To examine the relationships between of four measures of adiposity, namely waist circumference (WC), body mass index (BMI), and subscapular and abdominal skinfolds, with different cardiovascular risk factors in prepubertal children.
MethodsFour hundred and ninety-four prepubertal children aged 6–10 years participated in this cross-sectional study. The subscapular and abdominal skinfolds, WC, and BMI were measured to assess adiposity, and cardiovascular risk factors (CVRFs) were assessed by measuring systolic (SBP) and diastolic blood pressures (DBP), glucose, triglycerides (TG), and high density (HDL-C) and low density lipoprotein cholesterol (LDL-C). Dichotomous variables were created based on whether or not the subjects were in the upper quartile (Q4) for the WC, BMI, and skinfold variables.
ResultsNo CVRF was found in 52.8% of children, 33.4% had one factor, and 10.9% and 2.8% had 2 and 3 factors respectively. An adjusted logistic regression analysis showed that being in Q4 of anthropometric variables and CVRFs was associated to TG levels ≥ 100mg/dL. Glucose levels ≥96mg/dL were associated to Q4 and abdominal fold. Presence of 2 or more CVRFs was significantly associated to Q4 in all anthropometric variables despite adjustment for age, gender, and calorie intake. The subscapular skinfold was the adiposity marker associated to the highest risk.
ConclusionsChildren with a more unfavorable adiposity profile tend to have a greater cardiovascular risk in the prepubertal stage.
Examinar las asociaciones de cuatro medidas de adiposidad como la circunferencia de cintura (CC), el índice de masa corporal (IMC), y los pliegues cutáneos subescapular y abdominal con diferentes factores de riesgo cardiovascular (FRCV) en infantes pre-púberes.
MétodosCuatrocientos noventa y cuatro pre-púberes, de 6-10 años, participaron en este estudio transversal. Se midió la adiposidad con los pliegues cutáneos subescapular y abdominal, CC e IMC y los FRCV como presión arterial sistólica (PAS) y diastólica (PAD), glucosa, triglicéridos (TG), y el colesterol de las lipoproteínas de alta (cHDL) y baja densidad (cLDL). Se crearon variables dicotómicas respecto a estar y no estar en el cuartil superior (Q4) con las variables CC, IMC, y los pliegues en todos los sujetos.
ResultadosEl 52,8% de los infantes no presentó ningún FRCV, el 33,4% presentó un factor, y el 10,9 y 2,8% tenían 2 y 3 factores, respectivamente. El análisis de regresión logística ajustada mostró que ubicarse en el Q4 de las variables antropométricas y los FRCV, se asociaba con TG ≥100mg/dL. Niveles de glucosa ≥96mg/dL mostraron una asociación con el Q4 y con el pliegue abdominal. Presentar 2 o más FRCV se asoció significantemente con el Q4 en todas las variables antropométricas a pesar del ajuste por edad, género e ingesta calórica. El pliegue subescapular fue el indicador de adiposidad con mayor índice de riesgo.
ConclusionesLos infantes con una adiposidad más desfavorable tienden a presentar mayor riesgo cardiovascular en la etapa pre-púber.
Cardiovascular risk has increased in recent years in children and adolescents, and most studies associate such risk with the prevalence of obesity, which is reaching pandemic levels.1,2 In addition, different longitudinal3,4 and cross-sectional5 studies have shown that cardiovascular risk factors (CVRFs) associated with these diseases (central obesity, high blood pressure, dyslipidemia) persist from childhood into adulthood.6,7
Other observations have clearly shown a relationship between overweight/obesity and early lipid and carbohydrate changes.8,9 In children and adolescents, obesity is a significant predictor of high blood pressure and dyslipidemia. In US schoolchildren, increased obesity and central adiposity have resulted in an increased occurrence of hypercholesterolemia and high blood pressure.10,11 The use of early indicators for preventing obesity in children has therefore been considered a public health priority in many countries.12
The primary objective of this study was to examine the association of four adiposity measures (waist circumference, body mass index, and subscapular and abdominal skinfolds) with different CVRFs in prepubertal children. The potential influence of confounding variables such as age, gender, and total calorie intake was also assessed as a secondary objective.
MethodsParticipantsChildren selected for this study participated in the IFRECNTEC study (Identification of risk factors for non-transmissible chronic diseases of adults in schoolchildren aged 10–16 years in Cali, Colombia).13 This study assessed early signs of non-transmissible chronic diseases (NTCDs) in a representative sample of community schoolchildren aged 6–17 years living in Cali, Colombia (approximately 2800).14 Blood parameters were tested in a subsample of 494 prepubertal children, along with comprehensive anthropometric, nutritional, stomatological, and physical activity assessment. Anthropometric and blood data were collected for this study from the 256 boys and 238 girls forming this subsample. The data were collected from 2002 to 2006.
The study was conducted in accordance with the ethical rules as set down in the Declaration of Helsinki and the applicable Colombian legal regulations governing clinical research in humans (Decision 008430 of the Colombian Ministry of Health). The study was approved by the ethics committee of Universidad del Valle. At each of the institutions selected, managers and parents were requested to participate. Before the start of the study, children and their parents/guardians were informed about the nature of their participation and signed a consent form.
AdiposityThe Lopez et al.15 anthropometric protocol standardized for the Colombian population was used for this study. Skinfolds were measured on the left side of children using calipers (Slim Guide®, USA) in the following six areas: triceps, biceps, subscapular, abdominal, thigh, and gastrocnemius. Weight and height were measured using standard procedures.14 BMI was calculated as weight in kilograms/squared height in meters. In this study, two skinfolds (subscapular and abdominal) were used as adiposity markers, and waist circumference was used as a marker of central obesity.
Cardiovascular risk factorsSystolic (SBP) and diastolic (DBP) blood pressures were measured in mmHg using an Omrom® (M6, USA) (mmHg) automated digital pressure meter validated by the European Society of Hypertension.16 After fasting for at least 10h, children had blood drawn by puncture into the cubital vein, and the sample was placed in a dry tube for serum. Triglyceride (TG), high density lipoprotein cholesterol (HDL-C), and glucose levels were measured by colorimetric enzymatic methods using an A-15 analyzer (Biosystems, Spain). Low density lipoprotein cholesterol (LDL-C) fraction was calculated using the Friedewald formula.17
Association of cardiovascular riskSystolic and diastolic blood pressure values and LDL-C, TG, glucose, and HDL-C levels were part of the CVRF cluster because they are included in the definition of metabolic syndrome and cardiovascular disease (CVD) for adults18 and young subjects.19 Cut-off points used for the lipid profile were <35mg/dL for HDL-C and ≥130mg/dL for LDL-C according to the definition by Freedman et al.20 and ≥80th percentile for TG, taken from the study population (≥100mg/dL), according to the definition of Garnett et al.21 As there are no cut-off points for high glucose levels in children under 10 years of age, values equal to or less than the 90th percentile of the actual study population (≥96mg/dL) were taken as reference. High systolic or diastolic blood pressure was defined according to the criteria of the National Heart Lung and Blood Institute (NHLBI, USA) as a value equal to or higher than the 90th percentile for age, sex, and height reported in the population data table of the NHLBI.22
Data analysisResults are given as median and range because of data distribution (after a normality analysis). The prevalence of each CVRF by gender was calculated, and gender differences were estimated using a Chi-square test. Dichotomous variables were created based on whether or not the subjects were in the upper quartile (Q4) for waist circumference, BMI, and subscapular and abdominal skinfold variables. Adjusted logistic regressions were performed to assess the association of these variables with the presence of CVRFs. Adjustment models for evaluation always included age, gender, and total calorie intake (kilocalories/day). All analyses were performed using STATA v.11 for Windows software. A value of p<0.05 was considered statistically significant.
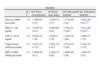
ResultsTable 1 shows the descriptive characteristics of children. A higher proportion of boys with glucose levels ≥96mg/dL (90th percentile of the total group) and of girls with low HDL-C levels can be seen. Adjusted logistic regression analysis showed that being in the upper quartile (Q4) of anthropometric variables and of CVRFs adjusted for age, gender, and calorie intake was associated with an increased number of TG levels ≥100mg/dL (80th percentile of the total group) (Table 2). This same analysis showed no association with waist circumference and BMI variables, but did show an association with subscapular and abdominal skinfolds and low HDL-C levels. Glucose levels higher than the 90th percentile showed an association with the upper quartile (Q4) of abdominal skinfold (Table 2).
Biochemical, anthropometric, and blood pressure values in prepubertal children.
| Boys (n=256)Median (range) | Girls (n=238)Median (range) | |
| Glucose (mg/dL) | 85(80–91) | 82(78–89) |
| HDL-C (mg/dL) | 50(43–58) | 50(42–58) |
| LDL-C (mg/dL) | 109.5(92–130) | 111(93–130) |
| Triglycerides (mg/dL) | 69(51–94) | 72.5(52–95) |
| SBP (mmHg) | 100(90–100) | 90(85–100) |
| SBP (mmHg) | 60(50–60) | 60(50–60) |
| Waist circumference (cm) | 56(53–59.8) | 54.5(51.5–58) |
| BMI (kg/m2) | 15.6(14.6–17.5) | 15.7(14.6–17.5) |
| Skinfolds | ||
| Subscapular (cm) | 6.0(5.0–8.8) | 7.5(6.0–10) |
| Abdominal (cm) | 8(5.6–13) | 11(7.0–16) |
| Cardiovascular risk factors | n (%) | n (%) |
| Glucose ≥90th percentile | 35(13.7)a | 18(7.6)a |
| HDL-C <40 mg/dL | 9(3.5)b | 18(7.6)b |
| LDL-C ≥130 mg/dL | 62(24.6) | 59(24.8) |
| Triglycerides ≥90th percentile | 47(18.4) | 54(22.7) |
| SBP or DBP ≥90th percentile | 7(2.7) | 6(2.5) |
HDL-C: HDL cholesterol; LDL-C: LDL cholesterol; BMI: body mass index; DBP: diastolic blood pressure; SBP: systolic blood pressure.
a,bDifference between the groups that share this letter, p<0.05. cCut-off points were estimated based on the actual study population.
Odds ratios (95% CI) adjusted by age, gender, and calorie intake for cardiovascular risk factors in the upper quartile of anthropometric variables.
| Quartiles | |||||
| Q 1–3 | Q4 Waist circumference | Q4 Body mass index | Q4 Subscapular skinfold | Q4 Abdominal skinfold | |
| Glucose ≥90th percentile | 1.0 | 1.20(0.63–2.27) | 1.35(0.71–2.57) | 1.71(0.90–3.24) | 1.94(1.04–3.61)*** |
| HDL-C <40 mg/dL | 1.0 | 1.67(0.72–3.87) | 2.04(0.89–2.07) | 3.16(1.41–7.10)** | 2.41(1.08–5.39)*** |
| LDL-C ≥130 mg/dL | 1.0 | 0.84(0.51–1.58) | 1.04(6.3–1.70) | 1.24(0.76–2.00) | 1.08(0.77–1.75) |
| Triglycerides ≥90th percentile | 1.0 | 2.93(1.81–4.73)* | 2.76(1.70–4.47)* | 3.27(2.02–5.29)* | 2.34(1.45–3.75)* |
| SBP or DBP ≥90th percentile | 1.0 | 3.09(0.94–10.1) | 2.42(0.73–8.00) | 1.60(0.46–5.58) | 1.46(0.42–5.07) |
HDL-C: HDL cholesterol; LDL-C: LDL cholesterol; DBP: diastolic blood pressure; SBP: systolic blood pressure: Q: quartile.
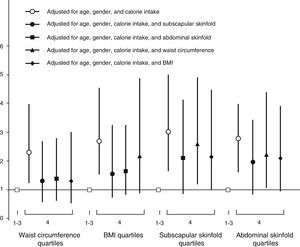
The presence of two or more CVRFs was significantly associated with classification in the upper quartile (Q4) in all anthropometric variables despite adjustments for age, gender, and calorie intake, with subscapular skinfold being the adiposity marker associated with the highest risk index. When all the other anthropometric variables were added to the adjustment model, the association of waist circumference and BMI continued to be without significance, while association persisted for both skinfolds (subscapular and abdominal) (Fig. 1). No cardiovascular risk factor was found in 52.8% of children, while one, two, and three factors were found in 33.4%, 10.9%, and 2.8% respectively. No gender differences were seen in the prevalence of number of factors.
DiscussionOverweight and obesity prevalence have dramatically increased in children and adolescents in recent decades, particularly in countries with mainly middle and low average incomes.23 Different studies have confirmed that increased body composition values predict for the occurrence of conditions that may affect cardiometabolic health in adult life.24,25 Some of the studies exploring this issue23–26 used BMI as the only or main measure of body composition, following recommendations by the International Obesity Task Force (IOTF).27 However, other authors28,29 agree that BMI or age-adjusted BMI do not take into account body fat distribution, which has been shown to be a predictor for the occurrence of CVD in adults.21–24 Anthropometric measures such as waist circumference or skinfolds,30 in addition to weighing weight composition and predicting a future cardiometabolic risk, may practically eliminate the bias resulting from child adiposity, described by Tu et al. as the “reversal paradox”.31 There is adequate evidence in adults to show that fat accumulation around the waist is the main risk factor for developing high blood pressure, diabetes mellitus, and metabolic syndrome.32 Two large international epidemiological studies in middle and low income countries, the INTERHEART33 and INTERSTROKE34 studies, showed that an increased waist circumference involves a population attributable risk (PAR) ≈60%, which is the same as saying that in almost two out of every three subjects who experience an acute myocardial infarction the main reason is the presence of abdominal obesity. However, our study showed that skinfolds (particularly the subscapular fold) are associated with a greater cardiovascular risk as compared to waist circumference. This finding agrees with the results of a 20-year follow-up of 2188 adults recently reported by Schmidt et al.35 showing that skinfolds, used as measures of adiposity, were the most significant predictors for the occurrence of metabolic syndrome in early adulthood. The RR of skinfolds for children in the upper quartile (as compared to the lower quartile) was 4.8 in males and 5.8 in females. For instance, Baker et al.36 noted that an increased adiposity “based on skinfolds and BMI z-score” in a cohort of Danish children aged 7–13 years was associated with an ≈22% greater risk of having a CVD event in early adulthood. By contrast, an analysis of a cohort of 11,000 Scottish children showed no association of adiposity measures at school entry with NTCDs in adulthood.37
The secondary objective of our study was to assess the degree of association between several adiposity markers and CVRFs. For this, differences in adiposity levels between the groups were assessed using four markers. Results showed that adiposity measured by skinfolds showed a closer association to CVRFs as compared to BMI and waist circumference. However, when two or more CVRFs were assessed, most adiposity markers were shown to be related to their presence. Moreover, regression analyses showed that skinfolds are not the only variables to reach a significant association after adjustment for a strong adiposity marker related to disease in adulthood, such as waist circumference. These results suggest that the group with greater adiposity (particularly as measured by skinfolds) had more unfavorable values in all four CVRFs assessed in prepubertal children.
A study such as this has limitations inherent to its design. If the purpose of such an analysis is to examine only the association between body composition of children and some CVRFs, such limitations are of minor significance. However, if the purpose is to separate the effects of high adiposity in childhood from the effects of adiposity in adults, changes in adiposity over time must be recorded. Thus, the measurement at an early age of anthropometric markers including not only BMI (for which centile curves from the age of 2 years are already available, CDC),38 weight for height, and weight for age, but also subcutaneous fat through skinfold thickness may provide additional data on the causal relationship with some diseases such as metabolic syndrome and CVD.39 Such anthropometric assessments and their relationship to cardiovascular risk in prepubertal children are extremely important considering the high prevalence of prediabetes in adolescents with severe obesity.40 In conclusion, children with a more unfavorable adiposity profile tend to be at greater cardiovascular risk, and in the prepubertal stage, subscapular and abdominal skinfolds may be more related to CVD than BMI and waist circumference. Additional studies are needed to confirm and extend the findings of this research.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Ramírez-Vélez R, et al. Asociación entre adiposidad y factores de riesgo cardiovascular en infantes pre-púberes. Endocrinol Nutr. 2011;58:457–63.