Initiation of global vaccination significantly reduced the morbidity and mortality of COVID-19. During the Omicron wave, approximately 70% of the Israeli adult population was fully vaccinated, but the efficacy of the vaccine was questioned.
MethodsWe conducted a retrospective cohort study of all adult patients admitted to the COVID-19 departments in Rabin Medical Center, during the Delta wave and the Omicron wave. Patients were matched in the 2 waves using the inverse probability of treatment weighting (IPTW) method and risk for mechanical ventilation and 30-day all-cause mortality was assessed.
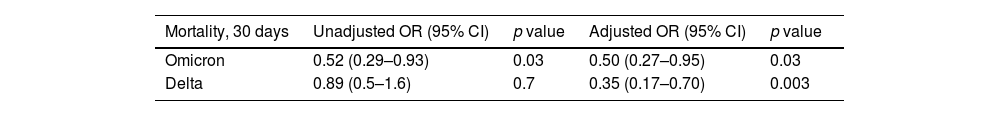
ResultsVaccination had a significant effect on 30-day mortality in the Delta and Omicron waves with adjusted OR of 0.35 (0.17–0.70) and 0.5 (0.27–0.95) respectively. Nonetheless, the rate of mechanical ventilation was similar between the groups with OR of 0.75 (0.52–1.09) and 0.64 (0.40–1.01). Vaccination status did not change the length of admission in both waves.
ConclusionWe observed a decreased risk for 30-day mortality among vaccinated patients during the Delta and Omicron waves in Israel. This association, even though consistent, was of a lesser magnitude during the Omicron wave.
La iniciación de la vacunación global redujo significativamente la morbilidad y la mortalidad de la COVID-19. Durante la ola de ómicron, aproximadamente 70% de la población adulta israelí estaba completamente vacunada, pero se cuestionó la eficacia de la vacuna.
MétodosRealizamos un estudio de cohorte retrospectivo de todos los pacientes adultos ingresados en los departamentos de COVID-19 en el Centro Médico Rabin, durante las olas de delta y ómicron. Los pacientes fueron emparejados en las dos olas utilizando el método de ponderación inversa de probabilidad de tratamiento (IPTW) y se evaluó el riesgo de ventilación mecánica y la mortalidad por todas las causas a los 30 días.
ResultadosLa vacunación tuvo un efecto significativo en la mortalidad a los 30 días en las olas de delta y ómicron con odds ratio (OR) ajustadas de 0,35 (0,17-0,70) y 0,5 (0,27-0,95), respectivamente. Sin embargo, la tasa de ventilación mecánica fue similar entre los grupos con OR de 0,75 (0,52-1,09) y 0,64 (0,40-1,01). El estado de vacunación no cambió la duración del ingreso en ambas olas.
ConclusiónObservamos un menor riesgo de mortalidad a los 30 días entre los pacientes vacunados durante las olas de delta y ómicron en Israel. Esta asociación, aunque constante, fue de menor magnitud durante la ola de ómicron.
The coronavirus disease 2019 (COVID-19), has emerged into our lives more than two years ago to become a pandemic affecting millions of people globally. In Israel, since the introduction of the SARS-CoV-2 BNT162b2 vaccine (BioNTech/Pfizer) in December 2020, over six million people were vaccinated with a second dose which accounts for more than 70% of the adult population 1. Despite the high rate of vaccination, at the beginning of the fifth SARS-CoV-2 wave in Israel, the efficacy of the BNT162b2 vaccine against the B.1.1.529 Omicron variant was questioned, and the burden of hospitalized patients was considerable 2. This study compares the characteristics and hospitalization outcomes of vaccinated versus unvaccinated patients during the Omicron and Delta waves in Israel.
MethodsWe conducted a retrospective cohort study of all adult patients admitted to the COVID-19 departments in Rabin Medical Center, during the Delta wave (May 1–September 30, 2021) and the Omicron wave (December 20, 2021–February 10, 2022). All included patients had a positive nasopharyngeal swab (SARS-CoV-2 PCR test) at presentation. Demographic, clinical, and laboratory data were collected from patients electronic medical records. Patients were considered vaccinated if they received at least two doses of the BNT162b2 covid-19 vaccine. Patients with unknown vaccination status were not included in the analysis. Categorical variables were compared using χ2 test. Continuous variables were compared using Mann–Whitney U test. We used the inverse probability of treatment weighting (IPTW) method to be vaccinated in each wave to adjust for patients characteristics and known risk factors for the outcomes of mechanical ventilation and 30-day all-cause mortality. The study was approved by the ethics committee of Rabin Medical Center.
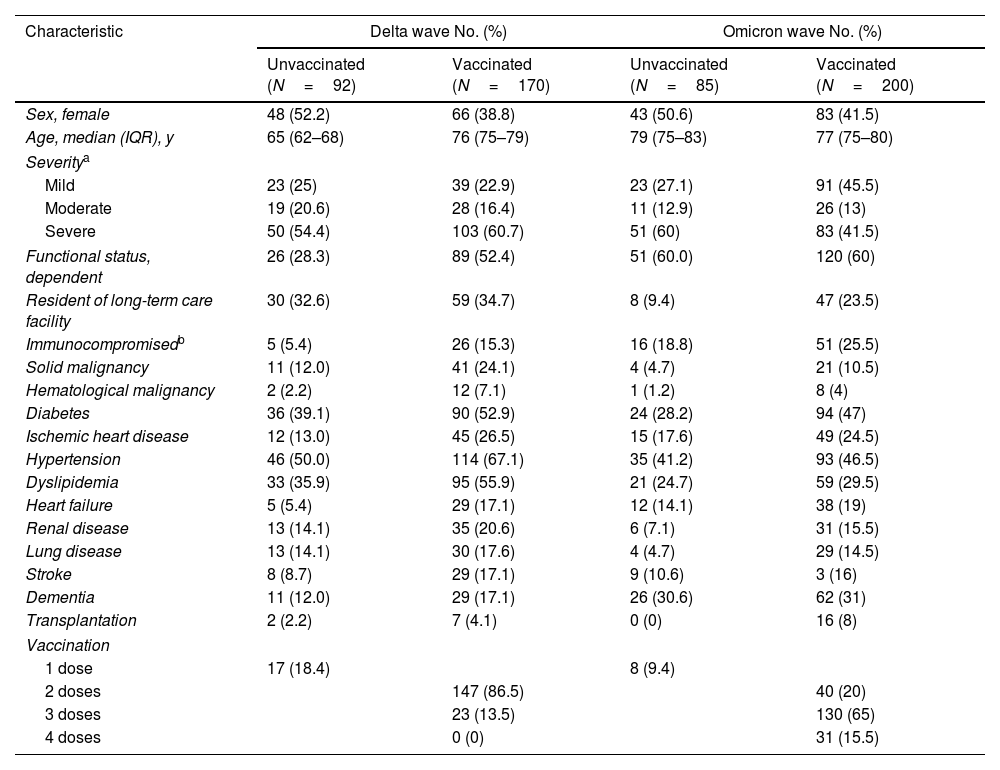
ResultsDuring the Omicron wave, 298 patients were admitted due to COVID-19 infection. Patients median age was 79 (IQR 65–85), the majority were male (162, 54.3%) and 72 (24.1%) were residents of a long-term care facility. Most patients had comorbidities (208, 69.7%) including hypertension (130, 43.6%), diabetes Mellitus (119, 40%), and ischemic heart disease (65, 21.8%). Immunosuppression was present in 56 patients (18.8%) mostly due to chronic use of corticosteroids. In this wave, 209 (70.2%) were vaccinated, 77 (25.8%) were considered unvaccinated and 12 (4%) had unknown vaccination status (Table 1). Among vaccinated patients, 28 (13.4%) were mechanically ventilated and 42 (20.1%) had died compared to 16 (20.8%) mechanically ventilated and 25 (32.5%) deaths in the unvaccinated. For vaccinated, the adjusted OR (95%CI) for mechanical ventilation was 0.64 (0.40-1.01) and the adjusted OR (95%CI) for 30 days mortality was 0.50 (0.27-0.95) (Table 2). The median length of hospital stay was 4 days (IQR 2-7) with no significant difference according to vaccination status.
Characteristics of hospitalized patients according to vaccination status.
| Characteristic | Delta wave No. (%) | Omicron wave No. (%) | ||
|---|---|---|---|---|
| Unvaccinated (N=92) | Vaccinated (N=170) | Unvaccinated (N=85) | Vaccinated (N=200) | |
| Sex, female | 48 (52.2) | 66 (38.8) | 43 (50.6) | 83 (41.5) |
| Age, median (IQR), y | 65 (62–68) | 76 (75–79) | 79 (75–83) | 77 (75–80) |
| Severitya | ||||
| Mild | 23 (25) | 39 (22.9) | 23 (27.1) | 91 (45.5) |
| Moderate | 19 (20.6) | 28 (16.4) | 11 (12.9) | 26 (13) |
| Severe | 50 (54.4) | 103 (60.7) | 51 (60) | 83 (41.5) |
| Functional status, dependent | 26 (28.3) | 89 (52.4) | 51 (60.0) | 120 (60) |
| Resident of long-term care facility | 30 (32.6) | 59 (34.7) | 8 (9.4) | 47 (23.5) |
| Immunocompromisedb | 5 (5.4) | 26 (15.3) | 16 (18.8) | 51 (25.5) |
| Solid malignancy | 11 (12.0) | 41 (24.1) | 4 (4.7) | 21 (10.5) |
| Hematological malignancy | 2 (2.2) | 12 (7.1) | 1 (1.2) | 8 (4) |
| Diabetes | 36 (39.1) | 90 (52.9) | 24 (28.2) | 94 (47) |
| Ischemic heart disease | 12 (13.0) | 45 (26.5) | 15 (17.6) | 49 (24.5) |
| Hypertension | 46 (50.0) | 114 (67.1) | 35 (41.2) | 93 (46.5) |
| Dyslipidemia | 33 (35.9) | 95 (55.9) | 21 (24.7) | 59 (29.5) |
| Heart failure | 5 (5.4) | 29 (17.1) | 12 (14.1) | 38 (19) |
| Renal disease | 13 (14.1) | 35 (20.6) | 6 (7.1) | 31 (15.5) |
| Lung disease | 13 (14.1) | 30 (17.6) | 4 (4.7) | 29 (14.5) |
| Stroke | 8 (8.7) | 29 (17.1) | 9 (10.6) | 3 (16) |
| Dementia | 11 (12.0) | 29 (17.1) | 26 (30.6) | 62 (31) |
| Transplantation | 2 (2.2) | 7 (4.1) | 0 (0) | 16 (8) |
| Vaccination | ||||
| 1 dose | 17 (18.4) | 8 (9.4) | ||
| 2 doses | 147 (86.5) | 40 (20) | ||
| 3 doses | 23 (13.5) | 130 (65) | ||
| 4 doses | 0 (0) | 31 (15.5) | ||
Unadjusted and adjusted association between vaccination and 30 days mortality during the omicron and delta waves.
| Mortality, 30 days | Unadjusted OR (95% CI) | p value | Adjusted OR (95% CI) | p value |
|---|---|---|---|---|
| Omicron | 0.52 (0.29–0.93) | 0.03 | 0.50 (0.27–0.95) | 0.03 |
| Delta | 0.89 (0.5–1.6) | 0.7 | 0.35 (0.17–0.70) | 0.003 |
a Models were adjusted using IPTW for Age, Sex, Functional status, Dementia, Diabetes, Renal disease, Lung disease, Hypertension, Dyslipidemia, Ischemic heart disease, Heart failure, Stroke, Solid malignancy, Immunocompromised conditions.
During the Delta wave, 269 patients were admitted due to COVID-19 infection. Patients median age was 73 (IQR 63-81), the majority were male (155, 57.6%) and 89 (33%) were residents of a long-term care facility. Most patients had comorbidities (222, 82.5%) including hypertension (160, 59.5%), diabetes Mellitus (126, 46.8%), and ischemic heart disease (57, 21.1%). Immunosuppression was present in 31 patients (11.5%) mostly due to chronic use of corticosteroids. In this wave, 187 patients (69.5%) were vaccinated, 75 (27.9%) were considered unvaccinated and 7 (2.6%) had unknown vaccination status. Among vaccinated patients, 62 (33.2%) were mechanically ventilated and 53 (28.3%) had died compared to 28 (37.3%) mechanically ventilated and 23 (30.7.%) deaths in the unvaccinated. For vaccinated, the adjusted OR (95%CI) for mechanical ventilation was 0.75 (0.52–1.09) and the adjusted OR (95%CI) for 30 days mortality was 0.35 (0.17–0.70) (Table 2). The median length of hospital stay was 4 days (IQR 2–8) with no significant difference according to vaccination status.
DiscussionIn this study of hospitalized SARS-CoV-2 infected patients we observe a decreased risk for 30-day mortality among vaccinated patients. This association, even though consistent in both waves, was of a lesser magnitude during the Omicron wave. Our observation aligns with previous studies evaluating vaccine effectiveness and may be the result of immune evasion of the Omicron variant 2,3. Another possible explanation could be the waning vaccine effectiveness and decreased immunogenicity over time 4,5. Our study has several limitations. It was a single center with an observational design. Due to the small amount of missing data, we excluded patients with unknown vaccination status from the final analysis. At the end of 2022, the CDC published a recommendation for 3rd “booster” vaccine. In our study, we defined vaccinated as patients who received at least two doses of the BNT162b2 vaccine. We chose to do so since this recommendation was not present during the Delta wave. Despite the incompatibility between the current recommendation, we believe that the inclusion of patients after two doses strengthen our results of good outcome among vaccinated patients. In conclusion our result show that vaccinated COVID-19 hospitalized patients had a decreased risk for 30-day mortality in both the Omicron and Delta waves.
Role of funder/SponsorNot relevant.
Funding/SupportNo external funding.
Conflict of interestNone
We would like to thank Mr. Dean Sharon for his assistance in writing the article.