Platypnea-orthodeoxia syndrome (POS) is a rare phenomenon, described as the appearance of dyspnea and hypoxemia manifested with postural changes, usually in a standing position, and that improves with lying down. This syndrome is associated most frequently with a right-to-left cardiac shunt (R-L shunt), often with a patent foramen ovale (PFO), as well as non cardiac causes. Alterations in the intrathoracic anatomy such as pulmonary resections, due to mediastinal movement and displacement of the interatrial septum after an intervention, have been described to trigger this pathology.1,2
We present the case of a 70-year-old woman with a 42mm×20mm cavitated adenocarcinoma in the right lower lobe and normal mediastinum by chest computed tomography (CT) scan and positron emission tomography (PET) scan. No prior cardiopulmonary history. Lung function: FEV1 2370L (137%) and DLCO 107% and SpO2 99–97% preoperative. The usual preoperative studies did not show conditions to contraindicate surgery. Surgical treatment was decided in a multidisciplinary committee. Lower right lobectomy and lymphadenectomy by video assisted thoracoscopic surgery (VATS) were performed without intraoperative incidents.
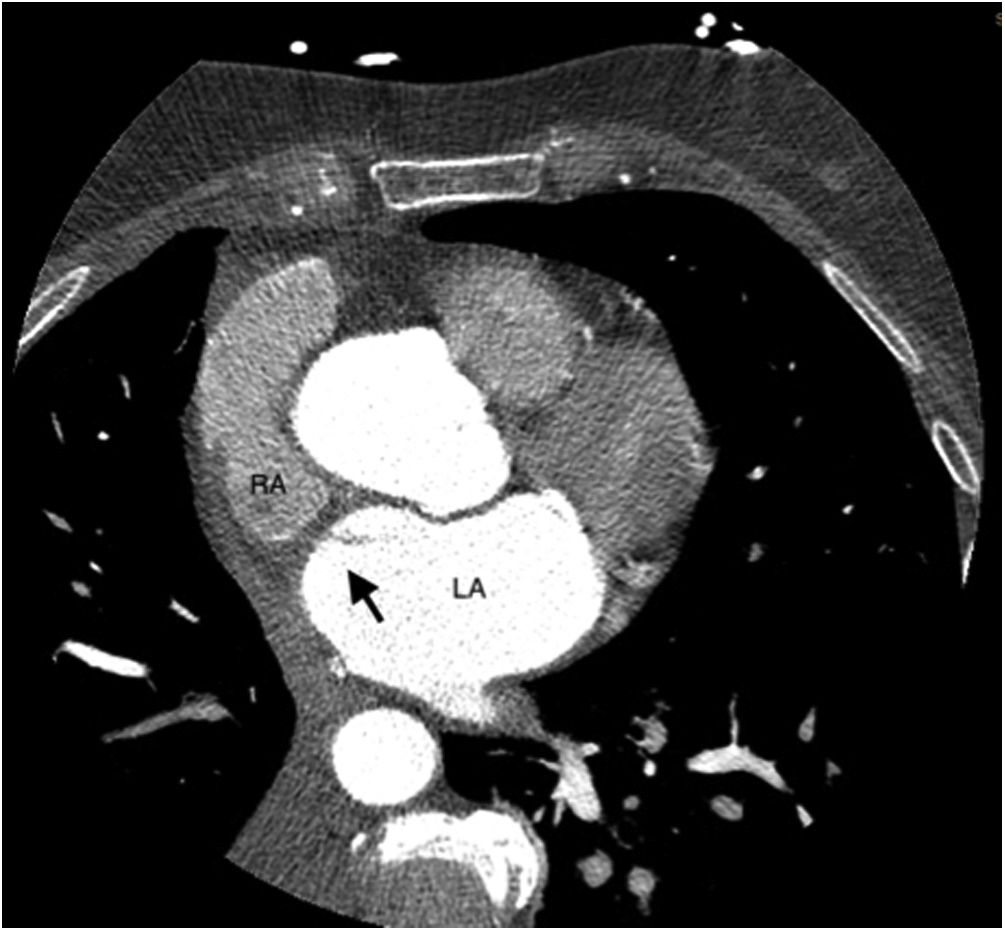
During the first week, the patient presented with oxygen desaturation from 89% to 72%, dizziness and dyspnea at rest, which was verified in the arterial blood gas: pH 7.5, pO2 48, pCO2 25 (SpO2 86%). A chest CT scan showed no signs of pulmonary embolism or other findings. Given the persistence of the symptoms, she was transferred to the intensive care unit (ICU), where she maintained oscillating saturations between 78% and 97% depending on her position. Suspecting a R-L shunt, a transthoracic echocardiogram was performed with the administration of turbulent serum in both upper extremities, showing the presence of bubbles passing from the right atrium to the left atrium. The study was completed with cardiac CT scan (Fig. 1) and transesophageal echocardiogram with evidence of R-L shunt with intracardiac defect and very likely in the interatrial septum, a foramen ovale type.
The patient was transferred to the coronary unit of reference, where she was treated percutaneously with an Amplatzer® device, accompanied by symptomatic improvement. She currently continues her oncological controls.
The following conditions have been described for the appearance of POS and they usually coexist. The first is an anatomical defect such as a PFO, fenestrated atrial septum, or aneurysmal septum.3 The second is a functional component, that increases right atrial pressure (usually lower than left atrial pressure by 1–3mmHg) and redirects blood flow through R-L shunt, like pulmonary hypertension; heart condition (aortic aneurysm, constrictive pericarditis); pulmonary (pneumonectomy, lobectomy and it has also been described in cases of interstitial pneumonia due to SARS-CoV2)4,5 or abdominal (compression of right chambers by liver lesions). Platipnea-orthodeoxia is evidenced by changes in the patient's position, from a lying to a standing position, the latter could cause the atrial septal defect to stretch, allowing blood flow from inferior vena cava through the defect, thus producing R-L shunt.
To the best of our knowledge, there are currently 10 cases of POS described in the literature after lobectomy, the majority of them right sided resections. The proposed mechanisms are: relocation of the mediastinum and stretching and distortion of the atrial septum; reduction in the pulmonary vascular bed that increases ventricular afterload as well as the previous conditions mentioned before.
The treatment in most cases (88%) is through percutaneous devices, as it was in our case. In cases of major septal or fenestrated defects, they are better suited for surgery. The resolution of the symptoms is effective in up to 95% of the cases.5 In summary, the POS after lobectomy is a rare cause of postoperative dyspnea/hypoxia must be taken into account to provide proper diagnosis and treatment.
Informed consentInformed consent was obtained from the patient's relative for publication of the clinical data and images present in this manuscript.
FundingNo external financing has been needed for this study.
Authors' contributionsLaura Costa: Done most of the work. Wrote the manuscript. Arranged the meetings for the secondary reviewers.
Sebastian Penafiel: Manuscript reviewer.
Dario Guaman: Manuscript reviewer.
Eduard Baeta: Manuscript reviewer. Senior author.
Conflicts of interestThe authors declare no conflict of interest.