Stenosis of the pancreaticodigestive anastomosis (pancreaticogastrostomy and pancreaticojejunostomy) is a very rare complication that usually develops several years after pancreaticoduodenectomy (PD). Only a few cases have been previously reported. We have reviewed the literature and present 2 more cases of pancreaticojejunostomy stenosis that started with episodes of recurrent acute pancreatitis 6 years and 1 year after PD, respectively. Diagnosis was based on symptoms of pancreatitis (12–15 episodes between 5 and 20 months after PD) and CT and MRI scans. Both patients were treated by resection of the pancreaticojejunostomy stenosis, including a 1-cm slice of pancreatic parenchyma in contact with the jejunum, followed by a new well-vascularized two-layer end-to-side PJ with external drainage of the Wirsung duct. Catheter drainage was exteriorized through a jejunal limb using the Witzel technique. Postsurgical course was uneventful in both cases, and after a follow-up period of 3 and 2.5 years, respectively, the patients remain asymptomatic but with endocrine and exocrine insufficiency. Resection of the PJ and construction of a new PJ with external stent drainage of the Wirsung duct is our preferred surgical option in the rare cases of PJ stenosis after a Whipple procedure.
Las estenosis anastomóticas pancreato-digestivas posduodenopancreatectomía cefálica (DPC) son complicaciones raras que suelen presentarse a largo plazo. Presentamos 2 casos de estenosis pancreato-yeyunal que comenzaron con un cuadro clínico de pancreatitis recurrente. El diagnóstico se realizó por clínica de pancreatitis (15 episodios en el primer caso con inicio del primero a los 6 años de la DPC; y 12 episodios en el segundo caso con inicio del primero al año de la DPC), tomografía axial computarizada y resonancia magnética. Ambas pacientes se trataron mediante resección de la anastomosis pancreato-yeyunal, incluyendo un margen de parénquima pancreático de 1cm en contacto con el asa yeyunal, seguida de una nueva pancreato-yeyunostomía término-lateral biplano, con tutorización externa del conducto de Wirsung. El posoperatorio cursó sin incidencias en ambos casos, y tras un periodo de seguimiento de 3 y 2.5 años, respectivamente, las pacientes permanecen asintomáticas, salvo con insuficiencia endocrina y exocrina evidenciadas antes de la reintervención. La reconstrucción de la anastomosis pancreato-yeyunal con drenaje externo del Wirsung es opción válida para tratar los casos de estenosis pancreato-yeyunal post-DPC.
Pancreaticoduodenectomy (PD) is the treatment of choice in patients with cancer of the pancreas, duodenum, periampullary area or distal bile duct, as well as in cases of intraductal papillary mucinous neoplasms (IPMN) of the pancreas. Both pancreaticojejunostomy (PJ) and pancreaticogastrostomy (PG) can be used in the reconstruction after PD. In the last 20 years, high volume HBP surgery centers have published postoperative mortality rates of less than 5%,1–3 with morbidity rates between 46% and 58.5%2,3 and 5-year actuarial survival rates between 15% and 25% after PD due to malignant disease.4–6 The most frequent post-PD complications are pancreatic fistula, hemorrhage and pancreatitis. Stenosis or obstruction of the pancreatico-digestive anastomosis (PJ or PG) is an extremely rare complication, which usually develops years after the PD. To date, only a few cases of this complication have been reported.7–12 After 210 cases of PD performed at our hospital in the last 10 years, we present 2 cases of PJ stenosis after PD, treated by limited resection of the stenotic area and subsequent reconstruction using PJ anastomosis and external pancreatic duct catheter. We will also review the few cases published to date.
Surgical TechniqueCase 1A 66-year-old woman had been diagnosed with symptomatic cholelithiasis, and open cholecystectomy was performed in 1996. Three years later, she presented multiple episodes of acute pancreatitis secondary to choledocholithiasis and stenosis of the sphincter of Oddi and the Wirsung duct, which were treated with double transduodenal sphincteroplasty and pancreatic duct plasty. In February 2007, the patient developed an IPMN with high-grade dysplasia, treated with pylorus-resecting PD. After PD, the reconstruction was performed with a two-plane, end-to-side, duct-to-mucosa, pancreaticojejunal anastomosis (internal with 6/0 polyglyconatei interrupted stitches and external also with 4/0 polypropylene interrupted stitches) with an internal tube. The hepatojejunal anastomosis was performed 17cm away from the pancreatic anastomosis, in an end-to-side position with interrupted 6/0 polyglyconate stitches, ending with the transmesocolic, end-to-side, gastrojejunal anastomosis 55cm away from the biliary, in 2 planes (internal with continuous polyglyconate 3/0 suture and external with continuous polypropylene 4/0 suture). The pathological study of the piece determined it was an IPMN with high grade dysplasia (carcinoma in situ).
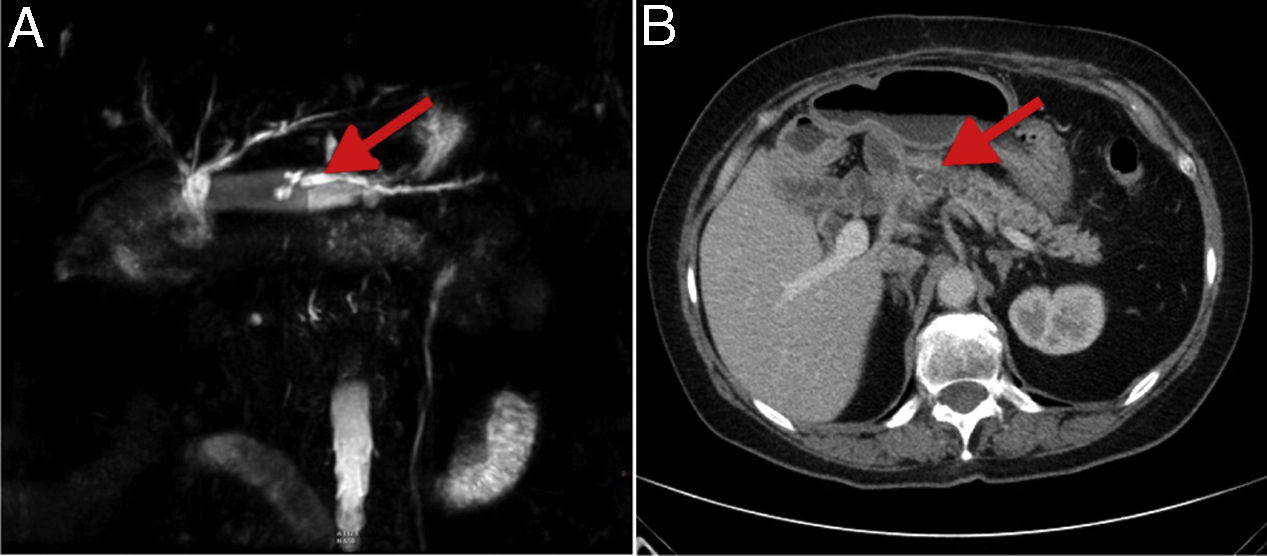
The postoperative period was uneventful, except for the presence of endocrine and subsequent exocrine insufficiency. Starting in January 2013, the patient presented 15 episodes of acute pancreatitis, and in November 2014 she was referred to our unit for the first time because of a new episode of pancreatitis. Lab work showed elevated blood glucose (155mg/dL, normal values [nv]: 70–110), serum amylase (300IU/L; nv: 28–100), serum lipase (350IU/L; nv: 12–70) and C-reactive protein (1.40mg/dL; nv: 0.1–0.5). Normal values were found for tumor markers CA 19-9 and CEA, hematology, coagulation, renal function and transaminases. CT and MRI studies showed a dilation of the pancreatic duct measuring 0.6cm (Fig. 1), although no endoscopic ultrasound was performed. After 2 failed attempts at ERCP, surgical exploration was conducted to treat the anastomotic stenosis. After the dissection, the PJ anastomosis was undone, the dilatation confirmed (diameter 0.6cm), and the Wirsung obstruction was treated by washing the detritus and extracting the calculi. We performed a transversal resection of a 1cm segment of pancreatic parenchyma that was in contact with the jejunal loop; intraoperative histology examination of the piece ruled out malignancy.
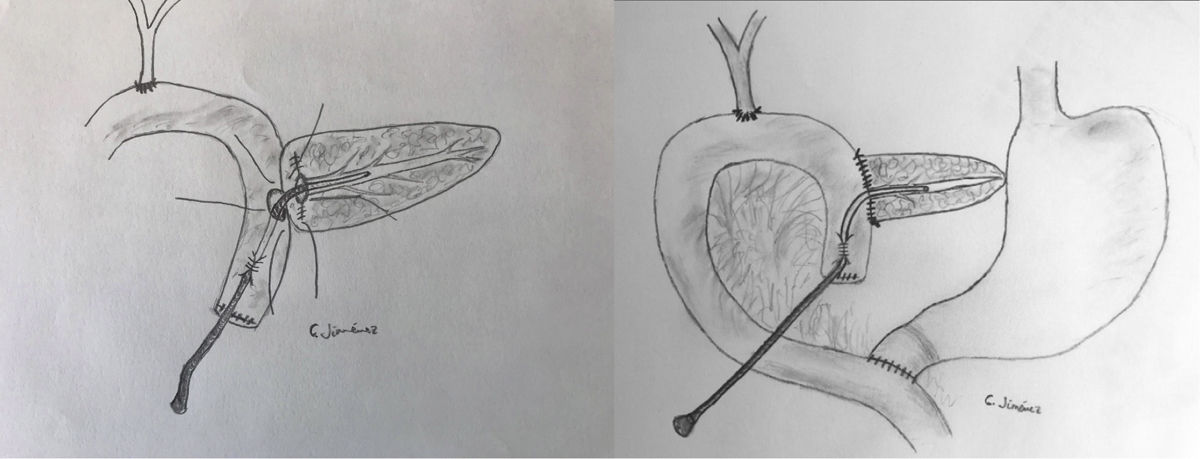
Both in this case and in Case 2, the distance between the pancreaticojejunal and the biliary-jejunal anastomoses was about 15–17cm, which allowed us to resect the jejunal loop attached to the pancreas and perform a new pancreatic-jejunostomy comfortably, without interfering with the biliary-jejunal anastomosis created in the previous intervention. The placement of the external tube was free of technical problems.
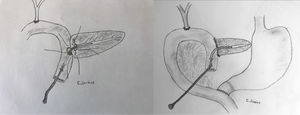
The pancreaticojejunostomy was performed in 2 planes: in the internal plane, suturing the Wirsung mucosa to the jejunal mucosa with 6–8 interrupted stitches of absorbable monofilament material (6-0 polyglyconate), and in the external plane with interrupted 4-0 polypropylene stitches. The end of the transanastomotic catheter was inserted about 3–3.5cm into the pancreatic duct, passing into the jejunal lumen and then later becoming externalized through the ascended proximal jejunal loop. The tube was affixed by following the Witzel technique (Fig. 2). The distal end of the catheter was externalized through the left anterior abdominal wall, where it was attached with silk stitches. The postoperative period transpired without incident, and the catheter was withdrawn 5 weeks after surgery. Three years after the operation, the patient remains asymptomatic, requiring only therapy with oral antidiabetic drugs and pancreatic enzyme replacement due to exocrine insufficiency.
Case 2In 2013, a 45-year-old woman was treated at another hospital for IPMN of the pancreas with pylorus-resecting PD. The surgical and reconstructive technique (pancreatic, biliary and gastric) was the same as in the first case. One year after PD, the patient presented an initial episode of pancreatitis, and these episodes started repeating more frequently (12 episodes of pancreatitis in 5 months). Six attempts at ERCP treatment were unsuccessful, and the patient was referred to our hospital in a situation of endocrine and exocrine insufficiency. Lab work showed normal results for blood count, coagulation, liver and kidney function tests, glycemia and tumor markers. Both CT and MRI scans showed mild dilation of the entire pancreatic duct (diameter 0.4cm), with no lithiasis (Fig. 1). With the diagnosis of PJ stenosis, the patient was reoperatedi, confirming the obstruction of the PJ. The area of anastomotic stenosis was resected, including a 1cm transversal segment of pancreatic parenchyma (intraoperative confirmation of no malignancy); a new two-plane anastomosis was created with an external tube in the Wirsung duct, using the same technique as in the first case. The postoperative period was uneventful, and the tube was withdrawn 5 weeks later. The patient remains asymptomatic 2.5 years after surgery, except for endocrine and exocrine pancreatic insufficiency, which is being treated.
DiscussionPost-PD reconstruction can be done by PG or PJ. The incidence of stenosis or obstruction of these pancreatico-digestive anastomoses is very difficult to evaluate because many patients undergoing PD due to malignant disease have a very limited survival time to develop the complication. In the published series, which include few cases, the incidence of stenosis was 20% after a mean follow-up of 10.8 years in 5 patients treated with PD and reconstruction with PG,7 while other studies estimate its frequency from 1.9 to 20.9%.10–13 Anastomotic stenosis can be observed as early as 1–2 weeks post-PD, and in this case be attributed to inflammation, fibrosis or pancreatic fistula9,14; meanwhile, other patients with pancreatico-digestive stenosis may remain asymptomatic15 or may show episodes of recurrent pancreatitis and/or exocrine pancreatic insufficiency.9 The time elapsed between PD with pancreatico-digestive anastomosis until the onset of stricture-related symptoms varies between one and 9 years.9 Previously published cases showed patients with clear signs of recurrent pancreatitis or simply recurrent abdominal pain.9,10,12 Our 2 cases had presented 15 and 12 episodes of pancreatitis, respectively, during a period of 20 and 5 months.
The permeability and functionality of PJ1–3 has been demonstrated by secretin-enhanced pancreatic MRI in 71% of cases.13 In our experience, PJ stenosis is suspected in recurrent episodes of pancreatitis and is confirmed by dilation of the pancreatic duct in CT or MRI scans. Likewise, intraoperative wirsungraphy and endoscopic ultrasound can also provide images explaining this complication.8 Endoscopic dilation is the conservative treatment of choice for pancreatico-digestive stenosis, but pancreatic duct catheterization has proven to be complex and does not always resolve the problem, as observed in one case of PG8 and in another case of PJ.9
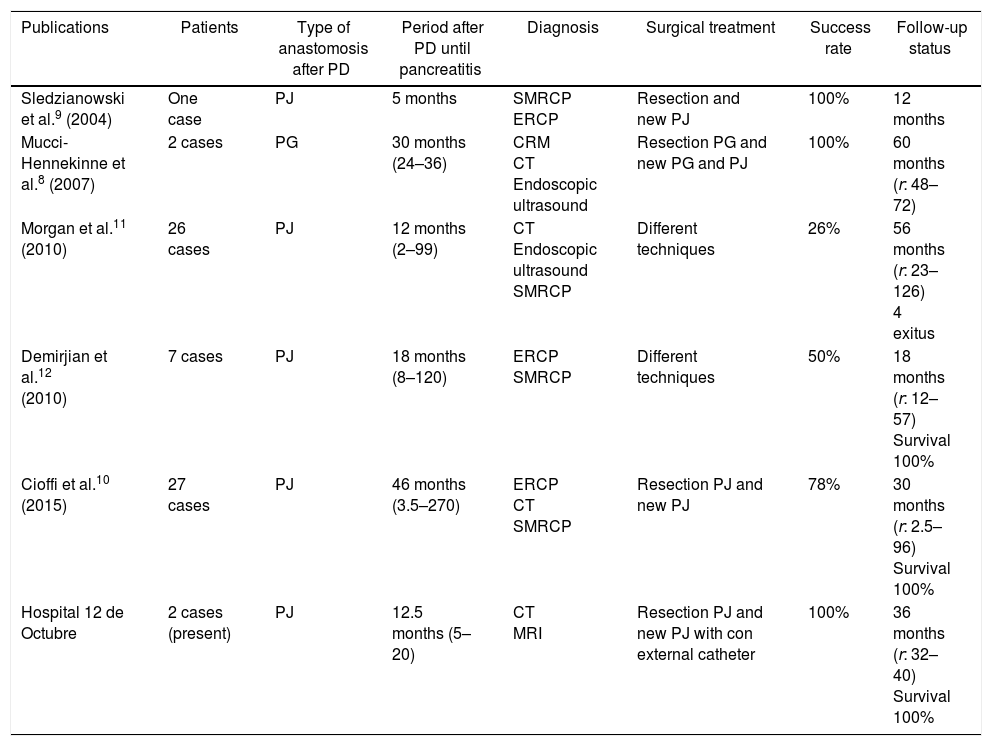
The improvement of pancreatic function and the resolution of abdominal pain due to stenosis or obstruction of the pancreatico-digestive anastomosis can be achieved with the resection of the anastomotic stenosis, including 1cm of pancreatic parenchyma, generally fibrotic, and creating a new PG anastomosis or PJ in cases of previous PG.7,8 A pancreatico-jejunostomy can be performed in cases of Wirsung dilatation with previous stenotic PG.8 As in another recently published case,9 our patients with PJ stenosis were treated by resection of the previous anastomosis and reconstruction with a new PJ. Some authors prefer to perform a modified Puestow procedure in the same intestinal loop.12 Similar to other authors,16,17 to prevent postoperative pancreatic fistula or possible restenosis of the PJ in our 2 cases with dilation of the pancreatic duct, we preferred to perform a duct-to-mucosa, pancreatico-jejunal anastomosis in 2 planes, adding an external catheter for the externalized anastomosis through the afferent jejunal loop, using the Witzel technique. The results of the most important series are shown in Table 1. Our patients did not present postoperative pancreatic fistulae, and after a follow-up period of 3 and 2.5 years, respectively, they remain asymptomatic, requiring only treatment for their pancreatic insufficiency, which they presented before the reoperation.
Characteristics of Published Case Series with Stenosis of the PJ Anastomosis After PD.
| Publications | Patients | Type of anastomosis after PD | Period after PD until pancreatitis | Diagnosis | Surgical treatment | Success rate | Follow-up status |
|---|---|---|---|---|---|---|---|
| Sledzianowski et al.9 (2004) | One case | PJ | 5 months | SMRCP ERCP | Resection and new PJ | 100% | 12 months |
| Mucci-Hennekinne et al.8 (2007) | 2 cases | PG | 30 months (24–36) | CRM CT Endoscopic ultrasound | Resection PG and new PG and PJ | 100% | 60 months (r: 48–72) |
| Morgan et al.11 (2010) | 26 cases | PJ | 12 months (2–99) | CT Endoscopic ultrasound SMRCP | Different techniques | 26% | 56 months (r: 23–126) 4 exitus |
| Demirjian et al.12 (2010) | 7 cases | PJ | 18 months (8–120) | ERCP SMRCP | Different techniques | 50% | 18 months (r: 12–57) Survival 100% |
| Cioffi et al.10 (2015) | 27 cases | PJ | 46 months (3.5–270) | ERCP CT SMRCP | Resection PJ and new PJ | 78% | 30 months (r: 2.5–96) Survival 100% |
| Hospital 12 de Octubre | 2 cases (present) | PJ | 12.5 months (5–20) | CT MRI | Resection PJ and new PJ with con external catheter | 100% | 36 months (r: 32–40) Survival 100% |
PD: pancreaticoduodenectomy; PJ: pancreaticojejunostomy; MRI: magnetic resonance imaging; SMRCP: secretin-enhanced magnetic resonance cholangiopancreatography; CT: computed tomography.
In summary, post-PD pancreaticojejunal stenosis is a rare complication that usually arises in the form of pancreatitis. Our preference is to treat this complication with anastomotic resection and a new PJ, with external drainage of the Wirsung duct.
AuthorshipIago Justo designed the study, Alberto Marcacuzco analyzed the data, Oscar Case conducted the radiological studies, Carlos Jiménez-Romero wrote the first draft of the manuscript. All the authors contributed to the design and interpretation of the study and subsequent revisions. Iago Justo is the corresponding author.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Justo Alonso I, Marcacuzco Quinto A, Caso Maestro O, Jiménez-Romero C. Reconstrucción anastomótica y drenaje externo del conducto de Wirsung como tratamiento de la estenosis pancreato-yeyunal posduodenopancreatectomía cefálica. Cir Esp. 2018;96:648–652.