Herniated thoracic intervertebral disc is a rare cause of spinal cord compression. Its frequency varies from 0.15% to 1.7% of all disc herniations, and produces symptoms in 0.5–0.8%.
Clinical casesCase 1. A 50-year-old woman, with pain and burning sensation in left hemithorax of four months of onset. It was treated as a herpetic syndrome, with no improvement. She was seen after thirteen days of exacerbation of clinical symptoms. The physical examination showed asymmetric paraparesis, lower left pelvic limb 1/5, and right pelvic limb 3/5, sensory level T8, with left Babinski positive. A thoracic disc herniation in space T8–T9 was diagnosed.
Case 2. A 55-year-old patient with a history of presenting pain in lumbar area of 5 years onset. She also had radicular pain that radiated to the right pelvic limb, with intensity 10/10 on a Visual Analogue Scale. Her physical examination showed muscle strength 5/5, with normal sensitivity in all dermatomes and tendon reflexes, and a positive right Babinski. Thoracic disc herniation T7–T8 level was diagnosed.
DiscussionDue to anatomical conditions that define this type of hernia, the extracavitary posterolateral approach should be the recommended surgical procedure when the simultaneously performed anterior decompression and fixation with posterior instrumentation are the treatments proposed.
ConclusionDespite the different anatomical structures of this special area, it was possible to obtain satisfactory results for both clinical cases.
Las hernias de disco intervertebral torácicas son una causa poco habitual de compresión medular. Su frecuencia varía entre el 0.15% al 1.7% de todas las hernias de disco, de las cuales producen síntomas del 0.5% al 0.8%.
Casos clínicosCaso 1. Paciente mujer, de 50 años de edad, que inicia con dolor y ardour en el hemitórax izquierdo de 4 meses de evolución; tratada como cuadro herpético sin obtener mejoría. Acude con 13 días de agudización del cuadro clínico. En el examen físico presentaba paraparesia asimétrica, miembro pélvico inferior izquierdo 1/5 y miembro pélvico derecho 3/5, además de nivel sensorial T8 con Babinski izquierdo positivo. Se diagnosticó hernia discal torácica en el espacio T8-T9.
Caso 2. Paciente mujer de 55 años de edad, con antecedente de presentar dolor en el área lumbar de 5 años de evolución, más dolor radicular que se irradiaba al miembro pélvico derecho, dolor 10/10 en la escala visual análoga; al examen físico: fuerza muscular 5/5, sensibilidad en todos los dermatomos normales, los reflejos eran normales, Babinski derecho positivo. Se diagnosticó hernia discal torácica nivel T7-T8.
DiscusiónPor las condiciones anatómicas en las que se encuentra este tipo de hernia, consideramos que el abordaje posterolateral extracavitario debe ser el procedimiento de elección en situaciones en las que nos proponemos realizar a la vez descompresión anterior y fijación con instrumental posterior.
ConclusiónA pesar de los diferentes aspectos anatómicos que hacen especial esta zona, se logró obtener resultados satisfactorios para ambos casos.
In the differential diagnosis of chest pain, it is important to consider different causes since due to its low incidence thoracic hernia is seldom considered. Hence the importance of presenting these cases so that they can be considered amongst the possible diagnoses, only thus will the appropriate treatment be given.
Thoracic intervertebral disc herniations are a rare cause of spinal cord compression, their frequency varies between 0.15% and 1.7% of all disc hernias, of which from 0.5% to 0.8% produce symptoms. Their highest incidence is in the third to the fifth decade of life and there is no difference as to sex. They are usually unique and the most frequent location is between T9 and T12.1,2
The first case of herniated disc with spinal cord involvement reported in the literature was described by Key3 in 1838. From their origins, these hernias have posed a diagnostic challenge for spinal surgeons, essentially due to the lesion's location, which is often anterior to the spinal cord, and therefore difficult to approach, involving a high neurological risk via the traditional posterior laminectomy route, and the biomechanical concept of vertebral stability. The extracavitary posterolateral approach is a modification of a similar procedure, initially used by Alexander4 and Capener5 for the surgical treatment of tuberculous spondylitis, and is known as costotransversectomy and racotomy (deriving from rachis).
The traditional dorsal laminectomy has become obsolete, and is often contraindicated for pathological processes located ventrally in the spinal canal.6
We used the extracavitary posterolateral approach, also called lateral extrapleural and extraperitoneal approach by Larson,7 to resolve the cases presented. We present our findings below in 2 clinical cases of thoracic herniated discs.
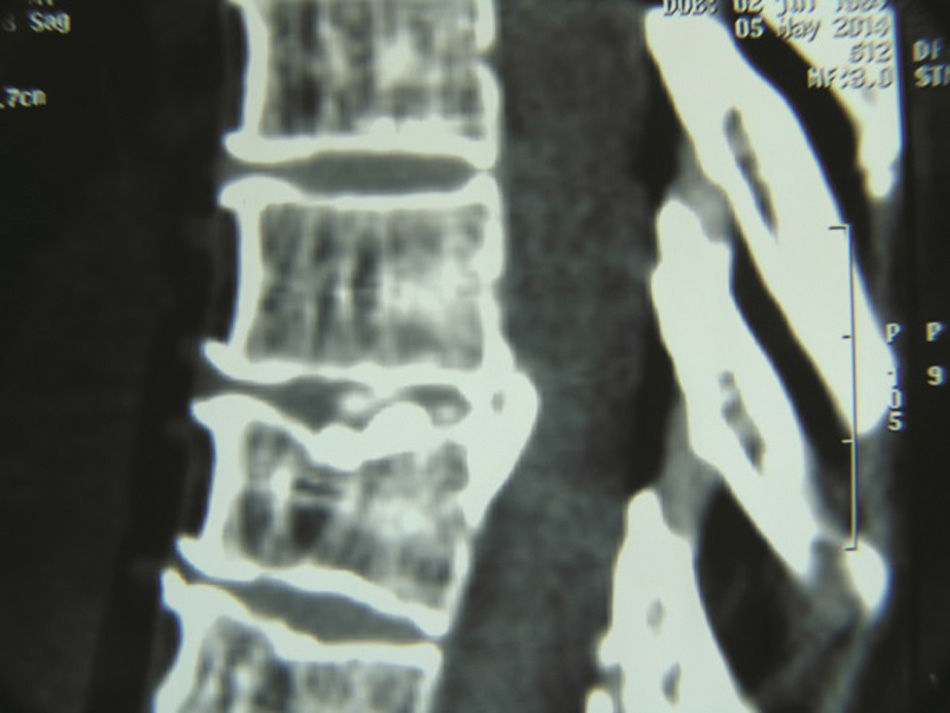
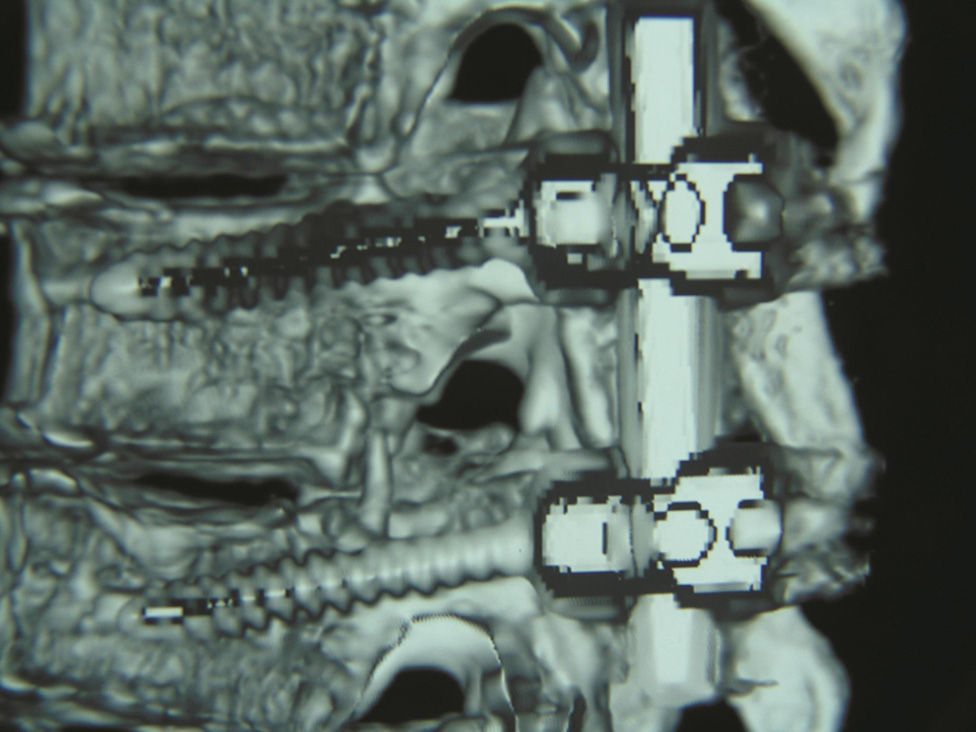
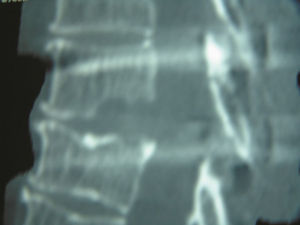
Clinical casesCase 1A 50-year-old female patient with a surgical history of cholecystectomy and personal history of obesity, systemic arterial hypertension, diabetes mellitus and allergy to penicillin. Four months previously, she presented with a 4-month history of pain and burning in the left hemithorax, initially treated as symptoms of herpes, without a satisfactory result, until it became more acute 13 days before she came to our department. She reported that the pain increased on physical exertion, and that she was even unable to walk due to progressive weakness. The patient was admitted and underwent a study protocol with imaging studies, which revealed a herniated disc in the left parasaggital T8–T9 space (Figs. 1 and 2). On physical examination, the patient presented asymmetric paraparesis with left pelvic limb muscle strength 1/5, right pelvic limb 3/5, as well as sensory level T6 with positive left Babinski sign and normal right plantar response to stimulus. Given all the signs found, we decided that the best treatment for this patient was surgery.
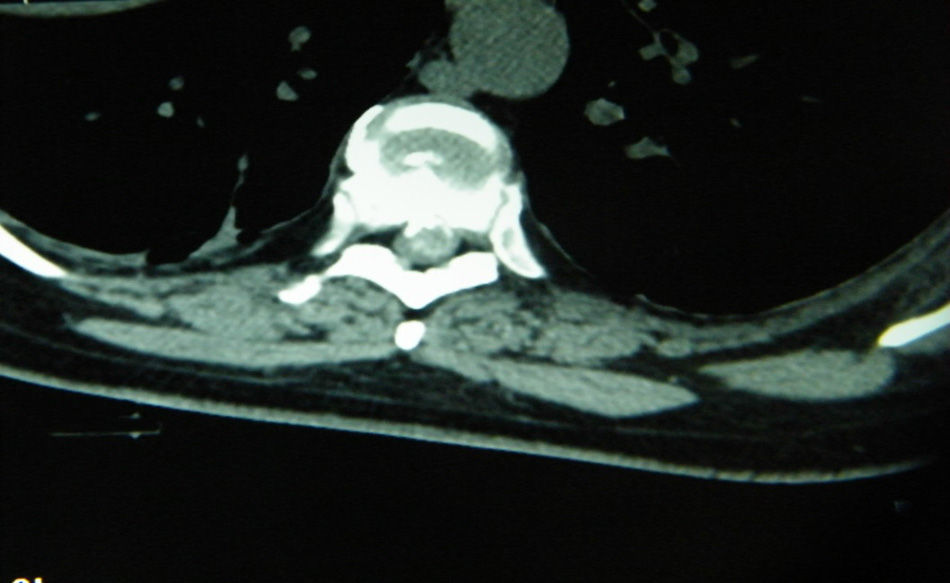
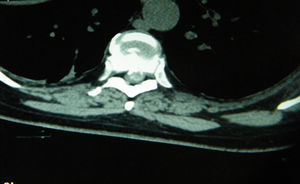
Case 2A 55-year-old female patient, with a five year history of pain in the lumbar region, accompanied by radicular pain radiating to the right pelvic limb, which was 10/10 on the visual analogue scale. Physical examination: muscle strength 5/5, sensitivity in all dermatomes normal, reflexes for L4 and L5 normal, positive right Babinski sign. An imaging protocol was performed and a level T7–T8 herniated thoracic disc diagnosed (Figs. 3 and 4). We concluded that a surgical procedure was necessary.
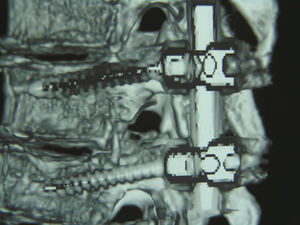
Surgical procedureWe placed the patient in the prone position with lateral supports. We made a hockey stick or capital L shape incision that was approached from the left side. Once the broad flap of skin and subcutaneous tissue were separated, we operated on the fascia and then the paravertebral muscles with a longitudinal incision subperiosteally. Then we made a transverse incision in order to visualise the costotransverse joint, where we then resected the head of rib and partially removed the lamina and the pedicular area, until we came to the dura mater and exposed the herniated intervertebral disc for discectomy. This required a pneumatic burr (Midas Rex® Curved Burr) because it had calcified; however, it was possible to remove it completely with extreme care. We performed all of this under microscope (OPMI Pentero 900) (Fig. 5). In order to provide stability, we placed 2 transpedicular screws (SGL® LFC) together with a rod, all of which were titanium (Fig. 6). Neurophysiological monitoring took place throughout the procedure to check neurological wellbeing.
The patient had a satisfactory postoperative outcome, with improved symptoms and was discharged 48h after surgery with a clean wound.
We reassessed the patient 2 weeks after surgery. She arrived at the department walking with the aid of a frame, we examined her and we found normal sensitivity in all dermatomes examined, apart from T8, where there was dysaesthesia, predominantly left sided in anatomical distribution. With regard to muscle strength, myotomes were evaluated in both lower limbs, finding a right pelvic limb muscle strength of 4/5 and left pelvic member 3/5.
Case 2The patient made satisfactory progress, the Babinski sign and lumbar pain disappeared, and her quality of life improved.
We used the American Academy of Orthopaedic Surgeons’ scale8 for assessment, L4, S1 reflexes were tested and found to be within normal parameters. Babinski sign and clonus were negative.
The patient's satisfaction was evident with regard to her progress after treatment. We assessed the surgical wound, finding no signs of infection and that it was healing well and therefore we removed the sutures without incident. Tomographic checks revealed the success of the technique used, which combined morphological aspects that we observed corresponding directly with the clinical improvement of the patient under study, who had already started physiotherapy and rehabilitation in order to resume her daily activities.
DiscussionOnce a definite diagnosis of herniated thoracic disc has been established, it is time to decide on the best treatment, so that the patient can to benefit from the outcome.9
It is important to remember that herniated thoracic discs are very rare and difficult to diagnose and therefore are a complex problem to treat, and there are anatomical aspects as well that characteristically distinguish the spinal cord from other vertebral regions. Firstly, the greater space occupied by the spinal cord in relation to the size of the spinal canal, although the spinal cord has little volume here. Secondly, the existence of a subarachnoid space that is equally small. Thirdly, the poor blood supply, particularly between T4–T9. These are relevant aspects that should be taken into account when deciding on the appropriate surgical approach. Surgeons have recently become familiar with the thoracoscopic techniques and they are being widely used in different diseases. These techniques are also used in herniated thoracic discs, as they are minimally invasive and obtain good results, and thus have revolutionised the treatment of spinal cord lesions.10
Despite the excellent results achieved with the abovementioned technique, the choice of patient in whom to use the technique is very important. We consider that for our patients in particular, because they had calcification, video-assisted discectomy would have been impossible. Another aspect to bear in mind is the principle of stability, which is often disregarded.
Taking the above into account, we consider that the extracavitary posterolateral approach is the procedure of choice in situations where we want to achieve anterior decompression and subsequent fixation with instruments. In this we agree with Escribano and Clavel11 and other authors.12,13
ConclusionIn patients with pathophysiological characteristics and thoracic herniated disc in a lateral location, the most appropriate approach is posterolateral.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interest to declare.
To Dr Titania Acosta Hernández for her technical support in preparing this document.
Please cite this article as: Picado-Baca ML, Mireles-Cano JN, León-Meza VM, García-González OG, Ramos-Trujillo A. Tratamiento de hernia discal torácica. Reporte de 2 casos. Cir Cir. 2016;84:415–419.