The impact of the COVID-19 pandemic on deaths, sequelae, and excess mortality has been reported. However, fewer reports on hospitalization costs are available, and they usually focus on the average cost for a general ward, the intensive care unit, and the emergency room.1–3 Fewer studies have described possible additional determinants of hospitalization costs.1–5 The main described factors increasing the hospital cost in COVID-19 patients included age, sex, the disease severity, and the presence of comorbidities, in addition to those considered standards such as the length of stay (LoS) in the hospital and the type of ward and support received, being highest in the intensive care unit (ICU), and for those requiring invasive mechanical ventilation (IMV).4–9
Hospitalization costs have a wide variability at the international level; the highest average costs have been reported in Saudi Arabia ($11,849) and the United States (U.S.) ($11,267 and 24,571).2,3,10 In Ethiopia and China ($1453–$6827), the lowest mean costs have been reported so far.4,5,11,12 Stratifying by severity, in Kenya, the average costs of severe and critical cases were USD 1949 and USD 7194, respectively.13 In Brazil, a mild case was estimated at USD$1975, a severe case USD$11,338, and a death in $12,993.1 In European studies, diabetes mellitus and obesity were positively associated with hospitalization costs in COVID-19 patients.14,15
Regarding the clinical determinants, age increased the mean cost by 0.9–85%, the length of stay by 4.7–4.9%, and the mechanical ventilation by 25% or up to 2.7 times.4,5,8 Likewise, the number of comorbidities increased the costs between 11 and 24%.8
In Mexico, 7.63 million confirmed cases of SARS-CoV-2 were registered until June 2023, of which 9.57% required hospitalization. The present study was conducted at the Instituto Nacional de Enfermedades Respiratorias “Ismael Cosío Villegas” in Mexico City. This is a national-reference public hospital for treating respiratory diseases and mainly uninsured patients. Each ward bed was equipped with a ventilator during the pandemic, and medical personnel equivalent to an intensive care unit were assigned. There were 255 beds with these features. Our objective was to determine the effect of clinical factors on the direct costs of care of adult patients hospitalized for COVID-19.
We collected clinical and cost data for each patient (age ≥18 years old) between March 2020 and August 2021. All patients underwent a PCR test to confirm SARS-Cov-2 infection. This study was submitted to the hospital ethics committee, and approval number E05-20 was obtained.
Clinical information was obtained through the electronic file. It included sex, age, length of stay, number of comorbidities, healthcare-associated infections (HCAIs), the severity of acute kidney injury (AKI), death, the type of support received: invasive mechanical ventilation (IMV), high-flow oxygen therapy, administration of antibiotics, antihypertensives and vasopressors. The severity of acute kidney injury was determined using the Kidney Disease Improving Global Outcomes (KDIGO) criteria.16 We used the maximum level of severity during hospitalization for the analysis.
The health economics department provided the unit prices and quantities of the supplies used for each patient. We multiplied the quantity of each input by its unit price and summed all the results to obtain the total cost of each hospitalization. All costs were transformed into 2023 U.S. dollars using an exchange rate of 18.55 pesos per dollar.
The hospital perspective was used to perform the analysis stratifying by sex and death. We estimated the median (P25–P75) and mean (S.D.) total hospitalization costs for each clinical characteristic considered in the study. Generalized linear models were fitted using a gamma distribution and the identity as link function. The models allowed us to estimate the average increase in hospitalization costs (coefficients) and the marginal effects (average adjusted costs) for each variable included. The analysis was performed using STATA v12 statistical software (Stata Corp., College Station, TX, USA).
Table S1 describes the clinical characteristics of the patients. Briefly, 3055 adult patients were included, 65.5% were men. Women were older than men. Sixty-two percent of the patients acquired a healthcare-associated infection, and 18.9% suffered from severe acute kidney injury. Antibiotics, antihypertensives, and vasopressors were administered in 74.4, 65.6 and 14.9% of patients. Invasive mechanical ventilation was required in 63.5% of patients, and high-flow oxygen therapy was required in 33.6%.
The median (p25–p75) days of hospitalization for all patients was 16 (10–26), for women was 15 (9–25), and for men was 17 (10–27) (Table S2). The average (S.D.) observed hospitalization cost was $16,985 ($17,697) for all patients, for women was $14,996 ($14,537), and for men was $18,011 ($19,046) (Table S3).
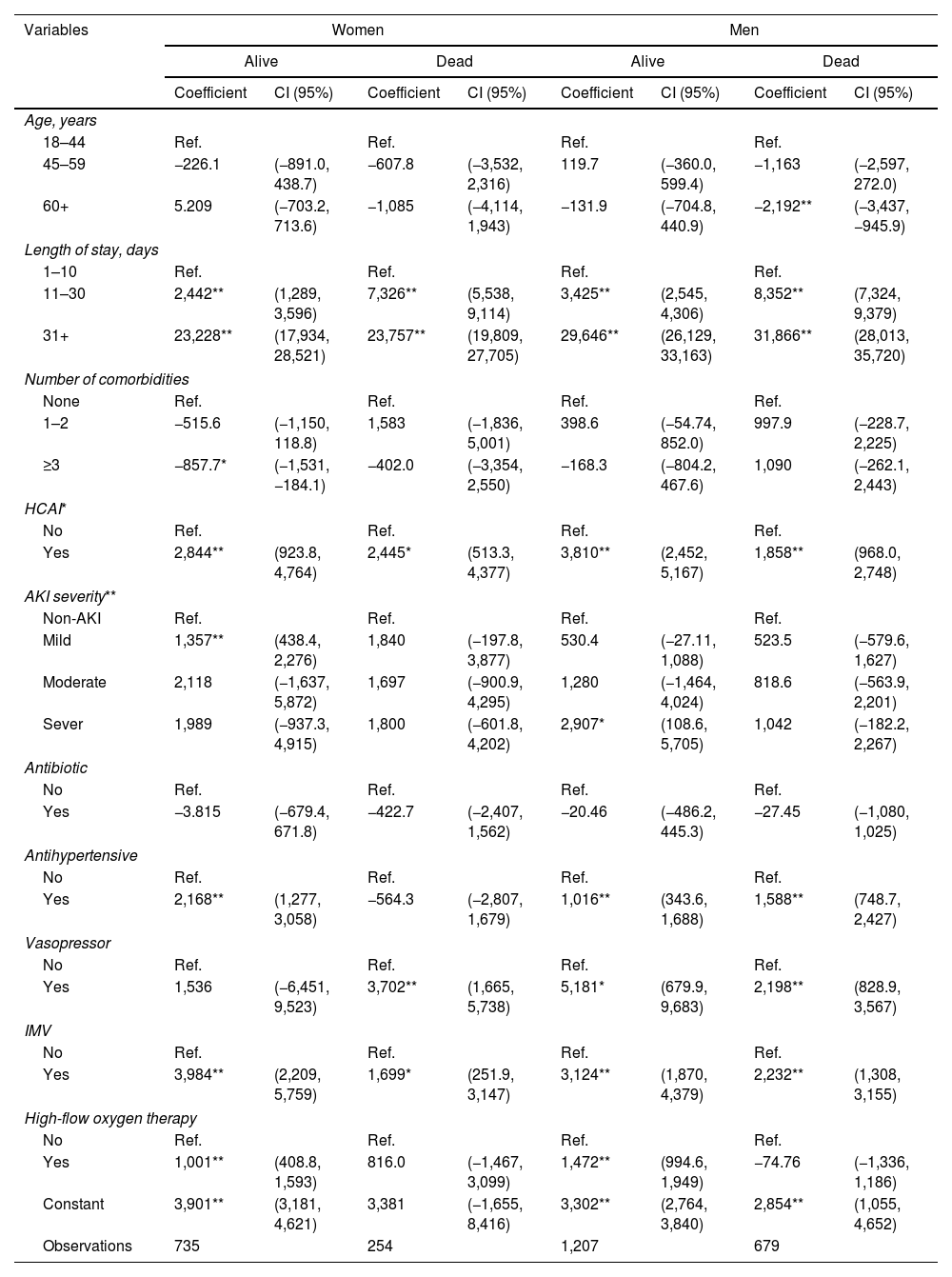
According to the generalized linear models, the LoS, IMV, and HCAIs significantly impacted costs in all patients. AKI severity, antihypertensive, and high-flow oxygen therapy were significant in alive patients, while non-survivors were vasopressors (Table 1).
Multivariate Models for Determinants of Hospitalization Costs in COVID-19 Patients.
| Variables | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| Alive | Dead | Alive | Dead | |||||
| Coefficient | CI (95%) | Coefficient | CI (95%) | Coefficient | CI (95%) | Coefficient | CI (95%) | |
| Age, years | ||||||||
| 18–44 | Ref. | Ref. | Ref. | Ref. | ||||
| 45–59 | −226.1 | (−891.0, 438.7) | −607.8 | (−3,532, 2,316) | 119.7 | (−360.0, 599.4) | −1,163 | (−2,597, 272.0) |
| 60+ | 5.209 | (−703.2, 713.6) | −1,085 | (−4,114, 1,943) | −131.9 | (−704.8, 440.9) | −2,192** | (−3,437, −945.9) |
| Length of stay, days | ||||||||
| 1–10 | Ref. | Ref. | Ref. | Ref. | ||||
| 11–30 | 2,442** | (1,289, 3,596) | 7,326** | (5,538, 9,114) | 3,425** | (2,545, 4,306) | 8,352** | (7,324, 9,379) |
| 31+ | 23,228** | (17,934, 28,521) | 23,757** | (19,809, 27,705) | 29,646** | (26,129, 33,163) | 31,866** | (28,013, 35,720) |
| Number of comorbidities | ||||||||
| None | Ref. | Ref. | Ref. | Ref. | ||||
| 1–2 | −515.6 | (−1,150, 118.8) | 1,583 | (−1,836, 5,001) | 398.6 | (−54.74, 852.0) | 997.9 | (−228.7, 2,225) |
| ≥3 | −857.7* | (−1,531, −184.1) | −402.0 | (−3,354, 2,550) | −168.3 | (−804.2, 467.6) | 1,090 | (−262.1, 2,443) |
| HCAI* | ||||||||
| No | Ref. | Ref. | Ref. | Ref. | ||||
| Yes | 2,844** | (923.8, 4,764) | 2,445* | (513.3, 4,377) | 3,810** | (2,452, 5,167) | 1,858** | (968.0, 2,748) |
| AKI severity** | ||||||||
| Non-AKI | Ref. | Ref. | Ref. | Ref. | ||||
| Mild | 1,357** | (438.4, 2,276) | 1,840 | (−197.8, 3,877) | 530.4 | (−27.11, 1,088) | 523.5 | (−579.6, 1,627) |
| Moderate | 2,118 | (−1,637, 5,872) | 1,697 | (−900.9, 4,295) | 1,280 | (−1,464, 4,024) | 818.6 | (−563.9, 2,201) |
| Sever | 1,989 | (−937.3, 4,915) | 1,800 | (−601.8, 4,202) | 2,907* | (108.6, 5,705) | 1,042 | (−182.2, 2,267) |
| Antibiotic | ||||||||
| No | Ref. | Ref. | Ref. | Ref. | ||||
| Yes | −3.815 | (−679.4, 671.8) | −422.7 | (−2,407, 1,562) | −20.46 | (−486.2, 445.3) | −27.45 | (−1,080, 1,025) |
| Antihypertensive | ||||||||
| No | Ref. | Ref. | Ref. | Ref. | ||||
| Yes | 2,168** | (1,277, 3,058) | −564.3 | (−2,807, 1,679) | 1,016** | (343.6, 1,688) | 1,588** | (748.7, 2,427) |
| Vasopressor | ||||||||
| No | Ref. | Ref. | Ref. | Ref. | ||||
| Yes | 1,536 | (−6,451, 9,523) | 3,702** | (1,665, 5,738) | 5,181* | (679.9, 9,683) | 2,198** | (828.9, 3,567) |
| IMV | ||||||||
| No | Ref. | Ref. | Ref. | Ref. | ||||
| Yes | 3,984** | (2,209, 5,759) | 1,699* | (251.9, 3,147) | 3,124** | (1,870, 4,379) | 2,232** | (1,308, 3,155) |
| High-flow oxygen therapy | ||||||||
| No | Ref. | Ref. | Ref. | Ref. | ||||
| Yes | 1,001** | (408.8, 1,593) | 816.0 | (−1,467, 3,099) | 1,472** | (994.6, 1,949) | −74.76 | (−1,336, 1,186) |
| Constant | 3,901** | (3,181, 4,621) | 3,381 | (−1,655, 8,416) | 3,302** | (2,764, 3,840) | 2,854** | (1,055, 4,652) |
| Observations | 735 | 254 | 1,207 | 679 | ||||
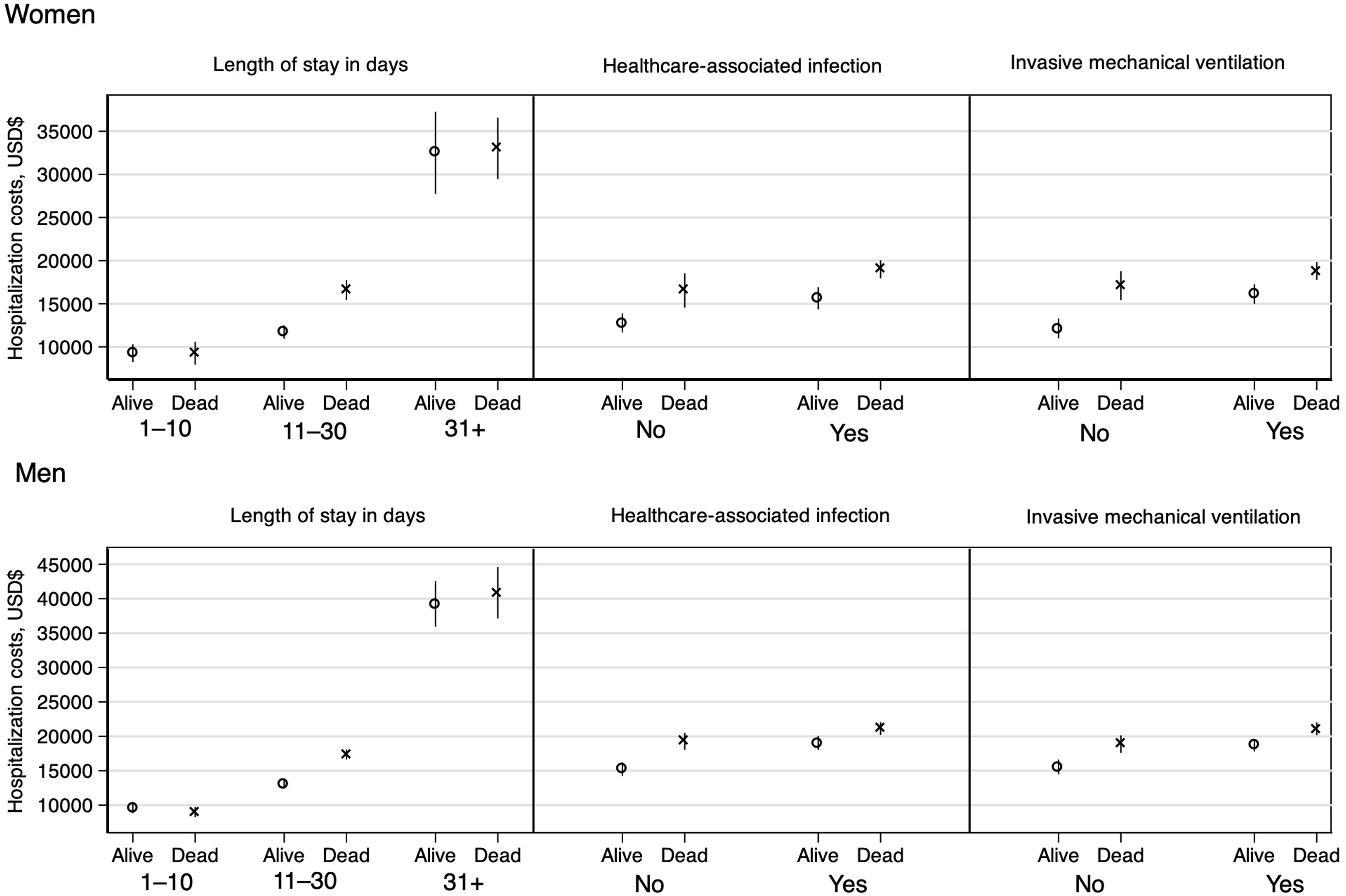
The mean of adjusted hospital costs was higher when the days of hospital stay increased, with healthcare-associated infection and invasive mechanical ventilation regardless of sex and death (Table S4 and Fig. 1).
Previously, the main clinical characteristics determining the costs of hospitalization for COVID-19 were age, the number of comorbidities, the number of days of hospital stay, and the presence of mechanical ventilation.4,5,8 In this study, the associated factors to higher cost were the length of stay, the healthcare-associated infections, and the invasive mechanical ventilation in all patients. However, specific determinants depended on sex and mortality.
The length of stay significantly impacted adjusted average costs ($8,988–$40,854) over any other clinical characteristic. A study in China described that one additional day of hospitalization increased hospital costs by 4.5%.4 However, the stay in the intensive care unit was the factor that most increased hospitalization costs. In our study population, the median (p25–p75) of LoS was 16 (10–26) without considering any stratification, similar to studies where severe and critical patients were included.4,5
In our population, 63.5% of the patients required invasive mechanical ventilation, which indicates the severity of the patients attended worsened due to altitude-related hypoxemia. The median costs of ventilated patients ranged from $16,121 to $21,089, while other studies have reported costs ranging from $9268 to $25,068.2,4,5 This difference may be because the studies have included public and private hospitals. On the other hand, the impact of nosocomial infections as a determinant of hospitalization costs has not been evaluated to date. Healthcare-associated infections increased costs in the range of $1858–$3810; these patients had stays two to four times longer than those without infection.
This study has the following limitations: first, the patients were recruited in only one public tertiary care center from Mexico City. Second, in our analysis, indirect costs were not considered. Third, we should have included the cost of the emergency equipment acquired as preparation for the pandemic used during the hospital conversion, which may lead to an underestimation of costs. Nevertheless, our results may shed more specific light on the factors determining the costs of hospitalization of patients hospitalized for SARS-CoV-2.
In conclusion, the length of stay, healthcare-associated infections, and invasive mechanical ventilation could increase hospitalization costs for COVID-19 patients.
FundingNone declared.
Conflicts of InterestNone declared.