Several studies have analyzed the influence of meteorological and geographical factors on the incidence of COVID-19. Seasonality could be important in the transmission of SARS-CoV-2. This study aims to evaluate the geographical pattern of COVID-19 in Spain and its relationship with different meteorological variables.
MethodsA provincial ecological study analyzing the influence of meteorological and geographical factors on the cumulative incidence of COVID-19 in the 52 (24 coastal and 28 inland) Spanish provinces during the first three waves was carried out. The cumulative incidence was calculated with data from the National Statistical Institute (INE) and the National Epidemiological Surveillance Network (RENAVE), while the meteorological variables were obtained from the Spanish Meteorological Agency (AEMET).
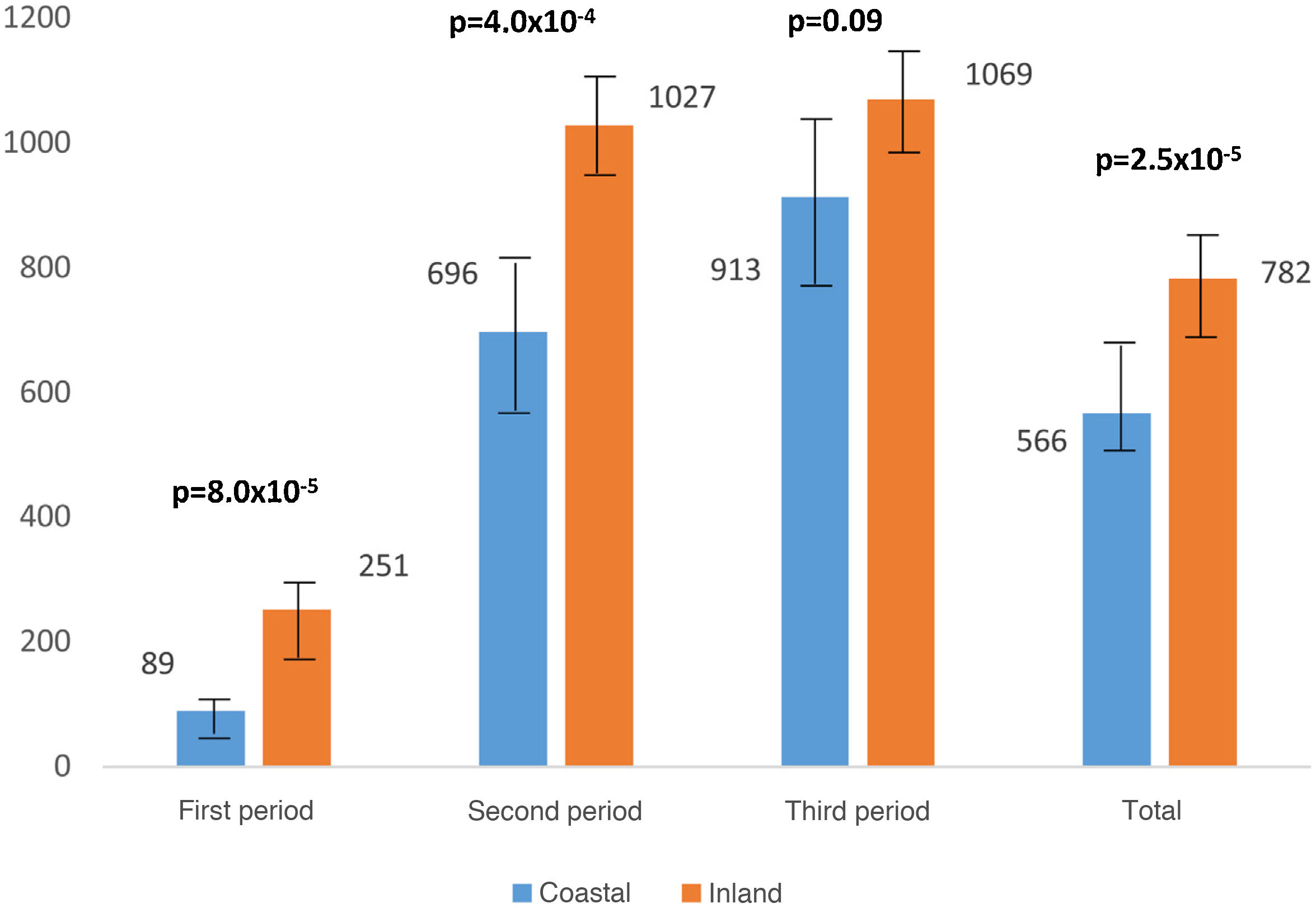
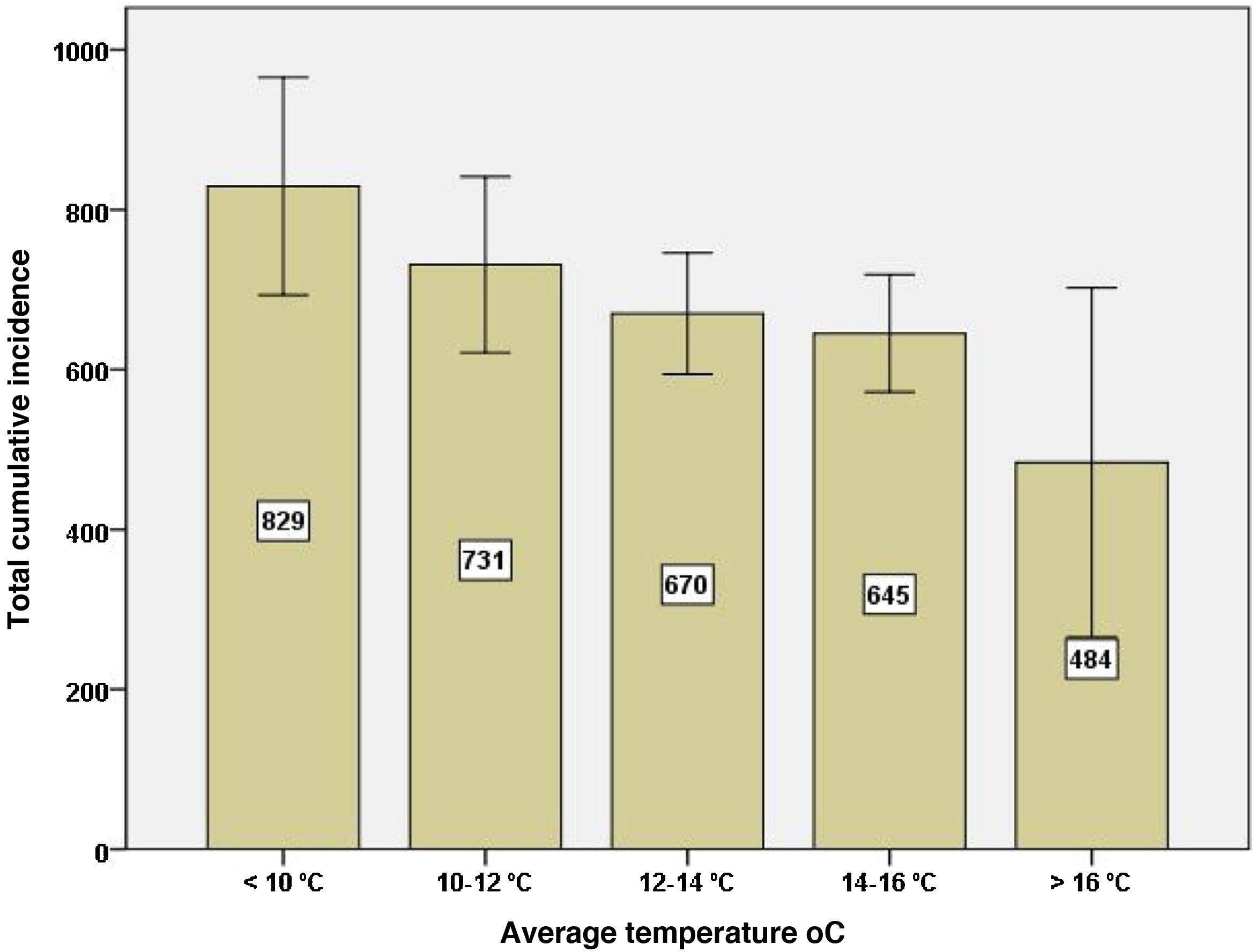
ResultsThe total cumulative incidence, in all three waves, was lower in the coastal provinces than in the inland ones (566 ± 181 vs. 782 ± 154; P = 2.5 × 10−5). The cumulative incidence correlated negatively with mean air temperature (r = −0.49; P = 2.2 × 10−4) and rainfall (r = −0.33; P = .01), and positively with altitude (r = 0.56; P = 1.4 × 10−5). The Spanish provinces with an average temperature <10 °C had almost twice the cumulative incidence than the provinces with temperatures >16 °C. The mean air temperature and rainfall were associated with the cumulative incidence of COVID-19, regardless of other factors (Beta Coefficient of −0.62; P = 3.7 × 10−7 and −0.47; P = 4.2 × 10−5 respectively)
ConclusionsMeteorological and geographical factors could influence the evolution of the pandemic in Spain. Knowledge regarding the seasonality of the virus would help to predict new waves of COVID-19 infections
Varios estudios han analizado la influencia de factores meteorológicos y geográficos en la incidencia de COVID-19. La estacionalidad podría tener importancia en la transmisión de SARS-CoV-2. Nuestro estudio evalúa el patrón geográfico de la COVID-19 en España y su relación con las distintas variables meteorológicas.
MétodosEstudio ecológico a escala provincial que analiza la influencia de factores meteorológicos y geográficos en la incidencia acumulada de COVID-19 en las 52 provincias españolas (24 costeras y 28 del interior) durante las tres primeras olas. La incidencia acumulada se calculó con los datos del Instituto Nacional Estadística (INE) y la Red Nacional de Vigilancia Epidemiológica (RENAVE), las variables meteorológicas se obtuvieron de la Agencia estatal de meteorología (AEMET).
ResultadosLa incidencia acumulada total, en los tres periodos, fue menor en las provincias costeras que en las del interior (566 ± 181 vs. 782 ± 154; P = 2,5 × 10−5). La incidencia acumulada correlacionó negativamente con la temperatura media (r = −0,49; P = 2,2 × 10−4) y las precipitaciones (r = −0,33; P = ,01), y positivamente con la altitud (r = 0,56; P = 1,4 × 10−5). Las provincias españolas con una temperatura media <10 °C tuvieron casi el doble de incidencia acumulada que las provincias con temperaturas >16 °C. La temperatura media y las precipitaciones fueron las variables asociadas con la incidencia acumulada provincial de COVID-19, con independencia de otros factores (Coeficiente Beta de −0,62; P = 3,7 × 10−7 y −0,47; P = 4,2 × 10−5 respectivamente).
ConclusionesLos factores meteorológicos y geográficos podrían influir en la evolución de la pandemia en España. El reconocimiento de la estacionalidad del COVID-19 ayudaría a predecir nuevas olas.
Several studies have analysed the influence of climate and geographical factors on the incidence of COVID-19.1–4 Seasonality, described for other respiratory viruses,5,6 could also play a role in the transmission of SARS-CoV-2.7–10 This temporal pattern seems to be attributed more to environmental factors than to changes in the genomic composition of the virus.11 Weather variables could be responsible for the differences found in the incidence of SARS-CoV-2.3,4 In fact, changes in temperature affect the viability of viruses,12 alter the mucociliary barrier and modify the host's innate and adaptive immune response.13 SARS-CoV-2 transmission appears to decrease in warm, humid conditions, while it increases in cold, dry air.8,14
Spain is one of the European countries most affected by the pandemic with more than 3,780,000 infections and 80,750 deaths (June 2021). The National Sero-Epidemiology Study on SARS-COV-2 infection (ENE-COVID), conducted between 27 April and 11 May 2020 in 61,000 people in 35,883 Spanish households, showed clear geographical differences in the seroprevalence rate, with lower immunisation in coastal areas (<3%) compared to areas near Madrid (>10%).15 This fact seemed to translate into geographical differences in the incidence of COVID-19 between coastal and inland regions of the Iberian Peninsula. Therefore, our study aims to carry out a spatial analysis of the cumulative incidence of COVID-19 in the different Spanish regions, determining the influence of the geographical coast/inland and weather factor on the spread of SARS-CoV-2.
MethodsEcological study at provincial level carried out during three periods defined by the peak incidence of COVID-19 in Spain. The first period was from March to May 2020, the second from September to November 2020 and the third from December to February 2021. Demographic data were obtained from the INE (National Statistics Institute) on the number of inhabitants in each of the 52 provinces and the provincial population density (inhabitants/km2).
Weather dataThe weather variables were obtained from the Spanish Meteorological Agency (AEMET) corresponding to 870 weather stations on a monthly scale. The data from all the stations located in each province were averaged. The variables analysed were the mean temperature in Celsius (°C), relative humidity as a percentage ratio (%) between the amount of water vapor contained in the air and the maximum amount it can contain at a given pressure and temperature, rainfall amount measured in millimetres of depth of water (mm), wind speed (km/h), wind calm percentage (percentage of days of the month in which there was no wind with a specific direction) and provincial altitude in metres (m).
COVID-19 incidence dataThe cases detected in each province were obtained from the National Epidemiological Surveillance Network (RENAVE) through the web-based computer platform SiViES (Spanish Surveillance System) managed by the National Epidemiology Centre (CNE). The date of symptom onset or, alternatively, six days prior to diagnosis (from the start of the pandemic until 10 May) or three days prior to diagnosis (from 11 May onwards) was used to calculate the cumulative incidence. The date of diagnosis was used for asymptomatic cases. Until 10 May 2020, cases diagnosed by a positive diagnostic test for active infection were included, as well as all hospitalised cases, intensive care unit (ICU) admissions and deaths; as from 11 May 2020, only cases confirmed by polymerase chain reaction (PCR), or antigen testing were included.
The province's population used for the calculation of the incidence rate comes from the official population figures derived from the revision of the INE's municipal census as of 1 January 2019. To calculate the cumulative incidence (CI) by province in each of the months of the study, new cases in the specified time period were estimated among the population at risk (population of the province).
The analysis of the data was carried out in the 52 Spanish provinces, 24 coastal provinces with access to the sea and 28 inland (Appendix B Annex 1) for each of the periods and for the total (mean of the three periods). The recommendations of the STROBE guidelines were followed for the publication of this study.16
Statistical analysisData were expressed as mean and standard deviation (SD). The distribution of quantitative variables was analysed with the Kolmogorov-Smirnov test. The Student's t-test or the Mann-Whitney test was used for the comparison of quantitative variables, while the Chi2 test or Fisher's test was used for qualitative variables. The Pearson or Spearman (Rho) correlation was used to study the relationship between quantitative variables. A univariate and multivariate multiple linear regression analysis was performed. For hypothesis testing, a value of P < .05 was considered statistically significant. All data were analysed with the statistical software SPSS (Statistical Package for Social Sciences, Chicago, IL, USA).
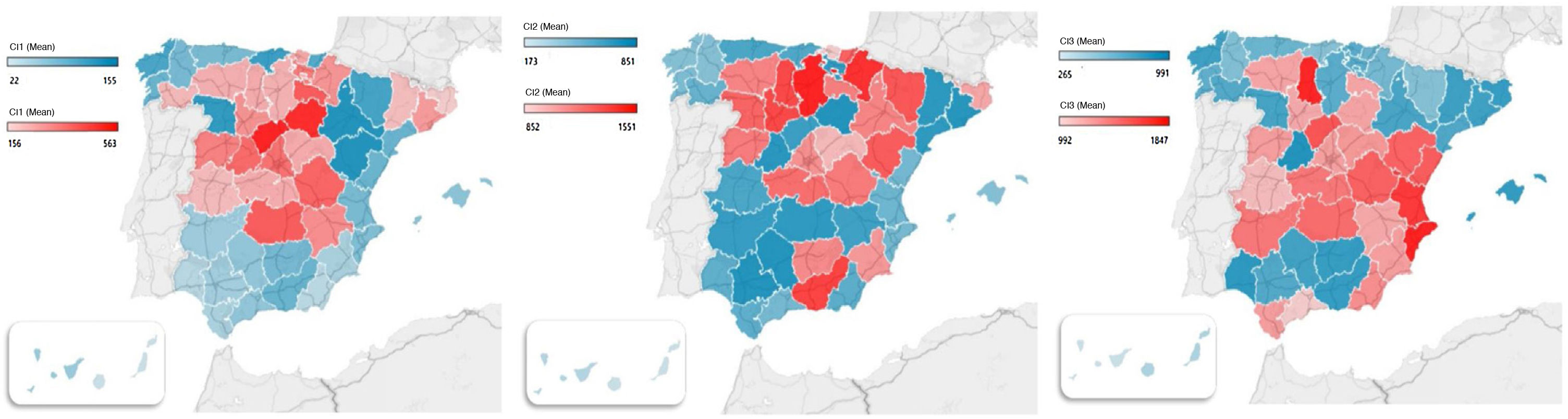
ResultsThe Spanish population (47,026,208 inhabitants; 51% women and 49% men) is divided into 52 provinces, 24 coastal provinces (with access to the sea) and 28 inland provinces (Appendix A Annex 1). The coastal provinces registered a lower CI of COVID-19 despite having a higher population density. CI in the first period (March–May) was 89 (61) cases in coastal provinces and 251 (138) in inland provinces (P = 8.0 × 10−5). In the second period (September–November) out of 696 (341) and 1027 (271) cases, respectively (P = 4,0 × 10−4), and in the third period (December–February) of 913 (390) vs. 1. 069 (319) cases (P = .09). Table 1 shows the CI data by periods and months. The geographic distribution of CI in the three periods, by province, is shown in Fig. 1.
Cumulative incidence in the coastal and inland provinces.
| Coastal provinces | Inland provinces | P | |
|---|---|---|---|
| n = 24 | n = 28 | ||
| Population of provinces | 1,172,472 (1,103,488) Median 982,732 | 674,531 (1,229,133) Median 372,562 | .0003* |
| Population of provincial capitals | 330,453 (350,285) Median 202,922 | 277,068 (608,183) Median 118,651 | .70 |
| Population density (inhab/km2) | 210 (165) | 67 (153) | 5.6 × 10−7* |
| Provincial altitude in meters | 289 (161) | 743 (229) | 4.5 × 10−8* |
| CI First period | |||
| March | 177 (102) | 503 (315) | 1.5 × 10−5* |
| April | 75 (71) | 209 (105) | 1.1 × 10−5* |
| May | 14 (18) | 41 (28) | 7.3 × 10−4* |
| Total | 89 (61) | 251 (138) | 8.0 × 10−5* |
| CI Second period | |||
| September | 399 (195) | 773 (307) | 2.1 × 10−5* |
| October | 903 (611) | 1347 (430) | .001* |
| November | 785 (325) | 962 (342) | .064 |
| Total | 696 (341) | 1027 (271) | 4.0 × 10−4* |
| CI Third Period | |||
| December | 571 (289) | 570 (234) | .99 |
| January | 1668 (911) | 2113 (789) | .06 |
| February | 500 (182) | 525 (227) | .66 |
| Total | 913 (390) | 1069 (319) | .09 |
Mean and standard deviation (SD). CI: cumulative incidence.
Total CI was also lower in the coastal provinces (566 ± 181 cases, compared to 782 ± 154 inland; P = 2.5 × 10−5) (Fig. 2). Las Palmas de Gran Canaria, Santa Cruz de Tenerife and Lugo were the provinces with the lowest total CI (173, 177 and 344 cases), while Palencia, Cuenca and Teruel were the provinces with the highest total CI (1,143, 1018 and 981, respectively). Below the median total CI (691 cases), 69% were coastal provinces, while above 77% were inland.
As for weather factors, the coastal provinces had higher average temperatures in the three periods (2.2 °C in the first period, 3.3 °C in the second and 5 °C in the third) and also higher relative humidity in the first two periods (3% and 4%, respectively) (Table 2). The rest of the weather variables studied, rainfall, wind speed and percentage of calm, showed no significant differences.
Weather factors in coastal and inland provinces by periods.
| Coastal provinces | Inland provinces | P | |
|---|---|---|---|
| n = 24 | n = 28 | ||
| Average temperature °C: | |||
| 1P | 15.4 (1.7) | 13.2 (1.7) | 1.9 × 10−5* |
| 2P | 17.5 (2.4) | 14.2 (2.2) | 3.5 × 10−6* |
| 3P | 10.8 (2.5) | 6.4 (1.8) | 1.1 × 10−7* |
| Total | 14.5 (2.1) | 11.2 (1.8) | 3.0 × 10−6* |
| Relative humidity % | |||
| 1P | 70 (5) | 67 (3) | .005** |
| 2P | 70 (6) | 66 (5) | .01** |
| 3P | 73 (7) | 78 (3) | .14 |
| Total | 71 (6) | 70 (3) | .49 |
Mean and standard deviation (SD).
The total province CI, in the three periods, correlated negatively with the mean temperature recorded in the provinces (Pearson's r: −0.51; P = 8.0 × 10−5). The mean temperature was able to explain 26% of the total variability of the CI in the three periods (linear R2: 0.26).
Total CI was also negatively correlated with rainfall (Pearson's r: −0.34; P = .01) and positively with altitude (Pearson's r: 0.52; P = .0007). The rest of the variables studied (humidity, wind speed and calm percentage) showed no correlation.
Changes in total CI according to changes in temperature are shown in Fig. 3. Provinces with an average temperature <10 °C recorded almost twice as much total CI as provinces with temperatures >16 °C.
Univariate linear regression analysis showed that the location of the province (coastal/inland), altitude, mean temperature and rainfall were associated with the provincial total CI (Table 3). The multivariate linear regression analysis (total CI dependent variable; independent variables were those that showed statistical significance in the univariate analysis) showed an independent negative relationship between mean temperature/rainfall and COVID-19 CI (Table 3). The standardized beta coefficients for mean temperature and rainfall were −0.62 and −0.47, respectively.
Univariate and multivariate linear regression analysis. Dependent variable: cumulative incidence in the three periods.
| Univariate | Multivariate | |
|---|---|---|
| Unstandardized Beta coefficient (95% CI) P | Unstandardized Beta coefficient* (95% CI) P | |
| Province (coastal/inland) | 216 (122–310) | – |
| P = 2.5 × 10−5 | ||
| Provincial altitude (m) | 0.3 (0.1–0.5) | – |
| P = 7.4 × 10−5 | ||
| Population density (inhab/km2) | −0.24 (−0.57 to 0.08) | |
| P = .13 | ||
| Average temperature (ºC) | −39 ([−57] to [−20]) | −47 ([−63] to [−31]) |
| P = 8.7 × 10−5 | P = 3.7 × 10−7 | |
| RH (%) | −10 (−21 to 1.1) | |
| P = .08 | ||
| Rainfall (mm) | −1.7 ([−3.0] to [−0.3]) | −2.4 ([−3.4] to [−1.3]) |
| P = 1.0 × 10−two | P = 4.2 × 10−5 | |
| Wind speed (km/h) | −2.4 (−32 to 27) | |
| P = .86 | ||
| % wind calm | −2.8 (−17 to 11.7) | |
| P = .69 |
Our study shows that factors related to weather and geography have an influence on the CI of COVID-19 in Spain. Specifically, the average temperature influenced the CI of COVID-19 in the Spanish provinces; for example, those with low temperatures had a higher CI, regardless of other factors studied, and conversely, those with higher temperatures had a lower incidence. The influence of temperature on provincial incidence rates is consistent, as it is observed in the first three waves recorded in our country and throughout the different seasons (spring, autumn and winter). We found that the provinces with average temperatures below 10 °C had twice the cumulative incidence of that recorded in the provinces with more than 16 °C. As in our analysis, several studies have found that temperature may be related to the incidence of COVID-19.17,18 Between 26 January and 29 February 2020, a negative correlation was described between CI and mean temperature in Wuhan (R2 = 0.126; P < .05).19 Another study in 166 countries (excluding China) found a daily reduction of 3.08% in cases of COVID-19 and 1.19% in deaths with the rise of 1 °C in temperature.20 An ecological study carried out in the Spanish autonomous communities between 15 March and 22nd April 2020 described a negative correlation between CI and mean temperature (r = −0.77; P < .0001), such that a 10% decrease in mean temperature increased CI by 14.6%.21 In the USA, 90% of COVID-19 cases have been reported in states with temperatures below 17 °C.22 Other authors, however, do not find a relationship23 or, on the contrary, they describe an increase in cases with the increase in maximum temperature.24 In addition, the relationship between temperature and incidence of COVID-19 may not be linear.25 Our study establishes a negative association between total CI and mean temperature, with a temperature range from 8.7 °C to 19.0 °C, so we do not know the effect of “more extreme” temperatures on the incidence of COVID-19. Changes in temperature can affect the viability of the virus and the immune response of the individual.26,27 Temperature also influences social habits, as low temperatures favour meeting indoors, without proper ventilation, which increases the risk of SARS-CoV-228 transmission, while higher temperatures favour going out in open spaces.
Rainfall also influenced the provincial CI in our study, in such a way that those provinces that recorded more rainfall (mm) were those with the lowest CI. Rain could help reduce air pollution, thus reducing the incidence of COVID-19.29 In fact, the absence of rain has been linked to an increase in the incidence of COVID-19 in nearby countries (Italy).30 Other studies, however, do not describe an influence of rainfall in cities such as Rio de Janeiro (April 2020)31 o New York (March–April 2020).1 Rainfall is directly related to relative humidity (in fact, the correlation in our study was 0.77), which is also a weather factor related to the transmission of respiratory viruses.32 A low percentage of humidity in the air (i.e., dry and cold air) could favour the persistence of aerosols and increase the incidence of COVID-19.33 The anticyclonic, dry atmospheric conditions in south-western Europe in February 2020 may have favoured the rapid spread of the virus in Italy and Spain at the onset of the pandemic.34
Increased relative humidity has been associated with a 0.85% (95% CI 0.51%–1.19%) reduction in new cases and 0.51% (95% CI 0.34%, 0.67%) reduction in deaths from the disease.20 As with temperature, humidity may be suggestive of a “sweet point” for SARS-CoV-2 transmission.24 A study in 206 regions and countries worldwide finds that 75% of cases are in an absolute humidity range of 5−10 g/m24 as 90% of cases in the USA are described in ranges of 4−9 g/m.22 However, other studies, like ours, find no association.35 On the other hand, wind speed and calm spells do not seem to influence the geographical differences found. Wind has been linked to COVID-19 transmission by reducing airborne SARS-CoV-2 pollution and suspension.36 A study in Indonesia describes a negative correlation between wind and incidence of COVID-19 (r = −0.31; P < .05).37
In our study, the provincial incidence rates of COVID-19 in Spain were also determined by geographic factors, such as the location of the province and its altitude. The coastal provinces, despite having a higher population density, had lower CI than the inland provinces. We think that this fact is mediated by temperature, which was higher in the coastal provinces, since it was ultimately the meteorological factor that was most clearly associated with the CI of COVID-19. Similarly, we can see that the provinces with higher altitudes (those inland) had a greater incidence, but likewise, the rise in altitude implies a drop in temperature, so ultimately temperature would also explain it. Several studies relate altitude to COVID-1910,11,38 incidence and mortality, although other studies do not describe it39 or, on the contrary, highlight a lower incidence in populations at higher altitudes, perhaps due to the difficulty in gaining access to them and the lower population density.40 Altitude-induced hypoxia could also lead to a lower expression of angiotensin-converting enzyme 2 (ACE2), the gateway for the virus to enter the cell,41 although studies are contradictory.42
Our work has several limitations as it is an ecological study, carried out on a provincial level. Furthermore, although we adjusted for different variables in the multivariate analysis, the association found does not imply causality. On the other hand, we do not know the influence of other environmental factors, such as pollution, which could affect virus transmission,43,44 or ultraviolet radiation, which could have an effect on COVID-19, partly mediated by vitamin D synthesis.45 Vitamin D regulates the expression of numerous genes involved in the immune response and its deficiency has been linked to the development of viral respiratory infections46 and SARS-CoV-2.47,48
In conclusion, we consider that weather and geographical factors could influence the evolution of the pandemic in Spain, especially due to changes in temperature. Recognising the seasonality of COVID-19 would help to predict new waves and adapt prevention campaigns.
AcknowledgmentsThank the advice and collaboration of the AEMET-Cantabria staff.