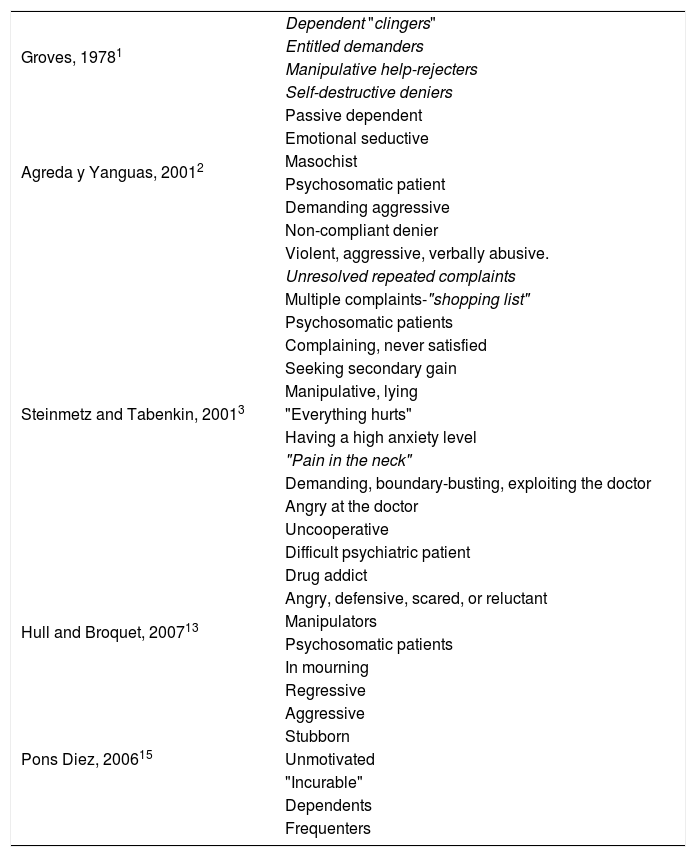
array:24 [ "pii" => "S2387020621001558" "issn" => "23870206" "doi" => "10.1016/j.medcle.2020.07.023" "estado" => "S300" "fechaPublicacion" => "2021-05-07" "aid" => "5295" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2020" "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Med Clin. 2021;156:459-62" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "es" => array:19 [ "pii" => "S0025775320304553" "issn" => "00257753" "doi" => "10.1016/j.medcli.2020.07.003" "estado" => "S300" "fechaPublicacion" => "2021-05-07" "aid" => "5295" "copyright" => "Elsevier España, S.L.U." "documento" => "article" "crossmark" => 1 "subdocumento" => "sco" "cita" => "Med Clin. 2021;156:459-62" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "es" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Artículo especial</span>" "titulo" => "Reflexiones sobre el paciente difícil" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "459" "paginaFinal" => "462" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Reflections on the difficult patient" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Miguel Bruguera, Josep Arimany-Manso" "autores" => array:2 [ 0 => array:2 [ "nombre" => "Miguel" "apellidos" => "Bruguera" ] 1 => array:2 [ "nombre" => "Josep" "apellidos" => "Arimany-Manso" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020621001558" "doi" => "10.1016/j.medcle.2020.07.023" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020621001558?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775320304553?idApp=UINPBA00004N" "url" => "/00257753/0000015600000009/v1_202104290731/S0025775320304553/v1_202104290731/es/main.assets" ] ] "itemSiguiente" => array:20 [ "pii" => "S2387020621001765" "issn" => "23870206" "doi" => "10.1016/j.medcle.2020.09.004" "estado" => "S300" "fechaPublicacion" => "2021-05-07" "aid" => "5487" "copyright" => "The Author(s)" "documento" => "simple-article" "crossmark" => 1 "licencia" => "http://creativecommons.org/licenses/by-nc-nd/4.0/" "subdocumento" => "pgl" "cita" => "Med Clin. 2021;156:463.e1-463.e30" "abierto" => array:3 [ "ES" => true "ES2" => true "LATM" => true ] "gratuito" => true "lecturas" => array:1 [ "total" => 0 ] "en" => array:13 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Consensus statement</span>" "titulo" => "Diagnosis and treatment of hepatocellular carcinoma. Update of the consensus document of the AEEH, AEC, SEOM, SERAM, SERVEI, and SETH" "tienePdf" => "en" "tieneTextoCompleto" => "en" "tieneResumen" => array:2 [ 0 => "en" 1 => "es" ] "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "463.e1" "paginaFinal" => "463.e30" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Diagnóstico y tratamiento del carcinoma hepatocelular. Actualización del documento de consenso de la AEEH, AEC, SEOM, SERAM, SERVEI y SETH" ] ] "contieneResumen" => array:2 [ "en" => true "es" => true ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1664 "Ancho" => 2656 "Tamanyo" => 263329 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Fig. " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Algorithm for the diagnosis of hepatocellular carcinoma.</p> <p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">MDCT: Multidetector CT, ECA-MRI: Magnetic resonance imaging with extracellular contrast agents, GA-MRI: Gadoxetic acid-enhanced magnetic resonance imaging.</p> <p id="spar0015" class="elsevierStyleSimplePara elsevierViewall">*Given that the probability of obtaining a false negative result can reach up to 30% in nodules smaller than 2 cm, if the biopsy is negative, consider repeating it, or close surveillance by imaging.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "María Reig, Alejandro Forner, Matías A. Ávila, Carmen Ayuso, Beatriz Mínguez, María Varela, Itxarone Bilbao, José Ignacio Bilbao, Marta Burrel, Javier Bustamante, Joana Ferrer, Miguel Ángel Gómez, Josep María Llovet, Manuel De la Mata, Ana Matilla, Fernando Pardo, Miguel A. Pastrana, Manuel Rodríguez-Perálvarez, Josep Tabernero, José Urbano, Ruth Vera, Bruno Sangro, Jordi Bruix" "autores" => array:23 [ 0 => array:2 [ "nombre" => "María" "apellidos" => "Reig" ] 1 => array:2 [ "nombre" => "Alejandro" "apellidos" => "Forner" ] 2 => array:2 [ "nombre" => "Matías A." "apellidos" => "Ávila" ] 3 => array:2 [ "nombre" => "Carmen" "apellidos" => "Ayuso" ] 4 => array:2 [ "nombre" => "Beatriz" "apellidos" => "Mínguez" ] 5 => array:2 [ "nombre" => "María" "apellidos" => "Varela" ] 6 => array:2 [ "nombre" => "Itxarone" "apellidos" => "Bilbao" ] 7 => array:2 [ "nombre" => "José Ignacio" "apellidos" => "Bilbao" ] 8 => array:2 [ "nombre" => "Marta" "apellidos" => "Burrel" ] 9 => array:2 [ "nombre" => "Javier" "apellidos" => "Bustamante" ] 10 => array:2 [ "nombre" => "Joana" "apellidos" => "Ferrer" ] 11 => array:2 [ "nombre" => "Miguel Ángel" "apellidos" => "Gómez" ] 12 => array:2 [ "nombre" => "Josep María" "apellidos" => "Llovet" ] 13 => array:2 [ "nombre" => "Manuel" "apellidos" => "De la Mata" ] 14 => array:2 [ "nombre" => "Ana" "apellidos" => "Matilla" ] 15 => array:2 [ "nombre" => "Fernando" "apellidos" => "Pardo" ] 16 => array:2 [ "nombre" => "Miguel A." "apellidos" => "Pastrana" ] 17 => array:2 [ "nombre" => "Manuel" "apellidos" => "Rodríguez-Perálvarez" ] 18 => array:2 [ "nombre" => "Josep" "apellidos" => "Tabernero" ] 19 => array:2 [ "nombre" => "José" "apellidos" => "Urbano" ] 20 => array:2 [ "nombre" => "Ruth" "apellidos" => "Vera" ] 21 => array:2 [ "nombre" => "Bruno" "apellidos" => "Sangro" ] 22 => array:2 [ "nombre" => "Jordi" "apellidos" => "Bruix" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775320307697" "doi" => "10.1016/j.medcli.2020.09.022" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => true "ES2" => true "LATM" => true ] "gratuito" => true "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775320307697?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020621001765?idApp=UINPBA00004N" "url" => "/23870206/0000015600000009/v1_202105020816/S2387020621001765/v1_202105020816/en/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S2387020621000073" "issn" => "23870206" "doi" => "10.1016/j.medcle.2020.11.003" "estado" => "S300" "fechaPublicacion" => "2021-05-07" "aid" => "5496" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "rev" "cita" => "Med Clin. 2021;156:449-58" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:13 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Review</span>" "titulo" => "Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review" "tienePdf" => "en" "tieneTextoCompleto" => "en" "tieneResumen" => array:2 [ 0 => "en" 1 => "es" ] "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "449" "paginaFinal" => "458" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Impacto psicológico de la COVID-19 en profesionales sanitarios de primera línea en el ámbito occidental. Una revisión sistemática" ] ] "contieneResumen" => array:2 [ "en" => true "es" => true ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "resumenGrafico" => array:2 [ "original" => 0 "multimedia" => array:8 [ "identificador" => "fig0005" "etiqueta" => "Fig. 1" "tipo" => "MULTIMEDIAFIGURA" "mostrarFloat" => true "mostrarDisplay" => false "figura" => array:1 [ 0 => array:4 [ "imagen" => "gr1.jpeg" "Alto" => 1815 "Ancho" => 2168 "Tamanyo" => 333034 ] ] "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Fig. " "rol" => "short" ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Flow diagram of the bibliographic selection process. Own elaboration based on the Prisma guidelines<a class="elsevierStyleCrossRef" href="#bib0255"><span class="elsevierStyleSup">51</span></a>.</p>" ] ] ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Alina Danet Danet" "autores" => array:1 [ 0 => array:2 [ "nombre" => "Alina" "apellidos" => "Danet Danet" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "es" => array:9 [ "pii" => "S0025775320308253" "doi" => "10.1016/j.medcli.2020.11.009" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "es" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775320308253?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020621000073?idApp=UINPBA00004N" "url" => "/23870206/0000015600000009/v1_202105020816/S2387020621000073/v1_202105020816/en/main.assets" ] "en" => array:16 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Special article</span>" "titulo" => "Reflections on the difficult patient" "tieneTextoCompleto" => true "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "459" "paginaFinal" => "462" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Miguel Bruguera, Josep Arimany-Manso" "autores" => array:2 [ 0 => array:3 [ "nombre" => "Miguel" "apellidos" => "Bruguera" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] ] ] 1 => array:4 [ "nombre" => "Josep" "apellidos" => "Arimany-Manso" "email" => array:1 [ 0 => "josep.arimany@comb.cat" ] "referencia" => array:2 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] 1 => array:2 [ "etiqueta" => "*" "identificador" => "cor0005" ] ] ] ] "afiliaciones" => array:2 [ 0 => array:3 [ "entidad" => "Unidad de Estudios Académicos, Colegio de Médicos de Barcelona, Barcelona, Spain" "etiqueta" => "a" "identificador" => "aff0005" ] 1 => array:3 [ "entidad" => "Servicio de Responsabilidad Profesional, Área de Praxis, Colegio de Médicos de Barcelona, Consejo de Colegios de Médicos de Catalunya, Barcelona, Spain" "etiqueta" => "b" "identificador" => "aff0010" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Reflexiones sobre el paciente difícil" ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">The health care activity generates a doctor-patient relationship that determines the medical act, which entails a personal interrelation that goes beyond a simple technical intervention and is integrated in the context of a human interaction, with a permanent emotional content. In this sense, there are multiple publications that classify, define, and describe the main characteristics of the so-called <span class="elsevierStyleItalic">difficult patient</span> (DP). Our intention in this paper is to offer some reflections on this construct called DP, emphasising certain personal considerations based on our experience over many years as health care physicians.</p><p id="par0010" class="elsevierStylePara elsevierViewall">There are various descriptions regarding the DP. All of them have a common characteristic: they indicate that they are patients who induce a feeling of distress (unpleasant subjective feeling) or a negative sensation in the doctor or in the care team, which can lead to a possible rejection of the professional and the demand for greater dedication from the care team.<a class="elsevierStyleCrossRefs" href="#bib0005"><span class="elsevierStyleSup">1–3</span></a> The aim of this paper is not to describe the different types of DP. We believe that it is more useful to propose strategies to deal with and reverse this situation, taking into account three factors: the patient himself, the doctor himself and the environment.</p><p id="par0015" class="elsevierStylePara elsevierViewall">The identification of a DP, his or her handling and management of the levels of conflict in the patient-doctor relationship by the doctor implies communication skills and therefore the need for him or her to be trained and skilled in this area.</p><span id="sec0005" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0005">The doctor-patient encounter</span><p id="par0020" class="elsevierStylePara elsevierViewall">The patient goes to the doctor most of the time with a health problem. The medical act requires building a relationship of mutual trust, which must be encouraged by the doctor himself, the promoter of this relationship, and also a smooth, empathic, and totally transparent transference and countertransference relationship. This is required by the current practice of medicine, where the right to information and the principle of patient autonomy are key values.</p><p id="par0025" class="elsevierStylePara elsevierViewall">The meeting with the patient must be considered by the doctor as an extremely important act in which he/she must not only interpret the meaning of the symptoms reported by the patient, but also create an atmosphere of serenity, cordiality, affection, respect and empathy and connect with the patient's feelings in an appropriate way so that the patient gains confidence, since the patient's confidence in the doctor's decisions contributes to the improvement of his/her state of mind and, sometimes, also of his/her physical state.</p><p id="par0030" class="elsevierStylePara elsevierViewall">Usually, the doctor sees patients in a positive frame of mind, but sometimes there is a care pressure that causes tension and stress for the doctor, which can affect this doctor-patient relationship and the conviction that the doctor's intervention will be useful, so that he or she will receive moral gratification from the patient's gratitude, sometimes verbal and sometimes only gestural. However, in some cases the visit becomes a kind of punishment for the doctor when the patient's attitude or behaviour causes discomfort or displeasure.</p><p id="par0035" class="elsevierStylePara elsevierViewall">In these cases, it is often referred to as DP or difficult-to-treat patients,<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a> terms that are perhaps not very precise but that avoid the use of more aggressive terms used by other authors, such as that of hateful patient<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> or from <span class="elsevierStyleItalic">heartsink patients</span><a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">5</span></a> or frustrating<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">6</span></a> or conflictive patients.<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">7</span></a> The name Groves syndrome was also proposed, as it was Groves who first described the existence of DP in 1978.<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a></p></span><span id="sec0010" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0010">Difficult patient types</span><p id="par0040" class="elsevierStylePara elsevierViewall">There are various types of DP. Those patients who systematically force longer visits than is considered necessary to provide good care are considered to be DPs. There are also so-called hyper-frequenters, those who show dissatisfaction not motivated by the service they have received, those who give long, complex, and unnecessary explanations, those who show unfounded doubts about what the doctor indicates or proposes, and those who request services to which they are not entitled.</p><p id="par0045" class="elsevierStylePara elsevierViewall">Equally difficult to deal with are those who are demanding, aggressive, insistent, non-compliant, those who doubt the professional's interest in the patient or his or her competence and, finally, those who display an insurmountable language barrier.</p><p id="par0050" class="elsevierStylePara elsevierViewall">In some situations, a DP is referred to as a psychiatric patient and sometimes they are patients with a substrate of personality disorder and therefore require management skills on the part of the professional.</p></span><span id="sec0015" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0015">They are not difficult patients</span><p id="par0055" class="elsevierStylePara elsevierViewall">The patients described above must be distinguished from those who pose another type of difficulty for which they are not to blame, such as those with a serious illness or poor prognosis, terminally ill patients, patients with chronic pathologies, those difficult to diagnose, those who do not respond to appropriately prescribed treatment, psychiatric patients<a class="elsevierStyleCrossRef" href="#bib0040"><span class="elsevierStyleSup">8</span></a> or those not capable of making decisions,<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">9</span></a> as well as those with co-morbidities. In these cases, the difficulty is posed by the disease and its management, not by the patient.</p></span><span id="sec0020" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0020">Prevalence</span><p id="par0060" class="elsevierStylePara elsevierViewall">Research estimates that 1–3% of patients in an outpatient practice are PD,<a class="elsevierStyleCrossRef" href="#bib0050"><span class="elsevierStyleSup">10</span></a> although the prevalence of this category of patients varies greatly between professionals, depending to a large extent on the technical skills of the doctors themselves in managing this type of patient.<a class="elsevierStyleCrossRef" href="#bib0055"><span class="elsevierStyleSup">11</span></a> In the light of this finding, one might ask whether the problem is the PDs or inexperienced doctors, or both, who do not express the empathy necessary for a good doctor-patient relationship, or do not have the necessary knowledge to ensure that the patient does not lose confidence in them or lose control when faced with reasonable questions or requests from the patient. The only viable strategy in this regard is to include and enhance the competencies necessary for good patient-physician relationships in the initial undergraduate training in medical studies. People with this profile should never be stigmatised, as it could hinder the establishment of a proper doctor-patient relationship by negatively biasing this type of patient.</p></span><span id="sec0025" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0025">The care of difficult patients by their doctor</span><p id="par0065" class="elsevierStylePara elsevierViewall">A study carried out in primary care shows how patients considered DPs by their referring doctor had a high degree of satisfaction with the treatment they received from their doctor.<a class="elsevierStyleCrossRef" href="#bib0060"><span class="elsevierStyleSup">12</span></a></p><p id="par0070" class="elsevierStylePara elsevierViewall">It should also be noted that PDs run the risk of a lower rate of correct diagnoses compared to other patients.<a class="elsevierStyleCrossRef" href="#bib0065"><span class="elsevierStyleSup">13</span></a> They could be seen as hindering medical reasoning and thus reducing the diagnostic accuracy of the practitioner. In fact, for some professionals, distress begins, in the case of scheduled visits, at the very moment when they discover a DP on the list of patients to be seen.</p></span><span id="sec0030" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0030">Recommendations for the management of the difficult patient</span><p id="par0075" class="elsevierStylePara elsevierViewall">The following is a series of general and special strategies for the correct management of DP, based on the personal experience of the authors, whose professional life has been mainly based on specialised medical visits. Similarly, some general considerations are set out in relation to the medical act.</p><span id="sec0035" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0035">General strategies</span><p id="par0080" class="elsevierStylePara elsevierViewall">Schedule, when possible, the DP in the last places in the order of visits. This requires a list of PDs and the cooperation of the administrative staff who schedule the visits, always ensuring that they are not stigmatised.</p><p id="par0085" class="elsevierStylePara elsevierViewall">Avoid telephone or face-to-face interruptions during the consultation with a DP.</p><p id="par0090" class="elsevierStylePara elsevierViewall">Provide justification for any interruptions or delays in relation to the time the visit was scheduled to take place.</p><p id="par0095" class="elsevierStylePara elsevierViewall">Try not to say anything that might irritate the patient, not to argue with them or try to convince them when they have a different opinion from ours and use communication skills.</p><p id="par0100" class="elsevierStylePara elsevierViewall">Be respectful and considerate of their requests, in the case of prolonging a sick leave or receiving drugs that they do not need. In such cases it is important to negotiate skilfully in order to reach an agreement.</p><p id="par0105" class="elsevierStylePara elsevierViewall">In situations where the patient reacts aggressively, we have to avoid confrontation and conflict. Maintain an appropriate tone of voice, which does not contribute to increasing tension and try at all times to remain calm and serene. Cooperation from other members of the care team can help in the management of the situation.</p></span><span id="sec0040" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0040">Special strategies</span><p id="par0110" class="elsevierStylePara elsevierViewall">Ask patients who come to the doctor with a long list of problems to prioritize and only state the issues that concern them most at each visit.</p><p id="par0115" class="elsevierStylePara elsevierViewall">In cases where the patient has difficulty in explaining him/herself or where there is a significant language barrier, request that he/she be accompanied to the visit, provided that there is no confidentiality situation.</p></span><span id="sec0045" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0045">The medical act</span><p id="par0120" class="elsevierStylePara elsevierViewall">Firstly, it is necessary to distinguish whether the suspected DP has his cognitive and volitional capacities preserved; if not, referral to specialised care should be made.</p><p id="par0125" class="elsevierStylePara elsevierViewall">Second, it is essential to distinguish whether it is an organ or functional pathology, a distinction that sometimes requires a physical examination and complementary tests in order to detect any abnormality associated with organ damage.</p><p id="par0130" class="elsevierStylePara elsevierViewall">Thirdly, it is important to identify the type of DP we are dealing with, as our attitude should not be the same if the patient is aggressive, rude, irresponsible, or not very competent.</p><p id="par0135" class="elsevierStylePara elsevierViewall">When faced with a patient who is extremely talkative, it is essential to detect which health problem is really worrying him/her.<a class="elsevierStyleCrossRef" href="#bib0070"><span class="elsevierStyleSup">14</span></a></p><p id="par0140" class="elsevierStylePara elsevierViewall">When, despite our efforts and skills, we are not able to manage a DP adequately, a change of professional should be proposed. In these cases, we have to follow a cautious approach and look for the most appropriate moment to suggest it.</p><p id="par0145" class="elsevierStylePara elsevierViewall">Regardless of how the patient addresses us, we should maintain a respectful and polite manner throughout the visit, addressing the patient formally and politely requesting that the patient's manner towards us is also appropriate.</p><p id="par0150" class="elsevierStylePara elsevierViewall">It is essential to maintain an attitude of listening with interest, avoiding hiding behind the computer screen.</p><p id="par0155" class="elsevierStylePara elsevierViewall">Medicalisation of PDs should be minimised, taking into account the balance between risk and benefit; unnecessary and unjustified medical acts have potential risks to which patients should not be exposed. On the other hand, this attitude is unnecessarily costly and does not solve the problem of dealing with the difficult patient, as the prescription may end the current visit but does not prevent subsequent visits.</p><p id="par0160" class="elsevierStylePara elsevierViewall">Probably the most appropriate approach to a DP is to handle the visit as any other normal medical act, applying all our communication skills and resources so that the patient trusts us and follows our recommendations, without the need to argue or debate them one by one.</p></span></span><span id="sec0050" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0050">Conclusions</span><p id="par0165" class="elsevierStylePara elsevierViewall">In our opinion and from our professional experience, based on the premise of the existence of patients who make the clinical act more difficult, the different classifications, which do not coincide (<a class="elsevierStyleCrossRef" href="#tbl0005">Table 1</a>), as well as being highly biased by the influence of the cultural context in which they are produced, are not very useful.</p><elsevierMultimedia ident="tbl0005"></elsevierMultimedia><p id="par0170" class="elsevierStylePara elsevierViewall">By approaching behaviour as if it were the patient's "being", it is not considered that the same behaviour can have very different causes and therefore the effectiveness of addressing it will depend on the appropriateness and relevance of the response in relation to the factors that are causing it.</p><p id="par0175" class="elsevierStylePara elsevierViewall">Patient behaviours are multifactorial in nature. Behind the behaviour of regressive, manipulative, demanding, aggressive or non-compliant patients, there may be different explanatory causes. The fact of approaching situations of relational difficulty from this perspective, including contextual factors and the doctor's own characteristics among the factors of influence, implies a personal positioning that, from the outset, increases capacity.</p><p id="par0180" class="elsevierStylePara elsevierViewall">Because, although in the literature reviewed we have found expressions such as "the difficult to handle patient",<a class="elsevierStyleCrossRef" href="#bib0020"><span class="elsevierStyleSup">4</span></a> "the difficult patient",<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a> terms such as "the hateful patient",<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a> "heartsink patients"<a class="elsevierStyleCrossRef" href="#bib0025"><span class="elsevierStyleSup">5</span></a> or "frustrating patients",<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">6</span></a> any interpersonal communication situation, such as that which exists in the medical practice, is more or less difficult and conflictive depending on different factors, in which the patient's profile is just one more, and whose influence can be more or less decisive in the final outcome. Obviously, the extent to which each situation is appropriately managed will depend on the degree to which responses are tailored both to the possible factors causing the difficult behaviour and to the type of behaviour manifested by the patient.</p><p id="par0185" class="elsevierStylePara elsevierViewall">There are strategies for dealing with these situations,<a class="elsevierStyleCrossRef" href="#bib0075"><span class="elsevierStyleSup">15</span></a> such as communication skills,<a class="elsevierStyleCrossRef" href="#bib0080"><span class="elsevierStyleSup">16</span></a> training in conflict management, dealing with problematic relationships tactfully, collaboration with the care team, the use of appropriate language, promoting a favourable atmosphere and redirecting each situation to try to make the doctor-patient relationship much smoother.</p><p id="par0190" class="elsevierStylePara elsevierViewall">Finally, after the above, we consider it necessary for medical students to learn about communication skills and management of situations in difficult patients<a class="elsevierStyleCrossRef" href="#bib0085"><span class="elsevierStyleSup">17</span></a> and, therefore, to place maximum emphasis on the fact that medical professionals are the ones who have to make the greatest effort to adequately care for patients with this profile through adequate training.<a class="elsevierStyleCrossRef" href="#bib0090"><span class="elsevierStyleSup">18</span></a></p></span><span id="sec0055" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0055">Funding</span><p id="par0195" class="elsevierStylePara elsevierViewall">The authors declare that there have been no external sources of funding.</p></span><span id="sec0060" class="elsevierStyleSection elsevierViewall"><span class="elsevierStyleSectionTitle" id="sect0060">Conflict of interests</span><p id="par0200" class="elsevierStylePara elsevierViewall">The authors declare that there is no conflict of interest.</p></span></span>" "textoCompletoSecciones" => array:1 [ "secciones" => array:10 [ 0 => array:2 [ "identificador" => "sec0005" "titulo" => "The doctor-patient encounter" ] 1 => array:2 [ "identificador" => "sec0010" "titulo" => "Difficult patient types" ] 2 => array:2 [ "identificador" => "sec0015" "titulo" => "They are not difficult patients" ] 3 => array:2 [ "identificador" => "sec0020" "titulo" => "Prevalence" ] 4 => array:2 [ "identificador" => "sec0025" "titulo" => "The care of difficult patients by their doctor" ] 5 => array:3 [ "identificador" => "sec0030" "titulo" => "Recommendations for the management of the difficult patient" "secciones" => array:3 [ 0 => array:2 [ "identificador" => "sec0035" "titulo" => "General strategies" ] 1 => array:2 [ "identificador" => "sec0040" "titulo" => "Special strategies" ] 2 => array:2 [ "identificador" => "sec0045" "titulo" => "The medical act" ] ] ] 6 => array:2 [ "identificador" => "sec0050" "titulo" => "Conclusions" ] 7 => array:2 [ "identificador" => "sec0055" "titulo" => "Funding" ] 8 => array:2 [ "identificador" => "sec0060" "titulo" => "Conflict of interests" ] 9 => array:1 [ "titulo" => "References" ] ] ] "pdfFichero" => "main.pdf" "tienePdf" => true "fechaRecibido" => "2020-05-21" "fechaAceptado" => "2020-07-06" "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">Please cite this article as: Bruguera M, Arimany-Manso J. Reflexiones sobre el paciente difícil. Med Clin (Barc). 2021;156:459–462.</p>" ] ] "multimedia" => array:1 [ 0 => array:8 [ "identificador" => "tbl0005" "etiqueta" => "Table 1" "tipo" => "MULTIMEDIATABLA" "mostrarFloat" => true "mostrarDisplay" => false "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at0005" "detalle" => "Table " "rol" => "short" ] ] "tabla" => array:1 [ "tablatextoimagen" => array:1 [ 0 => array:2 [ "tabla" => array:1 [ 0 => """ <table border="0" frame="\n \t\t\t\t\tvoid\n \t\t\t\t" class=""><tbody title="tbody"><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead rowgroup " rowspan="4" align="left" valign="middle">Groves, 1978<a class="elsevierStyleCrossRef" href="#bib0005"><span class="elsevierStyleSup">1</span></a></td><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t"><span class="elsevierStyleItalic">Dependent</span> "<span class="elsevierStyleItalic">clingers</span>" \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t"><span class="elsevierStyleItalic">Entitled demanders</span> \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t"><span class="elsevierStyleItalic">Manipulative help-rejecters</span> \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t"><span class="elsevierStyleItalic">Self-destructive deniers</span> \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " rowspan="6" align="left" valign="middle">Agreda y Yanguas, 2001<a class="elsevierStyleCrossRef" href="#bib0010"><span class="elsevierStyleSup">2</span></a></td><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Passive dependent \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Emotional seductive \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Masochist \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Psychosomatic patient \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Demanding aggressive \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Non-compliant denier \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " rowspan="15" align="left" valign="middle">Steinmetz and Tabenkin, 2001<a class="elsevierStyleCrossRef" href="#bib0015"><span class="elsevierStyleSup">3</span></a></td><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Violent, aggressive, verbally abusive. \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t"><span class="elsevierStyleItalic">Unresolved repeated complaints</span> \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Multiple complaints-<span class="elsevierStyleItalic">"shopping list"</span> \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Psychosomatic patients \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Complaining, never satisfied \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Seeking secondary gain \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Manipulative, lying \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">"Everything hurts" \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Having a high anxiety level \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t"><span class="elsevierStyleItalic">"Pain in the neck"</span> \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Demanding, boundary-busting, exploiting the doctor \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Angry at the doctor \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Uncooperative \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Difficult psychiatric patient \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Drug addict \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " rowspan="4" align="left" valign="middle">Hull and Broquet, 2007<a class="elsevierStyleCrossRef" href="#bib0065"><span class="elsevierStyleSup">13</span></a></td><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Angry, defensive, scared, or reluctant \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Manipulators \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Psychosomatic patients \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">In mourning \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " rowspan="7" align="left" valign="middle">Pons Diez, 2006<a class="elsevierStyleCrossRef" href="#bib0075"><span class="elsevierStyleSup">15</span></a></td><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Regressive \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Aggressive \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Stubborn \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Unmotivated \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">"Incurable" \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Dependents \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Frequenters \t\t\t\t\t\t\n \t\t\t\t</td></tr></tbody></table> """ ] "imagenFichero" => array:1 [ 0 => "xTab2586843.png" ] ] ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Classification of difficult patients according to the literature reviewed.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0005" "bibliografiaReferencia" => array:18 [ 0 => array:3 [ "identificador" => "bib0005" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Taking care of the hateful patient" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "J.E. Groves" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1056/NEJM197804202981605" "Revista" => array:6 [ "tituloSerie" => "N Engl J Med" "fecha" => "1978" "volumen" => "298" "paginaInicial" => "883" "paginaFinal" => "887" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/634331" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0010" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "El paciente difícil: quién es y cómo manejarlo" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "J. Agreda" 1 => "E. Yanguas" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "An Sist Sanit Navar" "fecha" => "2001" "volumen" => "24" "paginaInicial" => "65" "paginaFinal" => "72" ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0015" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "The’ difficult patient’ as perceived by family physicians" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "D. Steinmetz" 1 => "H. Tabenkin" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1093/fampra/18.5.495" "Revista" => array:6 [ "tituloSerie" => "Fam Pract" "fecha" => "2001" "volumen" => "18" "paginaInicial" => "495" "paginaFinal" => "500" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/11604370" "web" => "Medline" ] ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0020" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Actuación ante los pacientes de trato difícil" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "C. Blay" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "FMC" "fecha" => "1996" "volumen" => "4" "paginaInicial" => "243" "paginaFinal" => "250" ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0025" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "The difficult patient and the troubled physician" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "J.E. Crutcher" 1 => "M.J. Bass" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "J Fam Pract" "fecha" => "1980" "volumen" => "11" "paginaInicial" => "933" "paginaFinal" => "938" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/7452158" "web" => "Medline" ] ] ] ] ] ] ] ] 5 => array:3 [ "identificador" => "bib0030" "etiqueta" => "6" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Frustrating patients: physician and patient perspectives among distressed high users of medical services" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "E.H. Lin" 1 => "W. Katon" 2 => "M. Von Korff" 3 => "T. Bush" 4 => "P. Lipscomb" 5 => "J. Russo" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1007/BF02598969" "Revista" => array:6 [ "tituloSerie" => "J Gen Intern Med" "fecha" => "1991" "volumen" => "6" "paginaInicial" => "241" "paginaFinal" => "246" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/2066830" "web" => "Medline" ] ] ] ] ] ] ] ] 6 => array:3 [ "identificador" => "bib0035" "etiqueta" => "7" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Paciente conflictivo en urgencias: definición, tipología y aspectos éticos" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "B. Herreros" 1 => "G. García Casasola" 2 => "E. Pintor" 3 => "M.A. Sánchez" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.rce.2010.03.007" "Revista" => array:6 [ "tituloSerie" => "Rev Clin Esp" "fecha" => "2010" "volumen" => "210" "paginaInicial" => "404" "paginaFinal" => "409" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/20656286" "web" => "Medline" ] ] ] ] ] ] ] ] 7 => array:3 [ "identificador" => "bib0040" "etiqueta" => "8" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Trastorno de la personalidad: un desafío en la relación médico-paciente" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "R. Romero-Cabello" 1 => "I.C. González-Salas" 2 => "C. Javier Sánchez" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Atención Fam" "fecha" => "2016" "volumen" => "23" "paginaInicial" => "155" "paginaFinal" => "159" ] ] ] ] ] ] 8 => array:3 [ "identificador" => "bib0045" "etiqueta" => "9" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Valoración de la competencia de los pacientes para tomar decisiones" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "G.J. Palacios" 1 => "P. Pinto" 2 => "O. Marquez" 3 => "B. Herreros" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.rce.2019.04.009" "Revista" => array:6 [ "tituloSerie" => "Rev Clin Esp" "fecha" => "2019" "volumen" => "220" "paginaInicial" => "256" "paginaFinal" => "262" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/31345500" "web" => "Medline" ] ] ] ] ] ] ] ] 9 => array:3 [ "identificador" => "bib0050" "etiqueta" => "10" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "The ‘difficult patient’ as perceived by family physicians" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "D. Steinmetz" 1 => "H. Tabenkin" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1093/fampra/18.5.495" "Revista" => array:6 [ "tituloSerie" => "Fam Pract" "fecha" => "2001" "volumen" => "18" "paginaInicial" => "495" "paginaFinal" => "500" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/11604370" "web" => "Medline" ] ] ] ] ] ] ] ] 10 => array:3 [ "identificador" => "bib0055" "etiqueta" => "11" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Assessment of surgery residents’ interpersonal communication skills: validation evidence for the communication assessment tool in a simulation environment" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "A.W. Trickey" 1 => "A.B. Newcomb" 2 => "M. Porrey" 3 => "J. Wright" 4 => "J. Bayless" 5 => "F. Piscitani" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.jsurg.2016.04.016" "Revista" => array:6 [ "tituloSerie" => "J Surg Educ" "fecha" => "2016" "volumen" => "73" "paginaInicial" => "e19" "paginaFinal" => "e27" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/27216300" "web" => "Medline" ] ] ] ] ] ] ] ] 11 => array:3 [ "identificador" => "bib0060" "etiqueta" => "12" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "The role of the general practitioner’s affective behaviour in medical encounters" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "J. Bensing" 1 => "K. Schreurs" 2 => "A. De Rijk" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Psychol Health" "fecha" => "2007" "volumen" => "11" "paginaInicial" => "825" "paginaFinal" => "838" ] ] ] ] ] ] 12 => array:3 [ "identificador" => "bib0065" "etiqueta" => "13" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "How to manage difficult patient encounters" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "Sk Hull" 1 => "K. Broquet" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:6 [ "tituloSerie" => "Fam Pract Manag" "fecha" => "2007" "volumen" => "14" "paginaInicial" => "30" "paginaFinal" => "34" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/17598632" "web" => "Medline" ] ] ] ] ] ] ] ] 13 => array:3 [ "identificador" => "bib0070" "etiqueta" => "14" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Demanda y queja en la entrevista clínica, conceptos clave para una práctica clínica segura" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "F. Borrell i Carrió" 1 => "J.C. Hernández Clemente" 2 => "J. Lázaro" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Med Clin (Barc)" "fecha" => "2011" "volumen" => "137" "paginaInicial" => "216" "paginaFinal" => "220" ] ] ] ] ] ] 14 => array:3 [ "identificador" => "bib0075" "etiqueta" => "15" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "La comunicación entre el profesional de la salud y el paciente. Aspectos conceptuales y guía de aplicación" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:1 [ 0 => "X.P. Diez" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Enferm Integral" "fecha" => "2006" "volumen" => "73" "paginaInicial" => "27" "paginaFinal" => "34" ] ] ] ] ] ] 15 => array:3 [ "identificador" => "bib0080" "etiqueta" => "16" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Escuchar con atención al paciente aporta más de lo que cuesta" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:3 [ 0 => "J.J. Mira" 1 => "S. Lorenzo" 2 => "L.O. Perez-Jover" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Med Clin (Barc)" "fecha" => "2010" "volumen" => "135" "paginaInicial" => "477" "paginaFinal" => "478" ] ] ] ] ] ] 16 => array:3 [ "identificador" => "bib0085" "etiqueta" => "17" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Educationresearch: the medical student perspective on challenging conversations" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "R. Willis" 1 => "R.E. Strowd" 2 => "M.C. Barks" 3 => "R.E. Salas" 4 => "C.E. Gamaldo" 5 => "M.E. Lemmon" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1212/WNL.0000000000009261" "Revista" => array:2 [ "tituloSerie" => "Neu-rology" "fecha" => "2020" ] ] ] ] ] ] 17 => array:3 [ "identificador" => "bib0090" "etiqueta" => "18" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Il tocco, il rimedio, la parola: La comunicazione tramedico e paziente come strumento terapeutico" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:2 [ 0 => "R. Milanese" 1 => "S. Milanese" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Libro" => array:3 [ "fecha" => "2015" "editorial" => "Ponte Alle Grazie" "editorialLocalizacion" => "Milán" ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/23870206/0000015600000009/v1_202105020816/S2387020621001558/v1_202105020816/en/main.assets" "Apartado" => array:4 [ "identificador" => "44145" "tipo" => "SECCION" "en" => array:2 [ "titulo" => "Special article" "idiomaDefecto" => true ] "idiomaDefecto" => "en" ] "PDF" => "https://static.elsevier.es/multimedia/23870206/0000015600000009/v1_202105020816/S2387020621001558/v1_202105020816/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020621001558?idApp=UINPBA00004N" ]
Journal Information
Vol. 156. Issue 9.
Pages 459-462 (May 2021)
Share
Download PDF
More article options
Vol. 156. Issue 9.
Pages 459-462 (May 2021)
Special article
Reflections on the difficult patient
Reflexiones sobre el paciente difícil
Visits
7
This item has received
Article information
These are the options to access the full texts of the publication Medicina Clínica (English Edition)
Subscriber
Subscribe
Purchase
Contact
Phone for subscriptions and reporting of errors
From Monday to Friday from 9 a.m. to 6 p.m. (GMT + 1) except for the months of July and August which will be from 9 a.m. to 3 p.m.
Calls from Spain
932 415 960
Calls from outside Spain
+34 932 415 960
E-mail