A 68-year-old male presented with flu-like symptoms, fatigue, history of obesity, hypertension, type 2 diabetes and chronic smoking. Chest radiography revealed right basal opacity consisting of infiltrate. With respiratory failure, orotracheal intubation and mechanical ventilation were performed. Patient presented gas exchange alteration. Real-time PCR detected SARS-CoV-2. Treatment with liponavir/ritonavir and hydroxychloroquine was started. Because of poor acoustic window, speckle-tracking transoesophageal echocardiography (TEE) was performed, detecting deterioration in global longitudinal strain. Acute COVID 19 infection led us to suspect myocarditis, with no other signs or symptoms other than elevated troponin and altered strain. On day 15, the patient suffered bacteraemic sepsis at endovascular focus with Serratia marcescens and multiorgan failure. TEE-guided haemodynamic monitoring was repeated showing global longitudinal strain improvement. Acute COVID 19 infection led us to suspect myocarditis, with no other signs or symptoms beyond elevated troponin and altered strain.
Un hombre de 68 años presentó síntomas similares a los de la gripe, fatiga, antecedentes de obesidad, hipertensión, diabetes de tipo 2 y tabaquismo crónico. La radiografía de tórax reveló una opacidad basal derecha consistente con infiltración. Se realizó una intubación orotraqueal y ventilación mecánica. El paciente presentó alteración del intercambio gaseoso. La PCR en tiempo real detectó SARS-CoV-2. Se inició el tratamiento con liponavir/ritonavir e hidroxicloroquina. Debido a la deficiente ventana acústica, se realizó una ecocardiografía transoesofágica (ETE) de speckle-tracking, que detectó el deterioro de la tensión longitudinal global. La infección aguda por COVID 19 nos llevó a sospechar de miocarditis, sin más signos o síntomas que la elevación de la troponina y la alteración de la cepa. El día 15, el paciente sufrió una sepsis bacteriana en el foco endovascular con Serratia marcescens y fallo multiorgánico. Se repitió la monitorización hemodinámica guiada por ETE que mostró una mejora en la tensión longitudinal global.
The novel coronavirus disease (COVID-19) has been spreading exponentially in most countries around the world. Its clinical course is characterized by respiratory tract symptoms.1 However, COVID-19 also affects multiple organs and acute myocarditis has been described as an associated complication.2 Haemodynamic monitoring is important in the recovery process. Bedside transthoracic echocardiography (TTE) may be insufficient due to deficient acoustic window or suboptimal views when using positive end-expiratory pressure in mechanically ventilated patients.3–6 Strain imaging using speckle-tracking TEE could play a crucial role because of its greater sensitivity for the early diagnosis of myocarditis associated to COVID-19 in critically ill patients. We present a patient with COVID-19 whose myocardial deformation was detected using myocardial strain speckle-tracking by TEE.
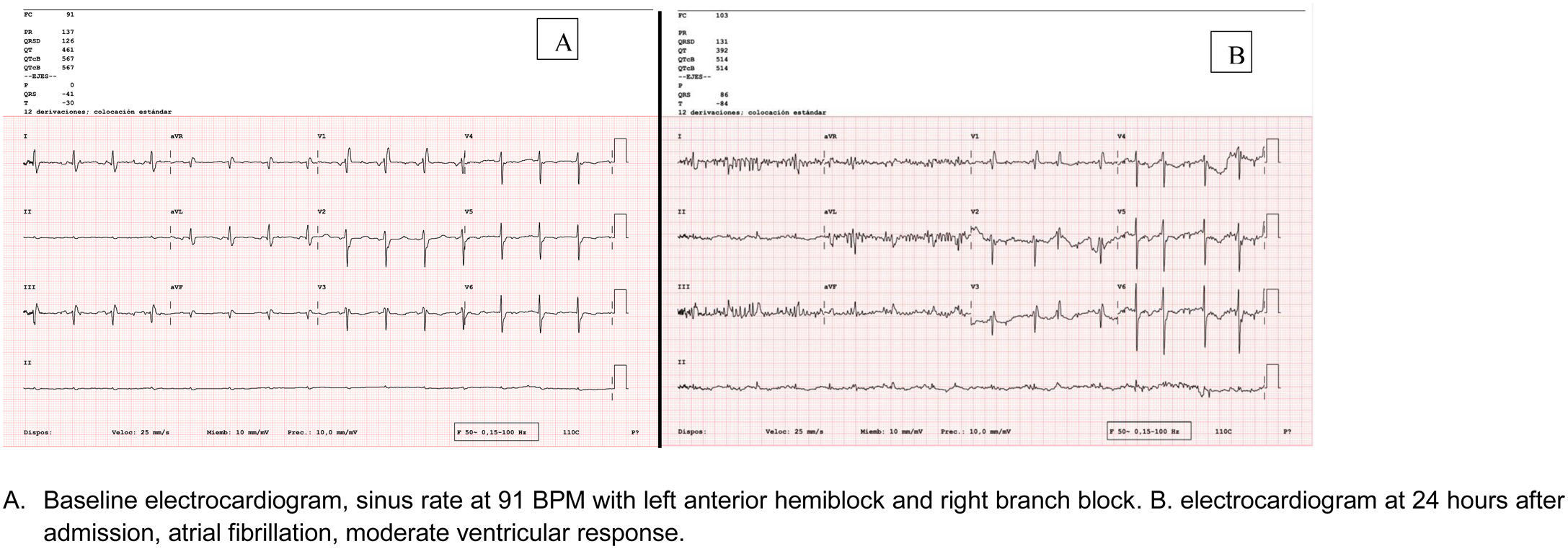
A 68-year-old male presented to the emergency department with a complaint of flu-like symptoms for the previous ten days and fatigue that had worsen in the previous hours. The patient had a history of obesity (BMI 33kg/m2), hypertension (treated with amlodipine 10mg/day and enalapril 10mg/day), type 2 diabetes (treated with empagliflozine), and chronic smoking (40 pack-year). An echocardiogram in September 2019 had shown normal biventricular size and function. When admitted to intensive care unit with acute respiratory failure, the patient presented an APACHE II of 8, a SAPS II of 18 and a SOFA of 3. Electrocardiograms at day 1 and 2 are shown in Fig. 1.
The patient required oxygen therapy at 2L/min, with adequate ventilatory mechanics, body temperature of 38°C; he was haemodynamically stable and lucid. Laboratory results showed metabolic acidosis and respiratory alkalosis without hyperlactacidemia, creatinine clearance MDRD 62mL/min, preserved leucocyte formula, and a normal hepatogram. Markers were LDH 198UI/l; troponin T 16pg/mL, ferritine 723ng/mL, BnP 370pg/mL; Dimer D 300ng/mL. Chest radiography revealed right basal opacities.
Respiratory sepsis with suspicion of SARS-CoV-2 was deemed as likely; therefore, empirical therapy with ampicillin/sulbactam was started. On day 3, the patient showed a more severe hypoxaemia which required orotracheal intubation and mechanical ventilation. The patient presented with alteration of gas exchange (PaO2/FiO2 167mmHg); so, anaesthesia was maintained with remifentanil (15mcg/kg/h) and propofol (1.42mg/kg/h), RASS target of −5; in addition, neuromuscular blockers (atracurium 1.1mg/kg/h) were indicated. Protective mechanical ventilation was performed with a tidal volume of 6mL/kg of ideal body weight with the following lung mechanic: volume-controlled ventilation 530mL, positive end-expiratory pressure of 10cm H2O, RR of 20rpm, 40% FiO2; plateau pressure of 17cm H2O, driving pressure of 7cm H2O, static compliance 75mL cm H2O. Respiratory filmarray panel detected Coronavirus NL63 and real-time reverse transcriptase-polymerase chain reaction assay detected SARS-CoV-2 in nasal and throat swab sample taken at admission. Treatment with liponavir/ritonavir and hydroxychloroquine was started. Three days later, because of prolonged QTc interval, treatment with antimalarials was discontinued. Due to persistent gas exchange alteration (PaO2/FiO2<150mmHg), the prone position was performed five times with subsequent improvement of PaO2/FiO2 ratio, keeping lung mechanics.
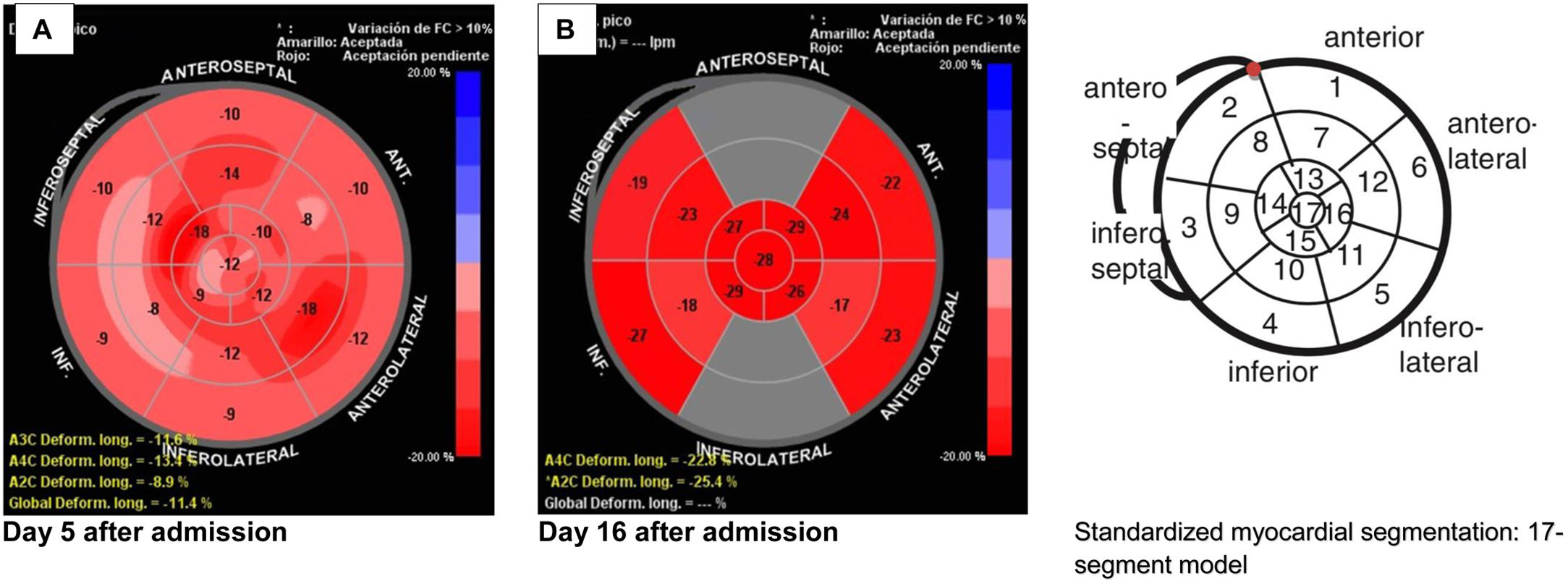
As a result of poor acoustic window, guided monitoring by TEE was performed on day 5, using an CX50 Philips Ultrasound (X7-2t) fitted with a multiplane 2–7MHz TEE transducer, following a standard procedure (Fig. 2), detecting deterioration in global longitudinal strain. Table 1 shows speckle-tracking analysis. Acute COVID-19 infection led us to suspect myocarditis, with no other signs or symptoms other than elevated troponin and the altered strain.
Left ventricle speckle-tracking analysis.
| Segments | Deformation (%)TEE (Day 5) | Deformation (%)TEE (Day 16) |
|---|---|---|
| Segment 13 | −18% | −27% |
| Segment 14 | −9% | −29% |
| Segment 15 | −12% | −26% |
| Segment 16 | −10% | −29% |
| Segment 17 | −12% | −28% |
| Mean apical strain % | −12.2% | −27.8% |
| Segment 8 | −11.7% | −23% |
| Segment 9 | −12% | −18% |
| Segment 11 | −18% | −17% |
| Segment 12 | −8% | −24% |
| Mean medial strain % | −12.4% | −20.5% |
Abbreviation: TEE, transoesophageal echocardiography.
Subsequently, on day 15, the patient suffered bacteraemic sepsis at endovascular focus with Serratia marcescens; therefore, treatment with imipenem depending on sensibility was started. The patient presented multiorgan failure, norepinephrine (0.2mcg/kg/min) was administered; respiratory values were PaO2/FiO2<150mmHg in treatment with protective mechanical ventilation, neuromuscular blocking, and prone position. In addition, haemodialysis was started. TEE-guided haemodynamic monitoring was performed on day 16 (Fig. 2). On day 22, the patient was still in the intensive care unit and has shown two negative tests for COVID-19. Written consent was obtained.
Patients with COVID-19 infection and associated myocardial injury may have an increased mortality compared with patients with normal troponin levels.1,2 Although the diagnosis of myocardial injury still depends on the increase of high-sensitivity troponin t, new cardiac image techniques could show ventricular failure.6–8 In our patient, a pronounced deterioration in both global and segmental longitudinal strain was observed, which was suggestive of acute myocarditis despite the only slight increase in cardiac troponin. We suspected myocarditis as a result of the context of acute COVID-19 infection, increased high-sensitivity troponin T and strain alteration. Although cardiac magnetic resonance imaging (CMRi) and endomyocardial biopsy are the gold standards for the diagnosis of myocarditis, the evidence shows a good correlation between echocardiographic strain and CMRi.9
We routinely screen ventilated patients with echocardiograms, especially in the case of COVID-19 infection, which can affect the cardiovascular system. Because of the impossibility of a good acoustic window by speckle-tracking TEE, the presence of altered strain in the first TEE and the patient's clinical deterioration with significant haemodynamic instability 10 days after the first ultrasound study, the speckle-tracking TEE was repeated. Of note, in the context of COVID-19 and with severe hypoxaemia requiring placing the patient in the prone position, TEE could be performed nonetheless.10 A notable improvement was seen in the global longitudinal strain values without significant changes in cardiac troponin.
In this patient, myocarditis appears to have been a subclinical event; however, myocardial injury cannot be ruled out. Myocarditis was suspected because of acute COVID-19 although the patient only presented increased troponin and an altered strain. Moreover, in the context of acute COVID-19 myocardial assessment in ventilated patients with sedation and analgesia seems to be important due to the prevalence of myocardial dysfunction.
Strain imaging using speckle-tracking TEE is a relatively new tool in ICUs – although not widely available - and evidence suggests that it has better sensitivity than the ejection fraction in assessing myocardial function. Although speckle tracking alterations in this scenario cannot confirm the diagnosis of myocarditis, the literature supports the use of this technique in critical transthoracic echocardiography; in the context of transesophageal echocardiography, results still need to be validated. The need for a good quality image by common two-dimensional ultrasound imagining was met by speckle-tracking TEE. Speckle-tracking echocardiography works as a “digital biopsy” and it could become an essential diagnostic tool for myocarditis and septic cardiomyopathy.11 Understanding atypical presentations and imaging findings could contribute to prompt diagnosis of COVID-19 induced myocarditis.
Financial disclosureThe authors declare no financial interest. No financial support has been received for this study.
Conflict of interestThe authors declare they do not have any conflict of interest.