Index | Social Science Citation Index, Emerging Sources Citation Index, Art and Humanities Index (Web of Science) | |
| Countries | Worldwide | Non |
Several eligibility and exclusion criteria are determined. Firstly, with regard to the literature type, only article journals with empirical data are selected, which means review article, book series, book, chapter in book, and conference proceedings are all excluded. Secondly, in order to avoid any confusion and difficulty in translating, the searching efforts excluded the non-English publications and focused only on articles published in English. Thirdly, with regard to the timeline, a period of 11 years is selected (between 2007 and 2018), an adequate period of time to see the evolution of research and related publications. As the review process focused on EBM for premature infant in the NICU, articles indexed in health science-based indexes are selected. Lastly, in-line objectives, which focus on getting the general view of the current issue worldwide (Fig. 1).
Data abstraction and analysisThe remaining articles were assessed and analyzed after assessed using The Joanna Briggs Institute Critical Appraisal tools (JBI). Efforts were concentrated on specific studies that responded to the formulated questions. The data were extracted by reading through the abstracts first, and then the full articles (in-depth) to identify appropriate themes and sub-themes. Qualitative analysis was performed using content analysis to identify themes related to existing literature on mothers’ perception towards the impact of expressing breast milk for their premature infant in the neonatal intensive care unit. The authors then organized sub-themes around the themes established by typology (Table 2).
An overview of the included studies.
| Author | Country | Study design | Setting | Number of participants (n) |
|---|---|---|---|---|
| Bower et al., 2017 | USA | Qualitative, phenomenology, in-depth interview | NICU, Level III | 17 mothers |
| Ikonen et al., 2016 | Finland | Qualitative, open-ended questionnaire, internet-based questionnaire | Internet-based questionnaire | 130 mothers |
| Henderson, 2015 | USA | Mixed method study | 62 beds NICU, Level IV | 20 mothers |
| Hurst et al., 2013 | USA | In-depth interview, ethnographic approach | NICU, Level III and II | 14 mothers |
| Rossman et al., 2013 | USA | Qualitative, in-depth semi-structured interview, descriptive | 57-bed, NICU, Level III | 23 mothers |
| Dowling et al., 2012 | USA | Qualitative | 15 NICU25 single family room | 40 mothers |
| Wilson, 2012 | England | Descriptive phenomenology, semi-structured interview | NICU | 8 mothers |
| Boucher et al., 2011 | Canada | Descriptive qualitative, semi-structured interviews | NICU, Level III | 10 mothers |
| Sisk et al., 2010 | USA | Qualitative, in depth interview | 56-bed, NICU | 32 mothers |
| Lee et al., 2009 | Taiwan | Descriptive, In-depth interview | Home visit | 31 mothers |
The review resulted in three main themes and seven sub-themes related to mothers’ perceptions towards the expressing breast milk for their premature infant in the neonatal intensive care unit. The three main themes are maternal physical and mental changes, pumping challenges and motivation factors during expressing their breast milk. The results provided a comprehensive analysis of the current mothers’ perceptions towards expressing breast milk.
A total of six studies were focused on the United States9–14; one study each was concentrated on mothers in Finland,15 mothers’ perceptions in England,16 one more in Canada,17 and another one was conducted in Taiwan, focused on mothers’ experiences.18 Furthermore, nine studies applied the qualitative approach, while another study employed a mixed method (qualitative+quantitative) approach. Regarding the years published, one article was published in 2009, 2010, 2011, 2015, 2016, and 2017, each; while two studies were published in 2012 and 2013 (Table 3).
Finding of systematic literature review.
| Studies | Findings |
|---|---|
| Bower et al., 2017 | Maternal changes, motivation factors |
| Ikonen et al., 2016 | Maternal changes, pumping challenges and motivation factors |
| Henderson, 2015 | Maternal changes, pumping challenges |
| Hurst et al., 2013 | Maternal changes, pumping challenges and motivation factors |
| Rossman et al., 2013 | Pumping challenges and motivation factors |
| Dowling et al., 2012 | Pumping challenges |
| Wilson, 2012 | Maternal changes, motivation factors |
| Boucher et al., 2011 | Maternal changes, pumping challenges and motivation factors |
| Sisk et al., 2010 | Maternal changes, pumping challenges |
| Lee et al., 2009 | Maternal changes, motivation factors |
Physical and mental changes are both positive and negative changes to the mother when expressing their breast milk. This happens with the routine changes, thus resulting in hormones that affect the emotions and physical changes of the mother. A total of 9 out of 10 studies was discussed on this issue. The most common theme was mental disturbances when expressing breast milk. Some authors mentioned the side effect of improper use of breast pump.
Some mothers viewed expression as a neutral and normal process, and considered expression as an obligation and connection to their infant.10,15 There are mothers who mentioned that providing her infant with milk has allowed her to feel like a mother (i.e. a sense of motherhood).10 They familiarized themselves with expression by recalling their previous experiences and other mothers seemed to welcome pumping sessions as an opportunity for solitude, either from the stressful NICU environment or from their hectic lives.14,15 Anticipation of breastfeeding provided support for milk expression. Furthermore, mothers were satisfied with having provided their babies with the breast milk, as it is a form of immunity to make them (the infant) strong.18
Mothers identified expressing breast milk is not very glamorous routine, pumping as unnatural with analogies from three participants to a dairy farm and are ashamed to express their breast milk using breast pump.10,15,16 Besides that, mothers also experience the feeling of failure when they are unable to breastfeed the infant.17 Mothers felt lonely and alienated from other mothers because they were required to express milk instead of proceeding immediately to breastfeeding, causing it to feel unnatural.15 An interview found that a mother complained of being stressful when she has to replace her infant between the breasts with breast pump.11 They felt that expressing breast milk was weird and reported experiencing expression related emotions that hindered success.15 Additionally, mothers also complained of disturbance when expressing their breast milk, causing diminish an exhausting nature of the process and less efficiency.17 Previous research has shown that the effects of treatment and the process of caesarean section cause the mother to feel drowsiness and fatigue, thus disrupting the expressing of breastmilk process at the beginning of birth delivery.14 The authors also found that the lack of preparation for preterm delivery and disruption of plans, as well as concern for their infant's health, job, and finances have distracted mothers from pumping frequently.14
As highlighted by a researcher that separation between mother and their premature infants, introduced more anxiety into an already stressful situation which then posed barriers to their pumping abilities and expressing.10 It is burden because is hard to do expressing the process adds to the stress of the mother who is worried about the condition of the sick child and in the same time need to pump. The separated situation, infant condition increase worries to the mother and expressing process made the mothers’ situation worsened,9,15 Another study found that mothers’ emotional aspect of expressing milk for their infants would increase the factor for the cause of stress.9 This is proven when the mother felt disappointed because she had failed to provide inadequate amount of breast milk even though they have been following advices, hence, becoming stressed out when comparing the EBM volume with another mother's.9 Numerous studies have found the same situation; their expression process was affected by their mood and became worried about the amount of milk supply for their infant.13,15,17,18
Expressing was a frustrating process because the milk was unable to come out properly, leading to mothers blaming themselves for the inadequacies, often crying and feeling depressed.15 Mothers with premature infant are associated with disappointment, defeat, embarrassment, and depression because they cannot provide enough breast milk for their infant.9 Similarly, in a different study reported that mothers were often concerned about exhaustion and were worried about their ability, or rather, their inability to produce adequate amount of milk.10 Throughout this study, mothers felt like a failure when they do not get a lot of milk during the expression.10 Furthermore, a study concluded that expressing breast milk often caused exhaustion to mothers, especially when their baby's demand was increasing.18 As highlighted by another author, maintaining their milk supply is a common worry for most mothers of premature infant and unfortunately, for some mothers, their milk supply does deteriorate.16
Every mother has different stress triggers and coping mechanism when facing difficulties in expressing breast milk. Mothers stated that the pumping process was intrusive, did not reflect how they were expected to feed their infant, and was time consuming.10 Mothers expressed that they felt tired however, motivated by their husband to continue expressing their breast milk.10 In addition, authors used themes of “stressful” and “overwhelming” to explain the situation that describes how a mother is taking away the quality time with others to make sure they achieve the optimal amount of expressed breast milk.9 However, the voices of mother expressed the time consuming factor as a minor problem compared to their infant's situation.9 In China, mothers felt stressed when in-laws expressed their opinions about how she (the mother) should feed the baby and external factors have increased a mother's anxiety and stress levels; some mothers started crying when they are out of control, such as missing the pumping session.11,18
Because of novice expression skills in the first few days, many mothers experienced bruises, skin abrasions or painfulness in establishing milk flow and producing scant amounts of milk. This is evidenced by three studies stating the same finding.10,16,18 Unsolved situations caused mothers to experience complications such as breast engorgement and sore nipple. Experiencing breast engorgement and sore nipples made mothers uncomfortable.10,11,14 Additionally, to ensure that they are comfortable, mothers need a change in their routine and diet.18
Mothers have to deal with time management when expressing their breast milk. Mothers used forms of distractions such as watching the television, reading or playing video games when expressing to overcome boredom and maintain the frequency of expressing breast milk.14 For others who are working, they expressed their concern pertaining to expressing breast milk at workplace.10 Moreover, a study revealed that a mother who had stop providing their expressing breast milk to their premature infant felt a sense of heartbreak and failure.9
Pumping challengesBreast pump is a mechanical device that lactating women use to extract milk from their breasts and it is very helpful for separated mother to ensure successful lactation process. Breast pump is one of the equipment used in the process of expressing breast milk. There are mothers who experience a fun time when using the machine, but there are also mothers who feel otherwise. The most common experience is the mothers’ feelings during the use of breast pump (7 studies), while 4 studies have found that mothers experienced problems while pumping their breast milk.
Mothers are often worried about expressing their breast milk correctly. Hand expressing of breast milk in early postpartum period encouraged milk production but, authors also found that mothers with health-related problem in the early postpartum period are unable to express their breast milk in early delivery, which resulted in several days of no milk expression.14 The expressing breast milk process should be carried out according to the suggested schedule, however, it was found that mothers who do not follow the suggested period faced complications such as breast engorgement.10 The key for successful breast milk expression is stimulating the let-down reflex and some mothers have a let-down reflex when they are only thinking about breast pump.11
They are more comfortable in expressing their breast milk at home compared to at the NICU and they would plan their routine and make sure that they bring the breast pump equipment together if they have to do it outside.13,14 Furthermore, choosing the suitable breast pump is very important because unsuitable pumps would affect the breast milk due to inconsistency pressure to express the milk, user friendly and cause complications.14 In addition, large and out-dated pumping machines can affect the amount of milk and the efficiency of the equipment.15 Because the ward facility for expressing breast milk is more sophisticated, mothers would attempt to fully utilize the breast pump service facility at the NICU and were willing to wait for the pump to be available.15 Some mothers have additional breast pump equipment, but need to be creative to manoeuvre the electric pump and routine, as it is associated to their milk flow and amount.11
Expressing breast milk is a difficult process for mothers who have previously done successful direct breastfeeding. Mothers are always associated with stress and anxiety when planning the pump process, often crying when deciding to complete the task.11 It was found that mothers also experience sore nipples related to pumping weeks after delivery; common issue in early post-partum period.11 Mothers in a study stated a profound dislike of pumping process that involved physical acts of using a breast pump and the lifestyle, on the positive side, they would still continue to provide milk to help their infants.12 Additionally mothers who express their milk using breast pump found it embarrassing and depreciating, less efficient, tiring and would eventually reduce the production of milk.12,17 There are mothers who express their feelings that pumping was intrusive, did not reflect how they were expected to feed their infant, and was time consuming.10 Mothers had also had paradoxical reaction during the expressing process when using breast pump.11 However, there are mothers who still think positively; having the this-is-for-my-baby mentality. Mothers who did not plan to continue breastfeeding their infant were expressed to have less efficient time management.14 For mothers who are eligible for maternity leave, they are forced to enter work within three weeks after delivery and encounter with unfriendly breastfeeding accommodation, including inconvenient time management, lack of privacy during expressing, and minimum outlet for electric pump.14
The impact of motivation factors to mothersInitiating and maintaining lactation is a method used by women to control their emotions to ensure that they can express breast milk. Many factors affect a mother's success during the expressing period. Expressing breast milk reminds a separated mother from her premature infant that she is a mother and a numbers of mothers getting support from the husband, grandparents and nurses to continue to express the milk.18
This encourages the mother to do what the lactation consultants had adviced them to do and mothers get support also tips from others to continue expressing her milk and this helps mothers to improve their skills.9,10 The emotional aspect of expressing milk for their infants could also be motivating and/or the cause of stress, thus leading mothers to set a goal to ensure she continues the expressing of her breast milk.9 For mothers, providing EBM is a contribution that a mother could give to her premature infant because it is deemed to be one of the mother's obligations and keep encouraging herself to continue expressing using various techniques.10–12,15,16 Even though the mother was separated from their premature infant and cannot afford to provide adequate amount of EBM, mother still feels like a mother and they still continue to express because they believe it will help the infant grow; aims to continue exclusive breastfeeding after discharge.10,12 There have been several studies in the literature reporting the mothers also practice expressing as a type of therapy for not being able to be with their premature infant and believe that expressing is a transition process to fully breastfeeding.11,15
Numerous studies have attempted to explain various methods that make mothers motivated to continue expressing their milk and provide positive development that may motivate them to continue providing breast milk. The optimal amount of breast milk enough for their infant makes a mother motivated to continue expressing their milk.15 Using imaginary technique is another approach used by mothers to stimulate breast milk production.11 For the same reason, mothers keep a follow-up on the infant's growth and development to motivate her to continue with the routine.12 The theme “sacrifices” used to explained the willingness of a mother to face difficulties in expressing the milk.9
DiscussionThis systematic review has summarized the published literature evidence on mothers’ perception towards expressing breast milk for their premature infant in the neonatal intensive care unit. This section discusses the results in relation to each focus question. Expressed breast milk is a worldwide practice for sick infant(s) in the NICU and mothers’ perceptions must be revealed to know the condition of the mother who has gone through the expressing process to capture any possible opportunities to improve care and health education programme for premature infant also for the mother. A rigorous review sourced from two databases has resulted in 10 articles related to mothers’ perceptions to the expressing breast milk practice. The results indicate that mothers have engaged in a diversity of insight during practices. With the scope of this review, three themes have emerged: maternal changes, pumping challenges, and motivation factors, which are the three main findings that have been summarized in this systematic literature review.
Socioeconomic and demographic disparities play an important role in breastfeeding behaviours. Several studies have discussed the demographic such as marital status, race, occupation, level of knowledge, and residential area, either urban or rural, that could affect the mental and physical changes as factors for the mother when expressing her breast milk.9,10,12–14,16,18 This is because regular workload and high level of education can make a mother more open to explore and study further about breast milk and breastfeeding.
Mothers also find it easy to find support and additional knowledge for lactation, especially through social media. Distance from home and settlement in either the urban or rural area can be a factor for time management for mothers during the expressing process. Some studies have shown that they also share the same problem as demographic disparity is almost identical. The evidence that17 associated with10 found that mothers experience the feeling of being a failure because they are not able to breastfeed the infant or get a lot of milk during the expressing process.
The American Academic of Paediatrics categorizes NICU into the level of care.19 The NICU Levels III and IV are the neonatal intensive care unit and regional neonatal intensive care unit, which provide comprehensive care and complex equipment for sick infants. This level provides intensive care for infants with critical illness and acuteness. In this level, mothers are more concerned about their infant's status and expressing breast milk will add stress to the mother. It was found that the mothers are more concerned for their infant's health, their job and finances are distracting them from pumping frequently.10,14 Single parents have many other factors that can cause mothers’ level of stress to increase and eventually disrupt the process of expressing breast milk.13
One of the important findings from this review that was discussed is the mothers’ physical and mental changes when expressing their breast milk. The studies explained stress and tiredness to being some of the physical and mental changes. Lack of alternatives and support in the early post delivery period can also complicate mothers to start expressing their breast milk. Mothers who receive treatment at the end of pregnancy and early births have caused them unable to start expressing quickly and for this reason, complications such as minimal amount of breast milk and breast engorgement would occur.10,14 The effects of medication and treatment during delivery and pregnancy had caused the disruption in the expressing process.
Currently, mothers tend to use the breast pump and would prepare the equipment before giving birth. However, mothers experience difficulties using the breast pump in the early weeks after delivery because new mothers will need to learn how to use it and the time to sharpen their skills.11,18 Furthermore, the mother relies entirely on the breast pump without applying other techniques to express the breast milk and this caused complications such as pain, breast engorgement, sore nipples, discomfort bruises, skin abrasions, and small amounts of milk.10,14,16
Many steps are taken by mothers to ensure that they can supply enough milk for their premature infant. They will be carrying the equipment every where they go and have extra equipment for easier expressing process.14 The privacy, calmness and comfort have resulted in optimal dose of milk produced, as they are more likely to be pumped at home than in the NICU.13 Additionally, they will use the efficient breast pumping facilities at the NICU because the equipment is more sophisticated and up to date.15 Expressing breast milk is an unnatural process because the use of machine as a baby replacement causes the mother to be slightly depressed and mother undergoes mental and negative thinking, thus disturbing the volume of milk produced.10,11,14,17 The studies also described that mothers surrounded by unsupported and unfriendly breastfeeding environment faced difficulty in expressing their milk, and this will affect the amount of milk produced.10,14
Another pivotal element to discuss is the initiation to expressing breast milk. A few studies were able to locate and address that the positive motivation factor leads to successful breast milk expression. Three of these studies described support from family members and health care providers, including a variety of sources in ensuring that they can maintain lactation.9,10,20 Support from various parties is very important to improve maternal motivation, however, external factors may implicate the mothers’ conditions.9,10 Presence of external factors can affect the motivation—the will start to work early, of being a single mother, having other children, distance from house to the NICU, and others.10 The aim may be beneficial to make sure mothers work to achieve success in breastfeeding, and that the expressing only a transition process.10,15 Many studies found that most mothers believed that providing their expressed breast milk is a contribution for her infant's treatment and one of a mother's obligations.10–12,15 This strategy has helped them to overcome problems and continue expressing her breast milk.
Studies have revealed that there are multiple strategies on how mothers worldwide get the motivation and use it for their benefit. During hospitalization, mothers have a sense of motherhood when expressing her breast milk and it can be a relaxation therapy for them.10,11 The amount of milk, imaginary technique, and following their infant's growth are techniques that can be reasonably recommended as they can make a mother feel more relaxed and encouraged in the breast milk production.11,12,15 On top of that, they are willing to ignore other activities and sacrifice their time and activities for the expressing process.9
Because of the limited source of primary studies, the literature retrieved sources that were 10 years back, but provided views for mothers’ perceptions of EBM. Much still remains unknown about Asian mothers’ perceptions to expressing their breast milk. More research is required to cover this issue, especially in Asian countries with various races. Only one study represents Asian subjects in this review.18 More broadly speaking, future research also needs to be done in different countries and settings to allowed for more combination and comparison of findings to better understand mothers’ perspectives of expressing breast milk for their premature infant in the NICU. Previous studies focused on mothers’ emotion pertaining to expressing their breast milk. Despite that, there are still many areas for experiments still uncovered, such as exploring the experience of a mother handling the EBM, a mother's routine and her relation with contamination risk of EBM. Most current research in this review are fully qualitative study. Future study should consider using more mixed method designs to offer in-depth analysis and detailed explanation on mothers’ perceptions regarding expressing their breast milk.
The author only studied one scope, which is the mothers’ perceptions about expressing their breast milk for their premature infants in the NICU. There are several ways that can be scaled up to expand the study; researching a mother's experience in the handling of expressed breast milk, knowing the difficulty of managing their expressed breast milk and linking those factors with health risks pertaining to premature babies. The mother's experience in finding solutions for the inadequate EBM supply can also be highlighted for future studies.
There are some findings from authors who have reported the adverse effects of using breast pump, especially in the early period of its usage. Future research on breast pump needs to explore more closely on the mother's knowledge of breast pump. This allows researchers to know their actual problem in managing the breast pump equipment optimally. This field is also suitable to be done using the mixed method research that combines qualitative and intervention studies.
Most recent research in this review reveals that the mother herself, and family members, are an important factor in influencing her to express breast milk better, or vice versa. Nowadays, the use of an Android phone is a necessity and the influence of social media can be one of the factors that can influence the level of motivation of the mother and this can be proven by future research.
ConclusionThis systematic review has highlighted the mothers’ perceptions in expressing breast milk. Globally, expressing breast milk for their infant in the NICU changes the mothers, mentally than physically speaking. They also face some issues during the handling of breast pump. In response towards this, mothers build up their positive thinking and look for motivation and support.
The review suggests several recommendations for future studies from methodology and empirical views. Firstly, future study should consider mixed method designs to offer in-depth analysis and detailed explanation on mothers’ perception regarding expressing breast milk. Further study should also be done in different countries and settings, consenting combination and made in comparison of its findings to better understand the mothers’ perspectives of expressing breast milk for their premature infant in the NICU. Secondly, to solve the empirical gap, future study should explore more about handling EBM, specifically in handling EBM and related to current issues such as contamination of EBM, donor and exclusive breastfeeding. Thirdly, to explore more about the systematic literature review method for guide research synthesis in context of expressed breast milk and to practice complimentary searching techniques such as citation tracking, reference searching, snowballing, and contacting experts.
Conflict of interestsThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.