As early as 1974, telehealth was being discussed as a link between hospitals and homes.1 There were few publications on the subject until 1992, the turning point when publications on this model started to emerge. Face-to-face interactions will always play a central role in our healthcare system. But a system based on high-quality remote care might work better for many patients and quite possibly for some doctors as well.2 Since the advent of SARS-CoV-2, telehealth has become a useful tool in certain healthcare systems.3 This disruptive experience has meant a sudden and total shift from face-to-face consultations to a virtual model, unprecedented in many health systems.
Our department implemented a comprehensive telecardiology model from 16th March until 1st May, time when we progressively returned to face-to-face activity. We do not yet have a specific tool, therefore, the model relied on two simple pillars, the electronic medical record and the telephone call as a means of communication with users and colleagues.
A total of 1721 teleconsultations were carried out, of which 1339 came from general consultations, 67 from the cardiac rehabilitation consultation and 315 from the monographic consultation on Advanced Heart Failure.
For the analysis of the results we propose 3 possibilities: (1) follow-up (it is resolved by teleconsultation and requires a check-up/complementary test); (2) resolved (it is resolved by teleconsultation without the need for further follow-up) and (3) re-appointment (requires a face-to-face visit).
Of the total of 1721 patients contacted by teleconsultation, 1156 (67.2%) were referred for a follow-up, 332 (19.3%) were resolved and only 233 (13.5%) required re-appointment
We analysed general consultations due to their greater volume (1339 patients), differentiating two tasks: first visits (315 patients) and follow-up visits (1024 patients). Of the first-visit patients, 18.1% were referred for a follow-up, 16.2% were resolved and 65.7% required a face-to-face visit. Of the follow-up group, 74.6% were doing a check-up, 25.3% were resolved and only 0.1% required a face-to-face visit.
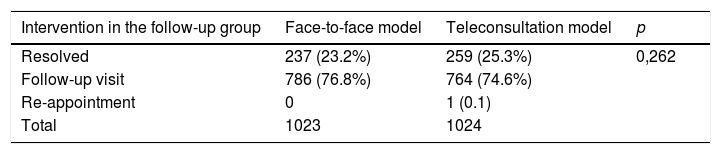
Despite the technical limitations, the percentage of resolutions of first-visit patients was not negligible (34.3%) but without a doubt, what was striking was the resolution capacity of almost 100% of the patients in the follow-up group. This data led us to perform a comparative analysis with the face-to-face model of 1023 review patients seen in the 7 weeks prior to the start of the teleconsultation model. Of these 1023 patients seen in person, 237 (23.2%) were resolved and 786 (76.8%) went for a follow-up visit (Table 1). We did not observe statistically significant differences in the outcomes of the follow-up group when the face-to-face model was compared to teleconsultation (p = 0.262).
Finally, we compared the number of patients who did not come to the face-to-face consultation (167, 12.5%) versus the number of patients who did not respond to the phone call (42, 3.1%), observing a statistically significant difference (p < 0.001).
Although we are aware of the need for longer-term comparative studies evaluating the results of teleconsultation, telehealth interventions generally seem equivalent to face-to-face care.4 This healthcare modality is promising and has adequate resolution rates for a specific group of patients, such as those under follow-up for stable chronic diseases and those who come to the clinic to collect results. For this reason, it is vitally important to invest in and develop platforms that allow effective communication between healthcare levels and between healthcare providers-patients because, without a doubt, telehealth will be part of our daily healthcare work.
Conflict of interestsThe authors declare no conflict of interest.
Please cite this article as: Isasti G, Díaz Fernández JF. Comparación de la teleconsulta con el modelo presencial tradicional durante la pandemia COVID-19. Med Clin (Barc). 2020;155:361–362.