COVID-19 may be a new risk factor for stroke. Stroke in COVID-19 varies from 1.1 to 8.1%. Various pathophysiological pathways predispose SARS-CoV-2 infected patients to stroke.
AimTo describe COVID-19 patients with acute stroke in one Colombian Center.
MethodsFrom March 6 2020 and March 6 2021 records of patients with acute stroke and in-hospital positive PCR (Polymerase Chain Reaction) test for Sars-CoV-2 infection were reviewed. Demographic, stroke and COVID-19 characteristics were extracted. Continuous variables were reported in means and ranges. Categorical variables were presented in frequencies and percentage. A descriptive narrative was performed.
ResultsOf 328 acute stroke patients 14 (4.2%) tested positive for PCR SARS-CoV-2. Mean age 56.4 years with 57% males. Five were (35.7%) without vascular risk factors but 9 (64.3%) overweight. Brain infarct diagnosed in 11 (78.5%), 53% with anterior circulation syndromes. Mean NIHSS score 11.8 and 7 (63%) received intravenous thrombolysis. Acute inflammatory blood biomarkers (D-dimer, ferritin, LDH elevated) were positive in all. 11 (78.5%) had symptomatic COVID-19 before stroke with a mean latency of 7 days. 12 (85.7%) had severe COVID-19 and 6 (42.8%) required mechanical ventilation. Outcome was unfavorable in 9 (64.3%) (The Modified Rankin Scale (mRS) >2), mean hospital stay was 21.8 days and in-hospital case fatality rate was 14.2%.
ConclusionIn susceptible individuals COVID-19 predisposes to stroke. Hypercoagulation and immune thrombosis may be at the culprit for this state. In Colombia, COVID-19 patients with stroke have similar characteristics to the described worldwide.
More than twenty months into the pandemic, evidence shows an association between SARS-CoV-2 infection and stroke, currently COVID-19 may be considered a new risk factor for acute ischemic stroke (AIS).1 In comparison with Influenza virus infection, COVID-19 is associated with a 7.6 fold increased risk of stroke.1 The risk is higher in patients with severe SARS-CoV-2 infection and pre-existing cardiovascular risk factors: high blood pressure, diabetes mellitus, and dyslipidemia.2 AIS in COVID-19 is more common in the elderly, of moderate severity, in the anterior circulation, cryptogenic in up to 63.6%, with large vessel occlusion in 40.9 to 60% and with a median between onset of infection symptoms and stroke of 10(+/−8) days. However, the risk extends to patients under 50 years of age, subjects without risk factors, asymptomatic individuals and to the convalescent period3 Conversely, it is recognized that AIS in COVID-19 infection increases 4 fold the risk of death and by 2.5 the development of acute respiratory distress syndrome (ARDS).4
Incidence of stroke in SARS-CoV-2 infected PCR (Polymerase Chain Reaction) positive patients varies between 1.1 to 1.4%,2–5 and up to 4.15% in patients older than 80 years of age. However, Nannoni et al. reported incidence as high as 8,1% in a single Asian study and 3.1% overall in the Asian population included in a systematic review.2
Increased risk of AIS in SARS-CoV-2 infection is multifactorial. At sites where the Angiotensin Converting Enzyme 2 (ACE2) receptor is expressed (lungs, heart, kidneys and blood vessels) there is endothelial damage and inflammation (endothelitis).2,4,6,7 There is also down-regulation of the Renin-Angiotensin System (RAS) and a decrease of Angiotensin 1–7 production, leading to failure in vascular compensatory mechanisms and an intensified vasoconstriction effect of Angiotensin II. The cytokines and chemokines produced during the active phase of infection result in a process known as immune thrombosis, due to hypercoagulability and direct damage of the endothelial surface. Activation of mononuclear cells, expression of tissue factor (TF) in the endothelial wall, expression of Von Willenbrand Factor (vWF) and the subsequent platelet adhesion through Neutrophil Extracellular Traps enhances recruitment of innate immune cells and activation of the extrinsic coagulation pathway.8 This wide range of effects leads to clot formation, a state known as Covid Associated Coagulopathy (CAC), and to plaque rupture in patients with previous atherosclerotic disease.5,6 Other factors may play an important role in this thrombosis-prone state such as dehydration, immobility, hypoxemia, ARDS promoting blood stasis and a hyperinflammatory cascade.9
In Colombia the first case of SARS-CoV-2 infection was reported on March 6th 2020. Vaccination against COVID-19 began on the 18th of February 2021. By the second week of March 2021 COVID-19 became the first all-cause mortality, with 60.082 dead, 2.262.646 confirmed cases, 34.890 active cases, 33.242 (0.1% of the population) individuals fully vaccinated and 749.059 (1.5% of the population) with at least one dose against the disease. Even though knowledge has accumulated around the disease and its relation to AIS, there is scarce information on the incidence, clinical characteristics and outcomes of stroke in SARS-CoV-2 infection in the Colombian population.10
The aim of the study is to describe the incidence, clinical characteristics and outcomes of SARS-CoV-2 infected patients with stroke in a Colombian hospital during the first year of the pandemic.
MethodsBogota is the country's (Colombia) capital, with an estimated population of approximately 7.2 million in 2019. La Cardio is a 349-bed cardiologic university clinic. In 2019, 16.075 hospital discharges and 83.102 emergencies were registered. The neurology department is composed of nine neurologists, 12 residents and four nurses, accounting for 5% (804) of all hospital discharges in 2019. The department doesn't have a neurology ward or a stroke unit, and patients are treated in general hospital beds or mixed intensive care units.
A single center retrospective cross sectional descriptive study was carried out. The medical records of all stroke patients admitted to the neurology service of La Cardio (Bogota, Colombia) between March 62,020 and March 62,021 were reviewed. Data from adult patients with acute stroke and in-hospital positive PCR (Polymerase Chain Reaction) test for Sars-CoV-2 infection were extracted. Demographic, stroke and SARS-CoV-2 infection characteristics were obtained. Admission laboratory workup and in-hospital clinical outcome for each patient was collected. Missing data were not imputed.
The study was conducted in compliance with national and international guidelines for clinical investigation. The study protocol was approved by the institutional ethics and investigational committees. Informed consent was waived in accordance with standing national clinical research law: Investigation classified as without risk and with anonymous data (Ministry of Health Resolution 8430 1993). Continuous variables were reported in mean and ranges. Categorical variables were presented in frequencies and percentage. A descriptive narrative was used to present the results of the study.
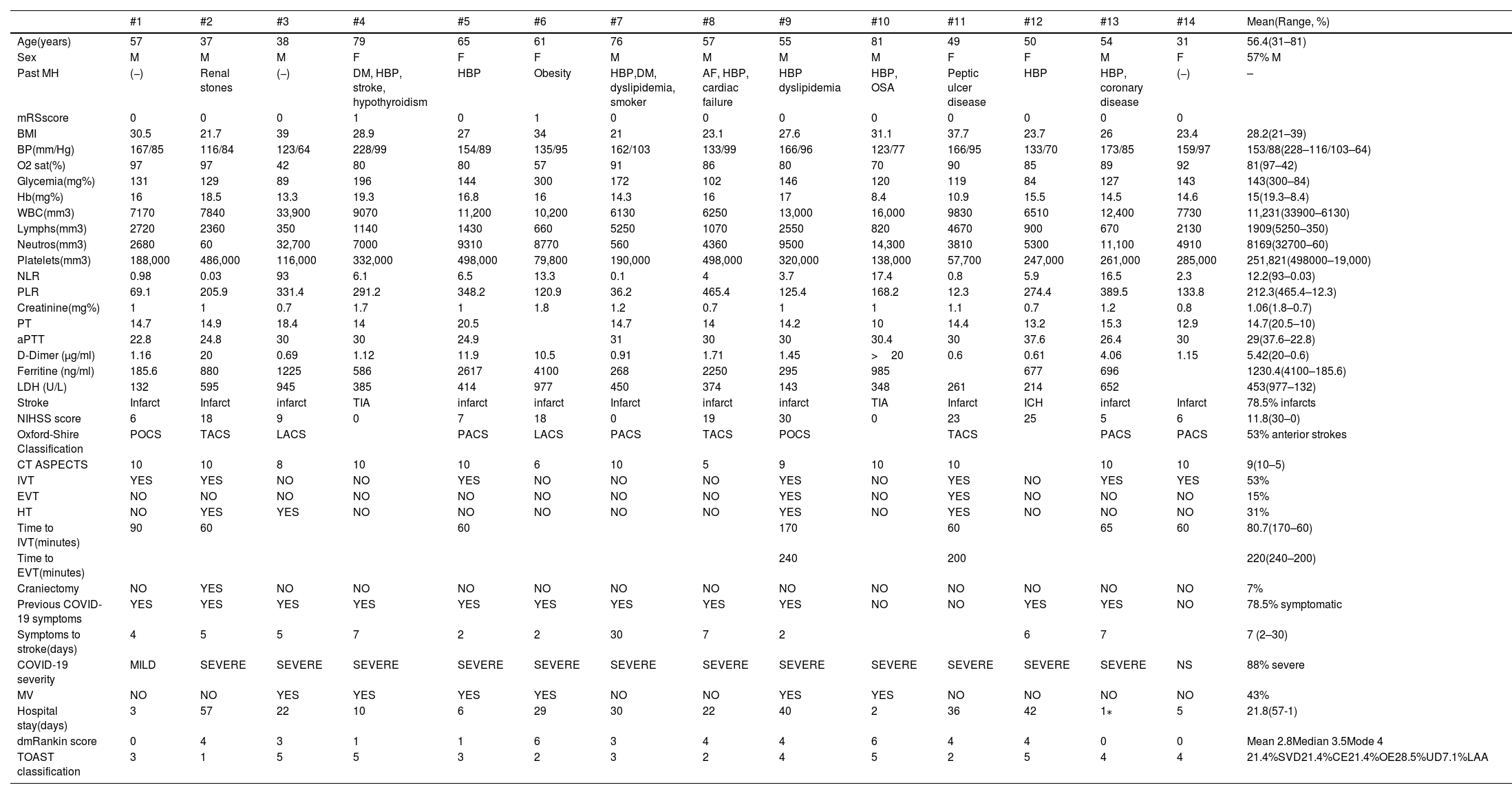
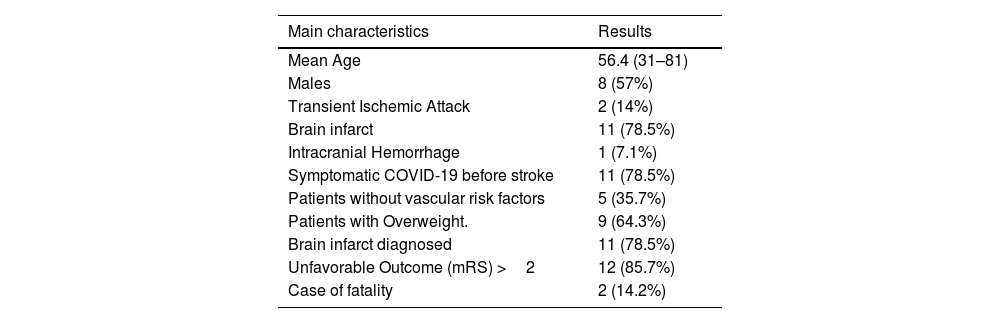
ResultsDuring the period studied (March 6, 2020-March 6, 2021), 328 patients with stroke were admitted to the neurology service. The SARS-CoV-2 PCR test in the hospital was positive in 14 patients with stroke, representing an incidence of 4.2%. All the results found in the 14 patients are shown in detail in Table 1, however the summary of the most important findings is found in Table 2 The mean age of SARS-CoV-2-infected stroke patients was 56.4 years (range 31–81 years), with 57% men. Arterial hypertension was the most prevalent risk factor (57.1%). Diabetes, dyslipidemia, and a history of heart disease were present in 14.2% each. No previous vascular risk factors were found in 5 (35.7%) patients. Overweight (BMI Body Mass Index >25) was found in 9 (64.3%) patients, including 3 without previous vascular risk factors.
Clinical and laboratory characteristics of stroke and SARS-CoV-2 infected patients. (March 6th 2020-March 6th 2021, La Cardio, Bogota, Colombia).
| #1 | #2 | #3 | #4 | #5 | #6 | #7 | #8 | #9 | #10 | #11 | #12 | #13 | #14 | Mean(Range, %) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age(years) | 57 | 37 | 38 | 79 | 65 | 61 | 76 | 57 | 55 | 81 | 49 | 50 | 54 | 31 | 56.4(31–81) |
| Sex | M | M | M | F | F | F | M | M | M | M | F | F | M | F | 57% M |
| Past MH | (−) | Renal stones | (−) | DM, HBP, stroke, hypothyroidism | HBP | Obesity | HBP,DM, dyslipidemia, smoker | AF, HBP, cardiac failure | HBP dyslipidemia | HBP, OSA | Peptic ulcer disease | HBP | HBP, coronary disease | (−) | – |
| mRSscore | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| BMI | 30.5 | 21.7 | 39 | 28.9 | 27 | 34 | 21 | 23.1 | 27.6 | 31.1 | 37.7 | 23.7 | 26 | 23.4 | 28.2(21–39) |
| BP(mm/Hg) | 167/85 | 116/84 | 123/64 | 228/99 | 154/89 | 135/95 | 162/103 | 133/99 | 166/96 | 123/77 | 166/95 | 133/70 | 173/85 | 159/97 | 153/88(228–116/103–64) |
| O2 sat(%) | 97 | 97 | 42 | 80 | 80 | 57 | 91 | 86 | 80 | 70 | 90 | 85 | 89 | 92 | 81(97–42) |
| Glycemia(mg%) | 131 | 129 | 89 | 196 | 144 | 300 | 172 | 102 | 146 | 120 | 119 | 84 | 127 | 143 | 143(300–84) |
| Hb(mg%) | 16 | 18.5 | 13.3 | 19.3 | 16.8 | 16 | 14.3 | 16 | 17 | 8.4 | 10.9 | 15.5 | 14.5 | 14.6 | 15(19.3–8.4) |
| WBC(mm3) | 7170 | 7840 | 33,900 | 9070 | 11,200 | 10,200 | 6130 | 6250 | 13,000 | 16,000 | 9830 | 6510 | 12,400 | 7730 | 11,231(33900–6130) |
| Lymphs(mm3) | 2720 | 2360 | 350 | 1140 | 1430 | 660 | 5250 | 1070 | 2550 | 820 | 4670 | 900 | 670 | 2130 | 1909(5250–350) |
| Neutros(mm3) | 2680 | 60 | 32,700 | 7000 | 9310 | 8770 | 560 | 4360 | 9500 | 14,300 | 3810 | 5300 | 11,100 | 4910 | 8169(32700–60) |
| Platelets(mm3) | 188,000 | 486,000 | 116,000 | 332,000 | 498,000 | 79,800 | 190,000 | 498,000 | 320,000 | 138,000 | 57,700 | 247,000 | 261,000 | 285,000 | 251,821(498000–19,000) |
| NLR | 0.98 | 0.03 | 93 | 6.1 | 6.5 | 13.3 | 0.1 | 4 | 3.7 | 17.4 | 0.8 | 5.9 | 16.5 | 2.3 | 12.2(93–0.03) |
| PLR | 69.1 | 205.9 | 331.4 | 291.2 | 348.2 | 120.9 | 36.2 | 465.4 | 125.4 | 168.2 | 12.3 | 274.4 | 389.5 | 133.8 | 212.3(465.4–12.3) |
| Creatinine(mg%) | 1 | 1 | 0.7 | 1.7 | 1 | 1.8 | 1.2 | 0.7 | 1 | 1 | 1.1 | 0.7 | 1.2 | 0.8 | 1.06(1.8–0.7) |
| PT | 14.7 | 14.9 | 18.4 | 14 | 20.5 | 14.7 | 14 | 14.2 | 10 | 14.4 | 13.2 | 15.3 | 12.9 | 14.7(20.5–10) | |
| aPTT | 22.8 | 24.8 | 30 | 30 | 24.9 | 31 | 30 | 30 | 30.4 | 30 | 37.6 | 26.4 | 30 | 29(37.6–22.8) | |
| D-Dimer (μg/ml) | 1.16 | 20 | 0.69 | 1.12 | 11.9 | 10.5 | 0.91 | 1.71 | 1.45 | >20 | 0.6 | 0.61 | 4.06 | 1.15 | 5.42(20–0.6) |
| Ferritine (ng/ml) | 185.6 | 880 | 1225 | 586 | 2617 | 4100 | 268 | 2250 | 295 | 985 | 677 | 696 | 1230.4(4100–185.6) | ||
| LDH (U/L) | 132 | 595 | 945 | 385 | 414 | 977 | 450 | 374 | 143 | 348 | 261 | 214 | 652 | 453(977–132) | |
| Stroke | Infarct | Infarct | infarct | TIA | infarct | infarct | Infarct | infarct | infarct | TIA | Infarct | ICH | infarct | Infarct | 78.5% infarcts |
| NIHSS score | 6 | 18 | 9 | 0 | 7 | 18 | 0 | 19 | 30 | 0 | 23 | 25 | 5 | 6 | 11.8(30–0) |
| Oxford-Shire Classification | POCS | TACS | LACS | PACS | LACS | PACS | TACS | POCS | TACS | PACS | PACS | 53% anterior strokes | |||
| CT ASPECTS | 10 | 10 | 8 | 10 | 10 | 6 | 10 | 5 | 9 | 10 | 10 | 10 | 10 | 9(10–5) | |
| IVT | YES | YES | NO | NO | YES | NO | NO | NO | YES | NO | YES | NO | YES | YES | 53% |
| EVT | NO | NO | NO | NO | NO | NO | NO | NO | YES | NO | YES | NO | NO | NO | 15% |
| HT | NO | YES | YES | NO | NO | NO | NO | NO | YES | NO | YES | NO | NO | NO | 31% |
| Time to IVT(minutes) | 90 | 60 | 60 | 170 | 60 | 65 | 60 | 80.7(170–60) | |||||||
| Time to EVT(minutes) | 240 | 200 | 220(240–200) | ||||||||||||
| Craniectomy | NO | YES | NO | NO | NO | NO | NO | NO | NO | NO | NO | NO | NO | NO | 7% |
| Previous COVID-19 symptoms | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | NO | YES | YES | NO | 78.5% symptomatic |
| Symptoms to stroke(days) | 4 | 5 | 5 | 7 | 2 | 2 | 30 | 7 | 2 | 6 | 7 | 7 (2–30) | |||
| COVID-19 severity | MILD | SEVERE | SEVERE | SEVERE | SEVERE | SEVERE | SEVERE | SEVERE | SEVERE | SEVERE | SEVERE | SEVERE | SEVERE | NS | 88% severe |
| MV | NO | NO | YES | YES | YES | YES | NO | NO | YES | YES | NO | NO | NO | NO | 43% |
| Hospital stay(days) | 3 | 57 | 22 | 10 | 6 | 29 | 30 | 22 | 40 | 2 | 36 | 42 | 1⁎ | 5 | 21.8(57-1) |
| dmRankin score | 0 | 4 | 3 | 1 | 1 | 6 | 3 | 4 | 4 | 6 | 4 | 4 | 0 | 0 | Mean 2.8Median 3.5Mode 4 |
| TOAST classification | 3 | 1 | 5 | 5 | 3 | 2 | 3 | 2 | 4 | 5 | 2 | 5 | 4 | 4 | 21.4%SVD21.4%CE21.4%OE28.5%UD7.1%LAA |
M:Male, F:Female,MH:medical history,HBP:High Blood Pressure, DM:Diabetes Mellitus, AF:Atrial fibrillation, pmRankin:previous modified Rankin,BMI:Body Mass Index, BP:Blood Pressure, O2Sat: Oxigen Saturation, Hb:Hemoglobin, WBC:White Blood Cell, Lymph:Lymphocytes,Neutro:Neutrocytes,NLR:Neutrocyte-to-Lymphocyte Ratio,PLR:Platelet-to-Lymphocyte Ratio,PT:Prothrombin Time, aPTT:activated Partial Thromboplastin Time,LDH:Lactate Dehydrogenase,TIATransient Isquemic Attack, ICH:Intracranial Hemorrhage, NIHSS:National Institute Stroke Scale, POCS:Posterior Circulation Syndrome, LACS:Lacunar Syndrome, TACS:Total Anterior Circulation Syndrome, PACS:Partial Anterior Circulation Syndrome, IVT:Intravenous Thrombolysis, EVT:Endovascular Thrombectomy, HT:Hemorrhagic Transformation, NS:No Symptoms MV: Mechanical Ventilation, dmRankin:discharge modified Rankin, TOAST: Trial of Org 10,172 Acute Stroke Treatment, SVD:Small Vessel Diesease, CE:Cardioembolic, OE:Other Etiology, UD:Undetermined, LAA:Large Artery Atherosclerosis.
Summary of main characteristics of stroke and SARS-CoV-2 infected patients. (March 6th 2020-March 6th 2021, La Cardio, Bogota, Colombia).
| Main characteristics | Results |
|---|---|
| Mean Age | 56.4 (31–81) |
| Males | 8 (57%) |
| Transient Ischemic Attack | 2 (14%) |
| Brain infarct | 11 (78.5%) |
| Intracranial Hemorrhage | 1 (7.1%) |
| Symptomatic COVID-19 before stroke | 11 (78.5%) |
| Patients without vascular risk factors | 5 (35.7%) |
| Patients with Overweight. | 9 (64.3%) |
| Brain infarct diagnosed | 11 (78.5%) |
| Unfavorable Outcome (mRS) >2 | 12 (85.7%) |
| Case of fatality | 2 (14.2%) |
mRS: modified Rankin scale.
Brain infarct was the most prevalent type of stroke, with 237(72.2%) in the overall stroke population and 11(78.5%) in the SARS-CoV-2 infected patients. A transient ischemic attack (TIA) was the presenting stroke in 57(17.4%) in the overall stroke population and in two (14%) in the SARS-CoV-2 infected patients. Only one (7%) patient with stroke and SARS-CoV-2 infection had an intracranial hemorrhage. There were no cases of cerebral venous thrombosis in the positive SARS-CoV-2 patients. Anterior circulation stroke syndrome was the most common phenotype present in 53% of the stroke and SARS-CoV-2 infected patients.
Amongst the brain infarct stroke patients with SARS-CoV-2 infection mean NIHSS score was 11.8, with 5(45.5%) classified as moderate stroke (NIHSS 5–15), 3(27.3%) as moderately severe (NIHSS 16–20), 2(18.2%) as severe and 1 with NIHSS score of 0. ASPECTS score on initial CT brain scan was 10 in 7(63.3%) brain infarct stroke patients. In the latter patients, 7(63.3%) received intravenous thrombolysis (IVT) and only two (18.8%) were taken to endovascular thrombectomy (EVT). Mean time to IVT was 80.7 min and for EVT 220 min. Hemorrhagic transformation (HT) occurred in 4 (36.4%) patients, the two with EVT, one with IVT and one with no reperfusion therapy. Craniectomy was performed in only one (7%) patient with a brain infarct.
Initial blood pressure, oxygen saturation and laboratory work-up for each patient is shown in Table 1. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR), simple parameters to assess the inflammatory status of a subject, were calculated. A NLR >4 and a PLR >200 was found in 7 (50%) patients. Most patients (78.6%) had at least 2 positive laboratory predictors for severe SARS-CoV-2 infection and 100% had elevated D-Dimer. Abnormal chest radiographs with bilateral ground-glass opacities were found in 64.3%. After laboratory work-up and according to the TOAST stroke classification 23% were attributed to small vessel disease, 23% to cardioembolism, 23% to other etiology, 15% to undetermined etiology and 7% to large artery atherosclerosis.
Previous COVID-19 symptoms before stroke were reported by most (78.5%) patients, with a mean latency of symptom onset to stroke of 7 days. The most frequently reported symptoms included cough, fever, myalgia and dyspnea. Twelve (85.7%) patients were classified with a severe SARS-CoV-2 infection.
Six (42.8%) stroke patients with SARS-CoV-2 infection required mechanical ventilation. Mean hospital stay was 21.8 days and in-hospital case fatality rate was 14.2%. In-hospital discharge outcome, measured with mRS, was unfavorable (mRS >2) in 9 (64.3%) patients. Hospital discharge mRS mean, median and mode were 2.8, 3.5 and 4 respectively.
DiscussionTo the best of our knowledge this is the first case series in Colombia of stroke patients with SARS-CoV-2 infection. Our findings are in accordance with the global reports on the topic. Stroke incidence of 4.2% in our studied population is in the range described worldwide. As in other cohorts or case series, patients tended to be younger, with less vascular risk factors but overweight.11 Also, anterior circulation brain infarct was the more prevalent type of stroke with a moderate to severe (NIHSS score > 5) presentation. On the contrary to previous reports, IVT and EVT were performed in high percentage of patients, 63.3% and 18.8% respectively. Hemorrhagic transformation (HT) occurred in a high proportion of patients (36.4%), but type of HT was not specified.
SARS-CoV-2 infection was symptomatic and severe in most of our patients, as has been previously reported. Acute inflammatory biomarkers (D-dimer, ferritin, LDH elevated) were positive in all patients and in relation to the severity of the infection. Latency of COVID-19 symptoms before stroke was 7 days, in the range of 10(+/−8) days found in the literature. Like other case series, cough, fever, myalgia and dyspnea were the commonly reported symptoms.
Mechanical ventilation was required in almost half of our stroke patients with SARS-CoV-2 infection, but probably in relation to the COVID-19 severity. Long hospital stays were observed (21.8 days), maybe a consequence of COVID-19 and stroke severity. Unfavorable Outcome discharge (mRS >2) in 64.3% is likely due to the combination of severe infection and stroke severity. In-hospital case fatality rate of 14.2% falls below the range previously reported in these patients but higher than in patients without coronavirus infection.
The high volume of strokes in our center, thorough review of medical electronic records, completeness of data, extensive work-up and inclusion of only positive PCR COVID-19 patients are strengths of the study. Limitations of the study include the small number of patients, its retrospective design, a single center protocol, in-hospital follow up only, including only admission laboratory work-up and not accounting for experience and behavioral changes in health personnel and the community.
COVID-19 is emerging as a new stroke risk factor.12 The clinical severity of the infection and the related inflammatory response may be determinants in this association.13 The stroke's profile may be different in the COVID-19 patient, and therefore diagnostic and treatment approaches may have to differ. However, our study supports the many similarities of stroke patients with SARS-CoV-2 infection across geographical regions and provides data to narrow the knowledge gap of this new evolving disease.
ConclusionsCOVID-19 is emerging as a new stroke risk factor. The inflammatory response to a severe SARS-CoV-2 infection induces a hypercoagulation prone state or may activate immune thrombosis in patients with previous vascular risk factors. In Colombia, COVID-19 patients with stroke have similar characteristics to those described worldwide. By describing acute stroke COVID-19 patients, we want to open the door to investigate whether they differ from non-COVID-19 stroke patients, which is likely to require future studies for specific diagnostic and treatment approaches.
Retrospective descriptive study.
FundingThe authors received no financial support for this article.
Ethical considerationsProtection of humans and animals.
The authors declare that no experiments on humans or animals have been performed for this research.
Confidentiality of dataThe authors declare that they have followed their centre's protocols on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.