Preeclampsia is a multifactorial disease. Among these factors, untreated hypertension during pregnancy can result in high morbidity and mortality rates and may also be related to the future development of cardiovascular diseases.Therefore, this systematic review aimed to determine the association of previous preeclampsia with the future development of cardiovascular diseases.
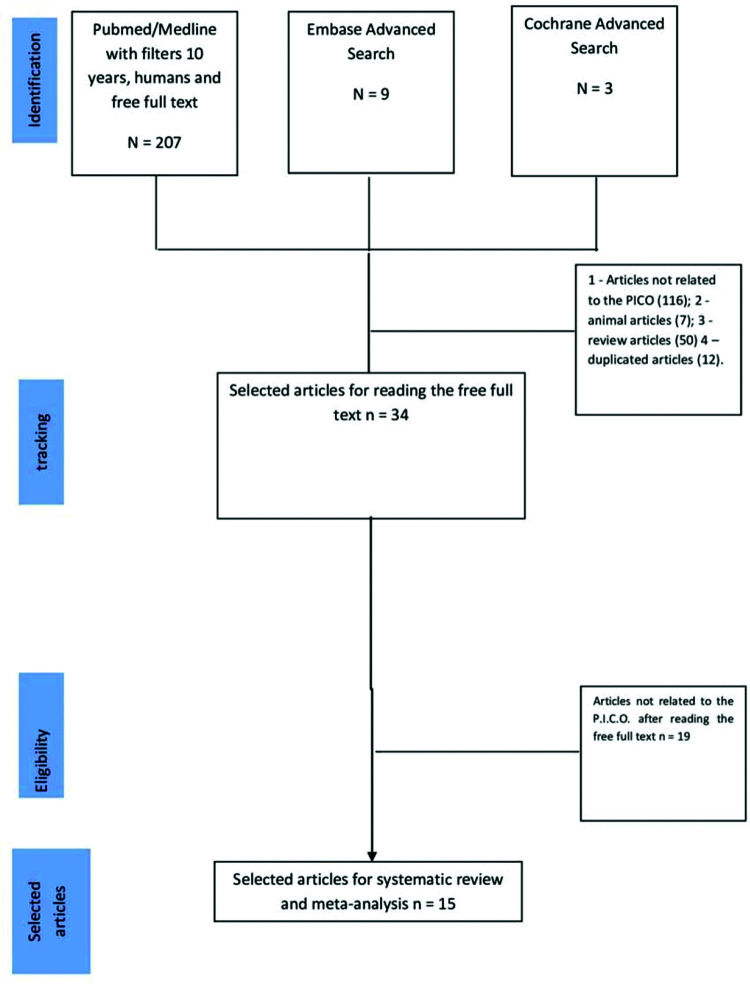
Studies on the association between preeclampsia and future cardiovascular diseases published in the last 10 years (2009-2019) were identified from the PubMed/Medline (207 articles), Embase (nine articles), and Cochrane (three articles) databases using the keywords “preeclampsia” and “future cardiovascular diseases”, “preeclampsia” and “future heart attack”, and “preeclampsia” and “future cardiac disease”. After applying the inclusion and exclusion criteria, 15 articles were analyzed by systematic review and meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The meta-analysis and the determination of the quality of the articles were conducted using RevMan software, version 5.3.
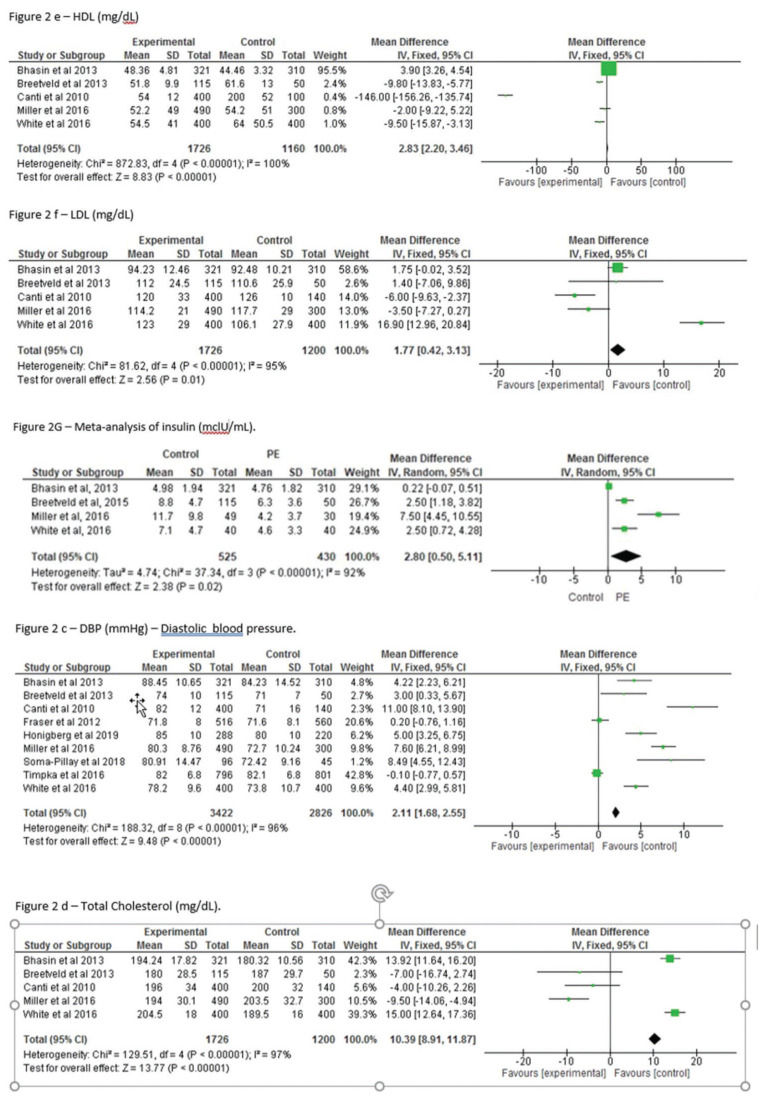
Statistically significant differences were observed between the control and previous preeclampsia groups with respect to systolic blood pressure (mean difference [MD] 4.32; 95% confidence interval [95%CI] 3.65, 4.99; p<0.001), diastolic blood pressure (MD): 2.11; 95%CI: 1.68, 2.55; p<0.0001), and insulin level (MD: 2.80; 95% CI: 0.50, 5.11; p<0.001). Body mass index (MD: 2.57, 95%CI: 2.06, 3.07; p=0.0001), total cholesterol (MD: 10.39; 95%CI: 8.91, 11.87; p=0.0001), HDL (MD: 2.83; 95%CI: 2.20, 3.46; p=0.0001), and LDL (MD: 1.77; 95%CI: 0.42, 3.13; p=0.0001) also differed significantly between groups.
Thus, the results of the present study showed that women with a history of preeclampsia were more likely to develop cardiovascular disease.
Preeclampsia (PE) is defined as a pregnancy complication characterized by high blood pressure and signs of damage to other organs, with dysfunctions in the circulatory, renal, hematological, hepatic, and neurological systems. PE usually begins after 20 weeks of pregnancy in women with previously normal blood pressure levels (1,2). This condition has high morbidity and mortality, affects 2-5% of pregnant women and is responsible for thousands of deaths of mothers and fetuses worldwide (3).
The risk factors for the development of PE include preexisting diabetes, pre-pregnancy body mass index ≥35 kg/m2, nulliparity, family history of PE, twin pregnancy, maternal age ≥40 years, systolic blood pressure ≥130 mmHg, chronic hypertension, history of chronic kidney disease, and assisted reproductive technologies (4,5). Among the pathophysiological mechanisms of PE development is vascular dysfunction, defined as an imbalance between pro-angiogenic and anti-angiogenic factors. The levels of markers such as vascular endothelial growth factor and placental growth factor (PIGF) are increased in endothelial vascular dysfunction, with a consequent increase in systolic and diastolic pressures and proteinuria in pregnant women (3,6).
While previous studies have demonstrated the association of PE development in pregnant women and future cardiovascular complications such as the development of hypertension, diabetes, ischemic disease, and other cardiovascular diseases, recent literature has suggested the need for additional studies for a more complete understanding of how this relationship is established (7–11).
Therefore, the objective of the present systematic review and meta-analysis was to evaluate the association between previous PE and future cardiovascular diseases.
MATERIAL AND METHODSThe literature search strategy was applied as recommended by Berstock et al. (2019) (12). We searched for articles published from January 2009 to July 2020. This time interval was chosen because the diagnosis of PE has improved and changed in the last decade. We first selected keywords from related articles and used Medicals Subject Headings (MeSH) to identify more related keywords with close meaning, such as: (“preeclampsia” [MeSH Terms] OR (“future cardiovascular diseases” [All Fields], as well as the MeSH terms “preeclampsia and future heart attack” and “preeclampsia and future cardiac disease” The search strategy was applied to the PubMed/Medline, Embase, and Cochrane databases.
This review was conducted according to the recommendations established by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) (13,14).
Two researchers with the ability to compile systematic reviews (E.C.V. and P.R.H.R.) independently and blindly retrieved the papers and evaluated the titles and abstracts with reference to the inclusion and exclusion criteria according to the PICO components (14). The selected articles were then critically evaluated for inclusion or exclusion in the review. Disagreements between the investigators regarding the inclusions of studies were resolved following consultation with a third reviewer (L.L.C.).
The main outcomes were increased risks of diabetes mellitus, dyslipidemia, hypertension, cardiovascular heart failure, and brain disease, as well as an increased risk of cardiac diastolic dysfunction. The other outcomes were increased risks of mother and child mortality, stroke, ischemic heart disease, increased risk of coronary artery calcification, greater relative wall thickness, and reduced left ventricular end-diastolic volume (Table 1). These qualitative results are the descriptors of various types of cardiovascular diseases that women with a history of PE eventually develop. Among several cardiovascular diseases that can be assessed, the most common are described here.
Characteristics of studies about women with preeclampsia.
| Author and year of publication | Country, baseline years of study | Study design | Definition of preeclampsia (SBP, DBP) | No. of participants | Follow-up time (median, range, years) | Age at follow-up (median, range, years) | Outcome |
|---|---|---|---|---|---|---|---|
| Gastrich et al. 2020 | USA | Case-control study | NS | 6,360 | 15 | 26.78 | Cardiac diseases, diabetes, stroke, myocardial infarction. |
| Honigberg et al. 2019 | USA | Observational study | SBP≥140 and/or DBP≤90 mmHg | 2,808 | 7 | 57.4 | Hypertension, hyperlipidemia, diabetes mellitus. |
| Kuo et al. 2018 | Taiwan 1996-2010 | Retrospective longitudinal study | NS | 6,475 | 9.8 | 30.5 | Increased risks of DM, dyslipidemia, hypertension, CHF, and cerebrovascular diseases. |
| Soma-Pillay et al. 2018 | South Africa 2013-2016 | Descriptive study | Mean (SD) 128 (14.17) −115 (9.89) | 141 | 1 | 28.9 | Increased risk of cardiac diastolic dysfunction one year after delivery. |
| Theilen et al. 2018 | USA 1939-2012 | Retrospective cohort study | NS | 172,152 | 18 | − | Increased risks of mortality from DM, ischemic heart disease, and stroke. |
| Parikh et al. 2017 | Sweden 1973-2011 | Prospective cohort study | SBP≥140 and/or DBP≤90 mmHg | 16,009 | 37 | 40 | Women presenting with preeclampsia, gestational diabetes, or placental abruption. |
| Miller et al. 2016 | USA | Case-control study | NS | 79 | 1 | 60 | Women with histories of preeclampsia, both waist circumference and measures of insulin resistance were greater in women with coronary artery calcification. |
| Timpka et al. 2016 | Sweden, USA, UK 1991-1992 | Prospective birth cohort study | ≥140, ≤90 | 1,511 | 1 | 17 | Greater relative wall thickness and reduced left ventricular end-diastolic volume. |
| White et al. 2016 | USA 1976-1982 | Cohort | ≥140, ≤90 | 80 | 6 | 59 | Among women with histories of preeclampsia, the presence of coronary artery calcifications. |
| Breetveld et al. 2015 | Netherlands 2010-2012 | Observational study | ≥140, ≤90 | 115 | 3 | 25-45 | A two-fold risk of developing cardiovascular disease. |
| Savitz et al. 2014 | USA 1995-2004 | Observational study | NS | 849,639 births | 1 | 1 | Hypertensive disorders of pregnancy strongly predicted short-term risk of hospitalization for chronic disease within 1 year of delivery, |
| Bhasin et al. 2013 | India | Observational study | NS | 631 | 10 | 33 | Hypertension pregnancy, DM, and pregnancy outcomes were all associated with an increased risk of CVD 10 years later |
| Feig et al. 2013 | Canada 1994-2008 | Retrospective cohort study | NS | 1,010,068 | 16 | 15-50 | Preeclampsia was associated with a two-fold increased incidence of diabetes. |
| Frasier et al. 2012 | United Kingdom | Prospective cohort study | ≥140, ≤90 | 3,416 | 18 | Mean 48 | Both gestational hypertension and preeclampsia were associated with a greater number of cardiovascular risk factors. |
| Canti et al. 2010 | BR | Cross-sectional study | NS | 40 | 10 | NS | Blood pressure measurements. |
Legends: DM - diabetes mellitus; CVD - cardiovascular disease; CHF - congestive heart failures.
RevMan 5.3 (Cochrane Collaboration, Oxford, UK) was used to perform the meta-analysis. A random-effects model was used for the assessment of heterogeneity.
Statistical analysisThe mean values and standard deviation of the studies are presented as mean difference (MD) of the post-intervention values after calculating the inverse of the variance to determine the magnitude of the effect of PE and future cardiovascular diseases (15). Heterogeneity was assessed using the Cochran and I2 Q tests, followed by visual inspection of the graph.
Heterogeneity between studies was defined as an I2 value above 50% (16,17). The analyses were performed using RevMan 5.3.
RESULTSThe search process, identification, and selection of the articles are shown in Fig. 1. The inclusion criteria were articles published in English related to the keywords preeclampsia and future cardiovascular disease appearing in the titles and abstracts of the selected articles. Articles without these keywords were excluded because they were not related to the Patient/Problem/Population, Intervention, Comparison, and Outcome(s) (PICO) design for the study, as follows. Patients: women with PE, Intervention: classic definitions by the articles of women with PE and optimal medical treatment during pregnancy, Comparator: women without PE and with pregnancy without hypertension, and Outcomes: future cardiovascular diseases in by the target audience (13). The exclusion criteria in the PubMed database were the filters “last 10 years”, “humans”, and “free full text”. This search identified 207 articles. We also searched for the keywords with an advanced search of the titles, which identified nine and three articles in the Embase and Cochrane databases, respectively. The next step was to apply the following exclusion criteria: we excluded 116 articles not related to the PICO, seven articles on animals, 50 review articles, and 12 duplicate articles. Of 34 articles selected for complete text review, 19 were excluded for not being related to the PICO. Thus, a total of 15 articles were finally selected for inclusion in the systematic review and meta-analysis (Fig. 1).
The information obtained from the studies selected for the systematic review is presented in Table 1, which lists the following characteristics of the articles: authors, year of publication, country, baseline, study years, study design, definition of PE according to systolic and diastolic blood pressures (SBP and DBP, respectively), number of participants in the study, follow-up time (mean and range in years), age at follow-up (mean and range in years), and outcomes.
Among the cardiovascular diseases that developed after PE that were reported in our selected articles, the most prevalent was hypertension (18–26,30–32), followed by diabetes (18,20,21,24–28,30,31), and heart failure (18,19,22,23,26,27,30,31). Stroke and brain diseases also occurred in some patients a few years after the incidence of PE (18,23,24,27,31), as well as coronary artery calcification in some women (21,29) (Table 2). It is important to emphasize that the moment of the evaluations of the variables of the meta-analysis in the selected articles were made after the follow-up, either one year or ten years or more after the diagnosis of PE, so that we can have as an outcome and as a result, the appearance of cardiovascular diseases.
Studies including women with PE and increased risks of the development of several cardiovascular diseases in general or specifically.
| Authors | Cardiovascular disease in general | Diabetes mellitus | Heart failure | Stroke and cerebral diseases | Coronary artery calcification | Hypertension |
|---|---|---|---|---|---|---|
| Gastrich et al. 2020 | X | X | X | X | X | |
| Honigbert et al. 2019 | X | X | X | X | ||
| Kuo et al. 2018 | X | X | X | X | − | X |
| Som sa-Pillay et al. 2018 | X | − | X | − | − | X |
| Theilen et al. 2018 | X | X | X | X | − | − |
| Parikh et al. 2017 | X | X | − | − | − | X |
| Miller et al. 2016 | X | X | − | − | X | X |
| Timpka et al. 2016 | X | − | X | − | − | X |
| White et al. 2016 | X | − | − | − | X | − |
| Breetveld et al. 2015 | X | − | X | X | − | X |
| Savitz et al. 2014 | X | X | − | X | − | X |
| Bhasin et al. 2013 | X | X | − | − | − | X |
| Feig et al. 2013 | − | X | − | − | − | − |
| Frasier et al. 2012 | X | X | X | − | − | X |
| Canti et al. 2010 | X | X |
X: relationship between women with preeclampsia and the future development of various types of cardiovascular disease.
-: no specific mention of this cardiovascular disease.
The results of the meta-analysis are described below. Comparison of body mass index (BMI) between the PE and control groups showed a significantly higher value in the PE group, indicating that women with previous PE were heavier than the control women (MD: 2.57, 95% confidence interval [95%CI]: 2.06, 3.07; p≤0.0001) (Fig. 2A). As expected, SBP was significantly higher among women in the previous PE group than that in the control group (MD: 4.32; 95%CI: 3.65, 4.99; p<0.00001) (Fig. 2B). Moreover, as expected, DBP was also significantly higher among women with previous PE (MD: 2.11; 95%CI: 1.68, 2.55, p<0.00001) compared to that in the control groups. In addition, the CI between groups was low (Fig. 2C). Blood insulin also differed significantly between women with PE and the controls (MD: 2.80; 95%CI: 0.50, 5.11; p<0.00001) (Fig. 2G).
A-G, Meta-analysis of the relationships between body mass index, systolic blood pressure, diastolic blood pressure, total cholesterol, high-density lipoprotein, low-density lipoprotein, and insulin levels and the later development of cardiovascular diseases according to the history of preeclampsia.
We also observed statistically significant differences in total cholesterol level (MD: 10.39; 95%CI: 8.91, 11.87; p<0.0001) (Fig. 2D), high-density lipoprotein (HDL) level (with a broad confidence interval) (MD: 2.83; 95%CI: 2.20, 3.46; p≤0.0001) (Fig. 2E), and low-density lipoprotein level (LDL) (MD: 1.77; 95%CI: 0.42, 3.13; p=0.09) (Fig. 2F).
DISCUSSIONThe major limitation of this study was that most of the studies included in the systematic review followed the mothers for less than 10 years, a fact that only allowed the analysis of blood markers and not the development of cardiovascular disease in women with a history of PE. Another limitation of this study was that, in bias risk analysis, the variables related to the blinding of the participants and personnel, blinding of the outcome assessment, and other biases showed unclear risks of bias. However, the strength of this study was that it demonstrated increased levels of cardiovascular disease variables in women with PE, indicating the probable future development of cardiovascular diseases.
The main findings of the present meta-analysis were increased BMI, SBP, DBP, HDL, LDL, total cholesterol, and insulin concentration in the previous PE group compared to those in the control group.
Among the articles included in the systematic review (18–32), we identified several outcomes leading to the increased incidence of future cardiovascular disease among women with PE, including increased mortality and two-fold increases in diabetes, hypertension, myocardial infarction, and other cardiovascular diseases. The results of these studies were concordant with those of four recent meta-analyses (33–35) showing that women with PE have higher chances of developing future cardiovascular diseases as well as a higher risk of mortality. One meta-analysis reported higher chances of developing coronary heart disease, stroke, and death due to cardiovascular disease (33); another reported higher chances of developing hypertension, ischemic heart disease, heart failure, and cerebrovascular accidents (34). Alma et al. (2017) (33) analyzed the role of biomarkers such as C-reactive protein, HDL, and insulin as markers of future cardiovascular diseases and observed increased levels in women with PE compared to those in pregnant women without increased blood pressure. In a study of women with hypertensive diseases in pregnancy, Ukah et al. (2018) (35) used multivariate models to demonstrate that these women are at higher risk of developing cardiovascular disease in the future. Irgens et al. (2001) (38) assessed whether mothers and fathers were at higher risk of death and cardiovascular disease after the mother was diagnosed with PE and concluded that genetic factors increased the chance of developing cardiovascular risks. Sattar et al. (2002) (39) discussed the pre-gestational metabolic status of women, suggesting that an adverse pregnancy increases the risk of future vascular and metabolic diseases.
Our meta-analysis identified the following six significant and consistent factors among PE patients: higher SBP (19,21–23,25,26,29), higher DBP (19,21–23,25,26,29), higher blood insulin value, which is indicative of future diabetes development (21,23,25,29); and higher HDL, LDL, and insulin levels. These results agree in part with those in recent literature, including the meta-analyses by de Groot et al. (2017) (33) and Brouwers et al. (2018) (34). However, most systematic meta-analyses have investigated other parameters in women with PE or with hypertensive disease in pregnancy; that is, the development of various cardiovascular diseases such as the risks of heart failure, coronary heart disease, and death from cardiovascular disease, focusing on different variables from those analyzed in the present study (32). Other studies performed different analyses; for example, Alma et al. (2017) (33) reported higher C-reactive protein and HDL levels in women with PE compared to those in controls. Ukah et al. (2018) (35) used another approach comparing the quality of assessment and accuracy and specificity in women with PE and other hypertensive diseases in pregnancy.
In our meta-analysis, BMI (19,21–23,25,26,29,31,32) showed statistical significance (p≤0.0001), consistent with recent findings (3,32) reporting a two-fold increase in the risk of diabetes in women with PE, as well as increased hypertension and serum glucose and lipid levels. Total cholesterol (21,23,25,29,31,32) and LDL (21,23,25,29,31,32) concentrations were higher in the control group, although the differences were not statistically significant. Women with a history of PE had significantly higher HDL levels (21,23,25,29,31,32). However, these relationships varied in the literature depending on socioeconomic and quality of life factors such as age, smoking, alcohol consumption, and physical activity (36,37).
CONCLUSIONIn conclusion, the results of this study showed that women with previous PE were more likely to develop cardiovascular disease in the future.
AUTHOR CONTRIBUTIONSde Arruda Veiga EC participated with substantial contributions to study concept and design, intellectual content, literature search, data and statistical analysis, manuscript preparation, article drafting, critical revision for important intellectual content and final approval of the manuscript. Rocha PR participated with literature search, data and statistical analysis, manuscript preparation, article drafting or critical revision for important intellectual content and final approval of the version to be published. Bettiol H, Barbieri MA, Caviola LL and da Conceição Pereira Saraiva M participated with data and statistical analysis, article drafting or critical revision for important intellectual content and final approval of the version to be published. Cardoso VC participated with data and statistical analysis, article drafting or critical revision for important intellectual content final approval of the version to be published.FSC-Data and statistical analysis, article drafting or critical revision for important intellectual content and final approval of the version to be published. Cavalli RC participated with substantial contributions to study concept, design and definition of intellectual content, article drafting and critical revision for intellectual content and final approval of the version to be published.
This study was supported by CNPq and CAPES (Brasília-Br) (protocol number Cnpq 301293/2018-0).
No potential conflict of interest was reported.