COPD causes high morbidity and mortality and high health costs. Thus, identifying and analyzing the distinctive and treatable traits seems useful to optimize the management of AEPOC patients. While various biomarkers have been researched, no solid data for systematic use have been made available.
AimAssessing the short-term prognostic usefulness of clinical and analytical parameters available in routine clinical practice in COPD exacerbations.
Material and methodsMulticenter prospective observational study conducted between 2016 and 2018. Patients admitted for COPD exacerbation who agreed to participate and signed an informed consent form were included. Prolonged stay, in-hospital mortality or early readmission was considered an unfavorable progression. 30-Day mortality was also analyzed.
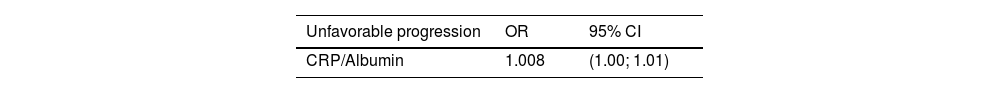
Results615 patients were included. Mean age was 73.9 years (SD 10.6); 86.2% were male. Progression of 357 patients (58%) was considered unfavorable. Mortality at 1 month from discharge was 6.7%. The multivariate analysis shows a relationship between the CRP/Albumin ratio and unfavorable progression (OR 1.008, 95% CI 1.00; 1.01), as well as increased risk of death at 1 month from discharge with elevated urea (OR 1.01, 95% CI 1.005; 1.02) and troponin T (OR 2.21, 95% CI 1.06; 4.62).
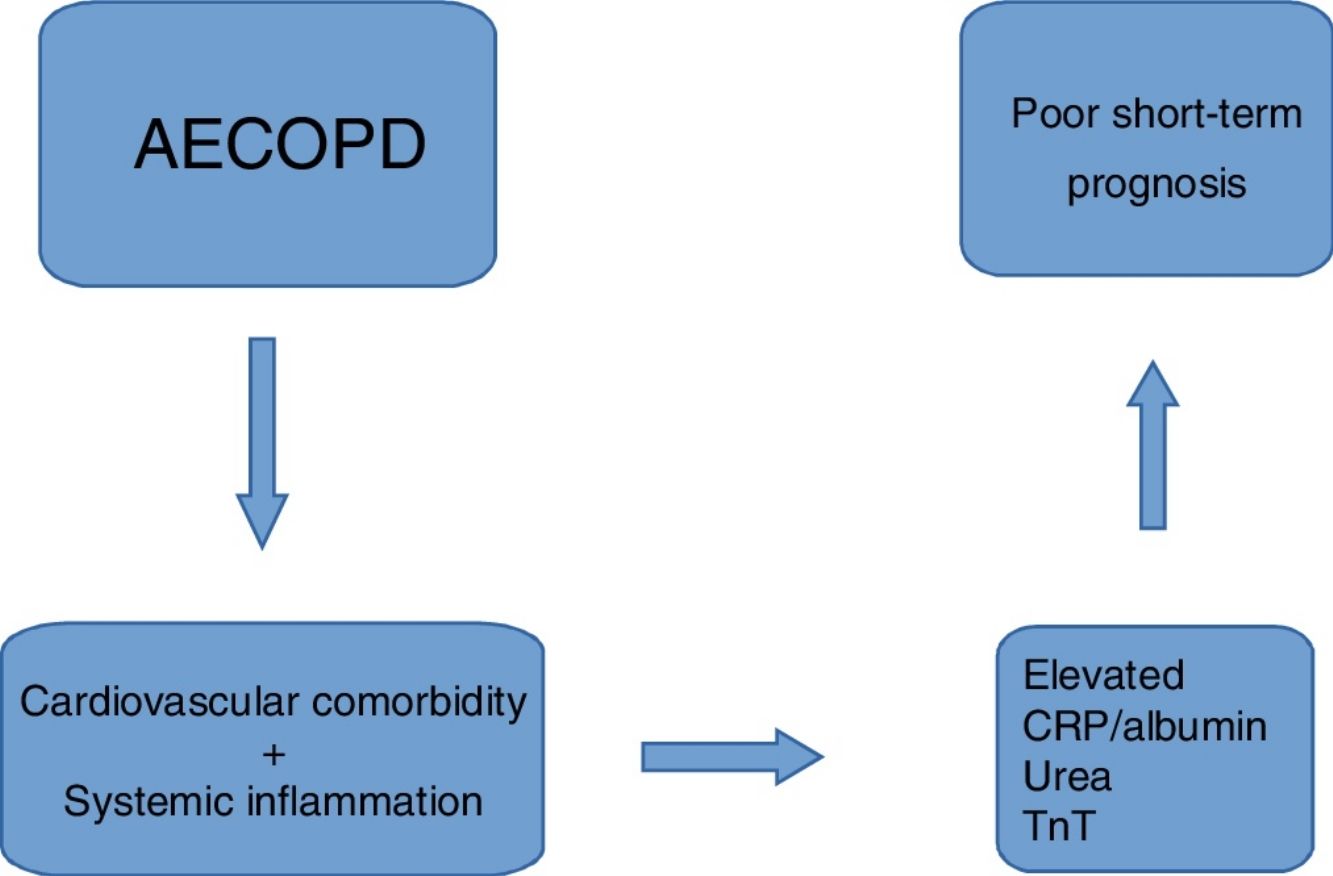
ConclusionElevated CRP/Albumin, urea and TnT are prognostic indicators of poor short-term outcome in patients admitted for COPD exacerbation. Cardiovascular comorbidity and systemic inflammation could explain these findings.
: La EPOC provoca una elevada morbimortalidad y elevados costes sanitarios. Identificar y analizar los rasgos distintivos y tratables parece útil para optimizar el tratamiento de los pacientes con AEPOC. Se han investigado varios biomarcadores sin que de momento se disponga de datos sólidos para su uso sistemático.
ObjetivoEvaluar la utilidad pronóstica a corto plazo de los parámetros clínicos y analíticos disponibles en la práctica clínica habitual en las exacerbaciones de la EPOC.
Material y métodosEstudio observacional prospectivo multicéntrico realizado entre 2016 y 2018. Se incluyeron pacientes ingresados por exacerbación de EPOC que aceptaron participar y que firmaron consentimiento informado. Se consideró evolución desfavorable la estancia prolongada, la mortalidad hospitalaria o el reingreso precoz. También se analizó la mortalidad a 30 días.
ResultadosSe incluyeron 615 pacientes. La edad media fue 73,9 años (DE 10,6); El 86,2% eran varones. Se consideró desfavorable la evolución de 357 pacientes (58%). La mortalidad al mes del alta fue del 6,7%. El análisis multivariante muestra una relación entre el ratio PCR/Albúmina y la progresión desfavorable (OR 1,008, IC 95% 1,00; 1,01), así como un mayor riesgo de muerte al mes del alta con urea elevada (OR 1,01, IC 95% 1,005; 1,02) y troponina T (OR 2,21; IC del 95%: 1,06; 4,62).
ConclusiónLa elevación de PCR/albúmina, la urea y la TnT son indicadores de mal pronóstico a corto plazo en pacientes ingresados por exacerbación de la EPOC. La comorbilidad cardiovascular y la inflamación sistémica podrían explicar estos hallazgos.
Chronic obstructive pulmonary disease (COPD) is one of the main causes of morbidity and mortality globally, although varying widely across different populations.1 COPD patients frequently show exacerbations conditioning clinical instability, caused by a heterogeneous set of alterations clinically expressed in a similar way.2 Acute exacerbations of COPD (AECOPD) have been associated with a significant increase in mortality, with 26.2% of AECOPD patients dying in the year following the exacerbation and 64.3% dying within 5 years.3,4 Due to high prevalence and morbidity, COPD causes high healthcare costs, especially in the most fragile group of patients, with 15% of all patients consuming 80% resources.5 This has triggered the search for healthcare alternatives such as home hospitalization or the use of artificial intelligence to study the disease.6–8 Also, attempts are made to progress in precision medicine, so that each patient may receive the most efficient treatment, optimizing efficacy with minimal side effects. To correctly stratify patients, classifying them according to their phenotypes, analyzing identifiable treatable traits seems useful.1,9,10 In recent years, various scales have been created to try to predict the progression of COPD exacerbations, and they have proven useful in routine clinical practice.11 The most recently studied biomarker in COPD is the level of eosinophils in peripheral blood, which seems useful to predict the response to corticosteroids or the risk of exacerbations. However, the results obtained are not homogeneous across studies, as some authors do not observe any relationship between blood eosinophil count and AECOPD.9,12–14 While other biomarkers have been researched (anemia, hyponatremia, thrombocytosis, fibrinogen, serum albumin level, etc.), no solid data for systematic use have been made available.15–19 Providing information on inflammation and nutritional status, the CRP/Albumin ratio appears to be a better predictor of prognosis in various diseases than each of these parameters individually.20–24
The aim of this study is assessing the short-term prognostic usefulness of clinical and analytical parameters available in routine clinical practice in COPD exacerbation.
Material and methodsProspective observational study conducted between 2016 and 2018 at the following centers in Galicia, Spain: Salnés County Hospital (Vilagarcía de Arousa), Arquitecto Marcide (Ferrol) and Clinic Hospital Complex of Santiago de Compostela. Patients admitted for AECOPD who agreed to participate and signed the informed consent form were included in the study. Diagnosis, baseline severity, and AECOPD were defined following the GOLD criteria.1 Patients without available baseline spirometry included in the study were diagnosed with COPD based on clinical, radiological and epidemiological criteria (previous compatible symptoms, chest X-ray suggestive of COPD and history of smoking) by the specialist responsible for admission, and subsequently reviewed by two pulmonologists from the research team.25 The baseline severity of COPD was categorized into 2 groups: mild or moderate and severe or very severe. Comorbidity was evaluated using the Charlson Index26 and categorized into 2 groups (scoring 0–2 and ≥3). Vital signs, arterial blood gases and chest X-rays were obtained upon patient arrival at the Emergency Department (ED). Hemogram and serum biochemistry data from both the ED and the hospitalization ward were recorded. Prolonged stay was defined as that equal to or greater than the median stay of the study population.27 Early readmission was defined as that occurring within the first 15 days following discharge from the AECOPD admission.28 Unfavorable progression was defined as that of those patients with a prolonged stay, dying during admission or readmitted early. Variables researched to find a relationship with unfavorable progression and 30-day mortality included hemogram data (hemoglobin, leukocytosis, neutrophilia), biochemistry data (glucose, urea, creatinine, sodium, potassium, troponin T, fibrinogen, CRP, albumin, and the CRP/Albumin index), and arterial blood gas data, using reference values from our laboratories. Troponin T (TnT) was considered positive at twice the upper limit of normality; leukocytosis if >12,000 leukocytes×106/L; neutrophilia if >70% neutrophils in peripheral blood.
Ethics approval and consent to participate: This study was performed in accordance with relevant guidelines and regulations. Original and observational study approved by the Galician Ethical Committee (Registry Code 2016/460), Spain. All patients admitted included in the study signed the informed consent form.
Statistical analysisThe data obtained from statistical analysis are expressed as mean±standard deviation (SD) in continuous variables, and as frequencies and percentages in categorical variables. Continuous variables were compared using Student's t test or Wilcoxon test; in the case of categorical variables, the Chi-square test and Fisher's exact test were used. To establish a relationship between unfavorable progression and biomarkers, a multivariate logistic regression analysis was performed, including those variables with p≤0.05 in the univariate analysis. 30-Day mortality was analyzed by Cox regression. Variables associated to p<0.05 were considered statistically significant. The analyses were carried out with SPSS 15.
Results615 patients admitted for AECOPD during the study period were included. Mean age was 73.9 years (SD 10.6); 86.2% were male. 46.2% patients had severe or very severe COPD and 83.4% scored 3 or higher on the Charlson Index. Mean stay was 8.4 days (SD 6.2). Progression of 357 patients (58%) was considered unfavorable: 54% patients had prolonged stay, in-hospital mortality was 3.7% and 6% patients were readmitted early. Mortality at one month following discharge from the index admission was 6.7%.
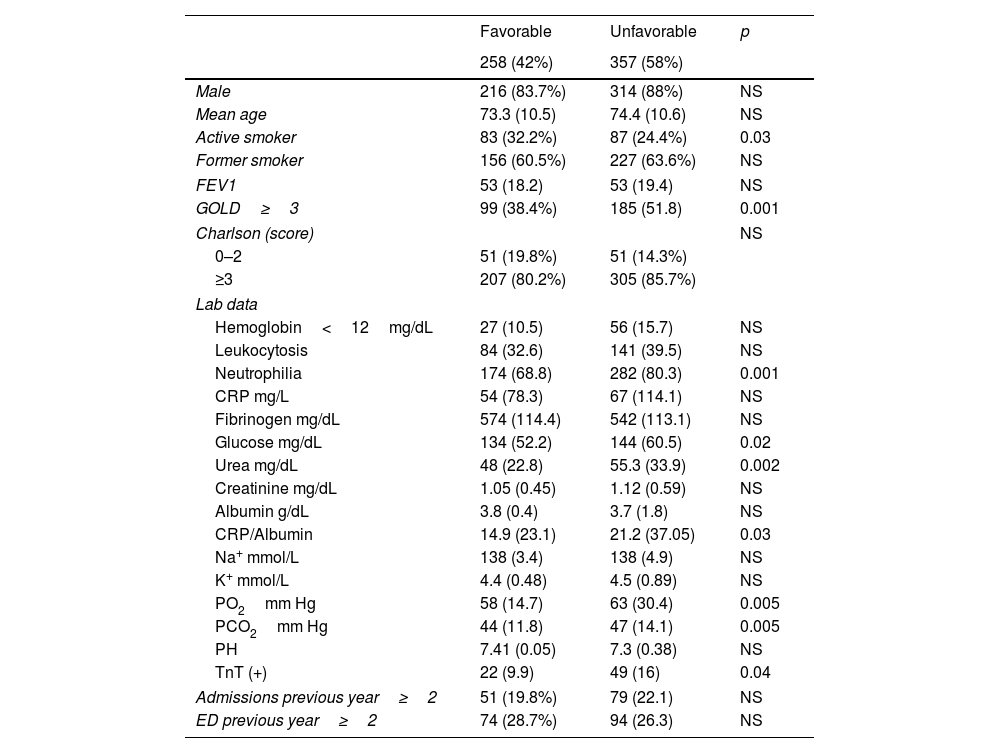
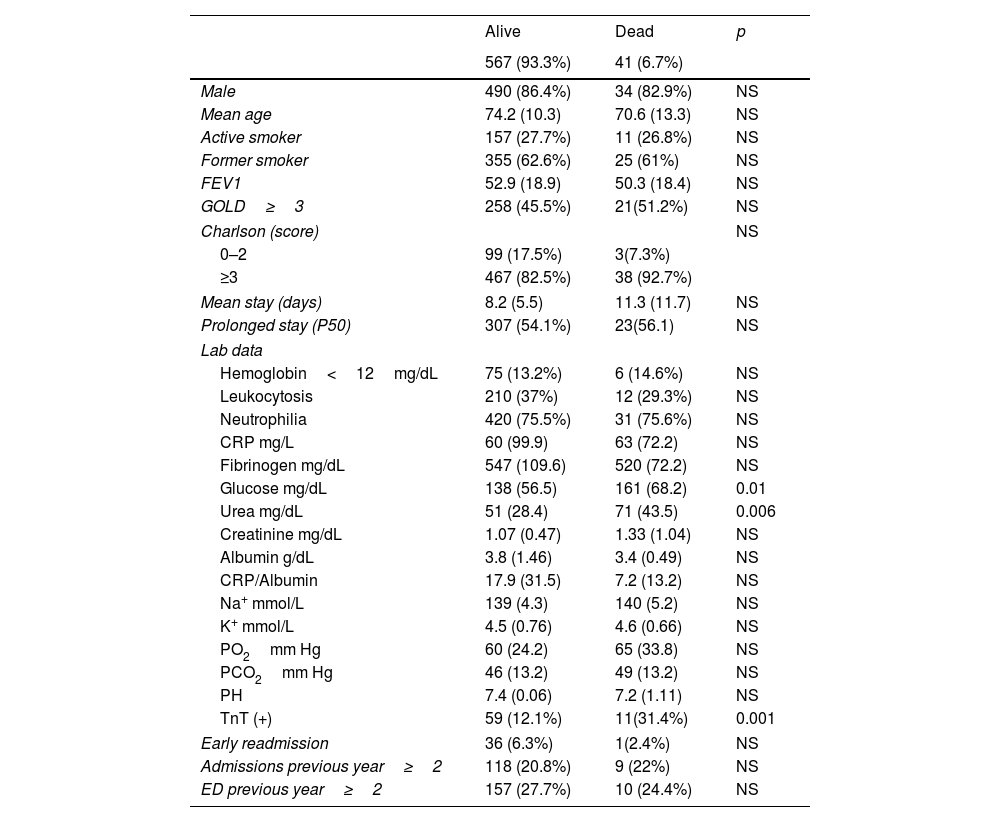
Variables related to unfavorable progression included severe or very severe COPD as per GOLD classification, neutrophilia, elevated glucose and urea, hypoxemia, hypercapnia, TnT positivity and elevated CRP/Albumin ratio. Active smoker status is associated with a favorable progression (Table 1). Variables related to 30-day mortality include elevated glucose and urea, as well as TnT positivity (Table 2). The multivariate analysis shows a relationship between the CRP/Albumin ratio and unfavorable progression (OR 1.008, 95% CI 1.00; 1.01), as well as increased risk of death at 1 month from discharge with elevated urea (OR 1.01, 95% CI 1.005; 1.02) and TnT (OR 2.21, 95% CI 1.06; 4.62) (Table 3).
Factors related with patient progression (univariate analysis).
| Favorable | Unfavorable | p | |
|---|---|---|---|
| 258 (42%) | 357 (58%) | ||
| Male | 216 (83.7%) | 314 (88%) | NS |
| Mean age | 73.3 (10.5) | 74.4 (10.6) | NS |
| Active smoker | 83 (32.2%) | 87 (24.4%) | 0.03 |
| Former smoker | 156 (60.5%) | 227 (63.6%) | NS |
| FEV1 | 53 (18.2) | 53 (19.4) | NS |
| GOLD≥3 | 99 (38.4%) | 185 (51.8) | 0.001 |
| Charlson (score) | NS | ||
| 0–2 | 51 (19.8%) | 51 (14.3%) | |
| ≥3 | 207 (80.2%) | 305 (85.7%) | |
| Lab data | |||
| Hemoglobin<12mg/dL | 27 (10.5) | 56 (15.7) | NS |
| Leukocytosis | 84 (32.6) | 141 (39.5) | NS |
| Neutrophilia | 174 (68.8) | 282 (80.3) | 0.001 |
| CRP mg/L | 54 (78.3) | 67 (114.1) | NS |
| Fibrinogen mg/dL | 574 (114.4) | 542 (113.1) | NS |
| Glucose mg/dL | 134 (52.2) | 144 (60.5) | 0.02 |
| Urea mg/dL | 48 (22.8) | 55.3 (33.9) | 0.002 |
| Creatinine mg/dL | 1.05 (0.45) | 1.12 (0.59) | NS |
| Albumin g/dL | 3.8 (0.4) | 3.7 (1.8) | NS |
| CRP/Albumin | 14.9 (23.1) | 21.2 (37.05) | 0.03 |
| Na+ mmol/L | 138 (3.4) | 138 (4.9) | NS |
| K+ mmol/L | 4.4 (0.48) | 4.5 (0.89) | NS |
| PO2mm Hg | 58 (14.7) | 63 (30.4) | 0.005 |
| PCO2mm Hg | 44 (11.8) | 47 (14.1) | 0.005 |
| PH | 7.41 (0.05) | 7.3 (0.38) | NS |
| TnT (+) | 22 (9.9) | 49 (16) | 0.04 |
| Admissions previous year≥2 | 51 (19.8%) | 79 (22.1) | NS |
| ED previous year≥2 | 74 (28.7%) | 94 (26.3) | NS |
FEV1: forced expiratory volume in 1second; GOLD: Global initiative for Chronic obstructive Pulmonary disease; Lab data: laboratory data; CRP: C-reactive protein; PO2: partial pressure of oxygen in arterial blood; PCO2: partial pressure of carbon dioxide in arterial blood; TnT: troponin T; ED: admission to the Emergency Department; NS: not significant.
Mortality at 30 days. Univariate analysis.
| Alive | Dead | p | |
|---|---|---|---|
| 567 (93.3%) | 41 (6.7%) | ||
| Male | 490 (86.4%) | 34 (82.9%) | NS |
| Mean age | 74.2 (10.3) | 70.6 (13.3) | NS |
| Active smoker | 157 (27.7%) | 11 (26.8%) | NS |
| Former smoker | 355 (62.6%) | 25 (61%) | NS |
| FEV1 | 52.9 (18.9) | 50.3 (18.4) | NS |
| GOLD≥3 | 258 (45.5%) | 21(51.2%) | NS |
| Charlson (score) | NS | ||
| 0–2 | 99 (17.5%) | 3(7.3%) | |
| ≥3 | 467 (82.5%) | 38 (92.7%) | |
| Mean stay (days) | 8.2 (5.5) | 11.3 (11.7) | NS |
| Prolonged stay (P50) | 307 (54.1%) | 23(56.1) | NS |
| Lab data | |||
| Hemoglobin<12mg/dL | 75 (13.2%) | 6 (14.6%) | NS |
| Leukocytosis | 210 (37%) | 12 (29.3%) | NS |
| Neutrophilia | 420 (75.5%) | 31 (75.6%) | NS |
| CRP mg/L | 60 (99.9) | 63 (72.2) | NS |
| Fibrinogen mg/dL | 547 (109.6) | 520 (72.2) | NS |
| Glucose mg/dL | 138 (56.5) | 161 (68.2) | 0.01 |
| Urea mg/dL | 51 (28.4) | 71 (43.5) | 0.006 |
| Creatinine mg/dL | 1.07 (0.47) | 1.33 (1.04) | NS |
| Albumin g/dL | 3.8 (1.46) | 3.4 (0.49) | NS |
| CRP/Albumin | 17.9 (31.5) | 7.2 (13.2) | NS |
| Na+ mmol/L | 139 (4.3) | 140 (5.2) | NS |
| K+ mmol/L | 4.5 (0.76) | 4.6 (0.66) | NS |
| PO2mm Hg | 60 (24.2) | 65 (33.8) | NS |
| PCO2mm Hg | 46 (13.2) | 49 (13.2) | NS |
| PH | 7.4 (0.06) | 7.2 (1.11) | NS |
| TnT (+) | 59 (12.1%) | 11(31.4%) | 0.001 |
| Early readmission | 36 (6.3%) | 1(2.4%) | NS |
| Admissions previous year≥2 | 118 (20.8%) | 9 (22%) | NS |
| ED previous year≥2 | 157 (27.7%) | 10 (24.4%) | NS |
FEV1: forced expiratory volume in 1second; GOLD: Global initiative for Chronic obstructive Pulmonary disease; Lab data: laboratory data; CRP: C-reactive protein; PO2: partial pressure of oxygen in arterial blood; PCO2: partial pressure of carbon dioxide in arterial blood; TnT: troponin T; ED: admission to the Emergency Department; NS: not significant.
In our study, a worse prognosis was observed in patients with AECOPD when they showed elevated CRP/Albumin ratio, urea or TnT.
Inflammation is one of the relevant factors in the pathophysiology of COPD, and therefore, various indicators of inflammation have been evaluated as COPD prognostic indicators.1 Providing information on inflammation and nutritional status, the CRP/Albumin ratio appears to be a better predictor of prognosis in various diseases than each of these parameters individually.20–23 Thus, Oh J. et al. found an association between the CPR/Albumin ratio determined in the Emergency Department and in-hospital mortality from any cause in patients older than 65.20 Yao et al. evaluated mortality at 28 days in patients with AECOPD and heart failure, and they included the CRP/Albumin ratio, higher in those who die, among risk factors.21 Although heart failure is a very common comorbidity in COPD, only 7.6% of our patients were admitted with decompensated heart failure in addition to AECOPD, which could explain the low strength of the relationship with unfavorable progression, and the fact that the CRP/Albumin ratio is not a very important risk factor in this group. In a sub-analysis carried out in patients with both diagnoses only, the association was lost. However, the sample was small, which may have influenced the results (46 patients, data not shown). Ranzani et al. related CRP/Albumin with 3-month mortality in septic patients admitted to the ICU,22 and Wong et al. proposed the CPR/Albumin ratio as a marker of inflammation and nutritional status in hemodialysis patients.23 Another study assessing mortality in critically ill patients admitted to the ICU proposes CRP/Albumin as a marker of mortality risk, however with less predictive power than albumin alone, APACHE II or the Charlson Index.29 Thus, the usefulness of CRP/Albumin as a predictor of 30-day mortality is questioned, which is consistent with our findings. A later study, carried out with patients admitted for AECOPD, shows a higher risk of readmission in patients with a lower CRP/Albumin,24 contrary to our results, which include early readmission in the unfavorable progression. In a study carried out with COPDGene and ECLIPSE patients, Zemans et al.30 concluded that certain groups of biomarkers, including CRP and fibrinogen, have greater predictive power in COPD than the biomarkers analyzed individually. However, they suggest that the history of exacerbation is more powerful to predict future COPD exacerbations, and that biomarkers do not provide additional information. Mathioudakis et al.31 defend that simultaneous high levels of CRP, fibrinogen and leukocyte count in peripheral blood predict the risk of exacerbation, mainly in the subgroup of patients with a history of previous exacerbations or worse FEV1. Thus, biomarkers would contribute little to the prediction of AECOPD. On the other hand, the biomarkers of inflammation do not usually remain stable over time, and we do not know whether these changes reflect the progression of patients or a change in their prognosis.18 In our study, surprisingly, no relationship was found between CRP, anemia, albumin, fibrinogen, FEV1, or severe exacerbations in the previous year and short-term prognosis. Contrary to other studies, we have not assessed the risk of future exacerbations, except those occurring during the first 15 days and leading to readmission. This probably has more to do with the characteristics of such exacerbations and the care provided during the index admission than with the baseline severity of COPD.28 The variability between the results in the literature and ours could be due to the differences in the populations studied or in the methodology used: younger age in some cases,22,29 higher percentage of women included in the analysis20,22,29; longer mean stay and higher in-hospital mortality rate in others,20,21,29 patients with decompensated comorbidities or admission to the ICU,21–29 assessment of risk of exacerbation or mortality at a longer term,18,22,30–32 or results obtained from non-original studies in other cases.18,31
Elevated urea, suggesting cardiac and renal dysfunction and unfavorable neurohormonal activation, is a sign of poor prognosis in different diseases.33,34 Previous studies relate elevated urea in patients admitted with AECOPD to in-hospital mortality and 30-day mortality.31,33–36 Furthermore, urea is included in various prognostic scales validated for COPD.36,37 Various mechanisms are proposed to explain this association: high prevalence of cardiovascular diseases in patients with COPD, infections as a cause of exacerbation and the use of corticosteroids, which increase catabolism and favor the reabsorption of urea at the kidney level, leading to elevation in peripheral blood, even with normal creatinine values, as it is the case in our study.38–40 Unlike other authors, we have not found a relationship between uremia and in-hospital mortality, which could be explained by the differences in methodology (retrospective studies), populations (age and percentage of male patients included) and in-hospital mortality.34,35
In our study, the risk factor with the strongest association with 30-day mortality was an elevation of troponin T during admission. Waschki et al. found an association between troponin I and mortality in the COSYCONET cohort.41 Other authors reported that the elevation of troponin T on admission for AECOPD increases the probability of death in the first month after discharge, and they related it to cardiac dysfunction undetected by clinical evaluations and complementary tests carried out on these patients, which is consistent with our results.42–44 However, the mechanisms that explain the progression of heart damage during AECOPD have not been established, although some have been suggested: risk factors common to COPD and cardiovascular diseases, such as tobacco use or advanced age; acute compromise of the pulmonary circulation or transient cardiac myocyte injury during AECOPD, even with no evidence of underlying heart disease; or indirect elevation of troponin in AECOPD, mediated by increased systemic inflammation.45–47 Elevated TnT has been associated with prognosis not only in AECOPD, but also in COPD patients admitted for pneumonia.47 In our population, almost 21% of the patients admitted for AECOPD showed consolidation on the chest X-ray. However, no significant differences were found in TnT between patients with and without pneumonia (data not shown), which seems to indicate that the cause of TnT elevation was probably a consequence of myocardial disease, with systemic inflammation playing a minor role.
Finally, it is worth mentioning that some surprising results have appeared in our study, such as the association between active smoking and favorable evolution, or that the FEV1 is not significant in prognosis and the GOLD classification, based on spirometric criteria, is. Other prognostic factors, such as CRP or anemia, a known independent predictor of mortality in patients with severe chronic disease,48 neither was associated with unfavorable evolution in our study. Since they are the result of a univariate analysis not confirmed with Cox regression, we cannot rule out the influence of confounding factors.
The limitations of our study include the lack of spirometry available in up to 17% of patients. The failure to consider the treatments administered during admission, mainly diuretics and corticosteroids, which could lead to different patient profiles and impact the results. We only have TnT data at admission and hence lack information on the progression of cardiac dysfunction. Other predictors of mortality in COPD, such as body mass index, exercise tolerance (6MWD) or baseline dyspnea (eMRCD) have not been assessed. However, we have a large sample from multiple hospitals that has been prospectively evaluated, which would give external validity to our results.
In conclusion, elevated CRP/Albumin, urea, and TnT are prognostic indicators of poor short-term outcome in patients admitted for AECOPD. Cardiovascular comorbidity and systemic inflammation could explain these findings. Our results could be useful to identify subpopulations of patients subject to close monitoring or individualized treatment.
FundingThis paper has not been funded.
Authors’ contributions(I) Conception and design: GS and GB; (II) Administrative support: GB and Carreira; (III) Provision of study materials or patients: GS, GB and CA; (IV) Collection and assembly of data: GS, MG, CM, CA, NF, DO, PP, and RV; (V) Data analysis and interpretation: GS, GB and Carreira; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors; (VIII) Guarantor of the paper: GS.
Conflicts of interestGonzalez-Barcala Francisco-Javier has received speaker fees, consulting fees or research grants from ALK, Astra-Zeneca, Bial, Boehringer-Ingelheim, Chiesi, Gebro Pharma, GlaxoSmithKline, Laboratorios Esteve, Menarini, Mundipharma, Novartis, Rovi, Roxall, Sanofi, Stallergenes-Greer and Teva. The remaining authors have no conflicts/competing interests to declare.
Santiago García-Sanz for the translation of the manuscript.