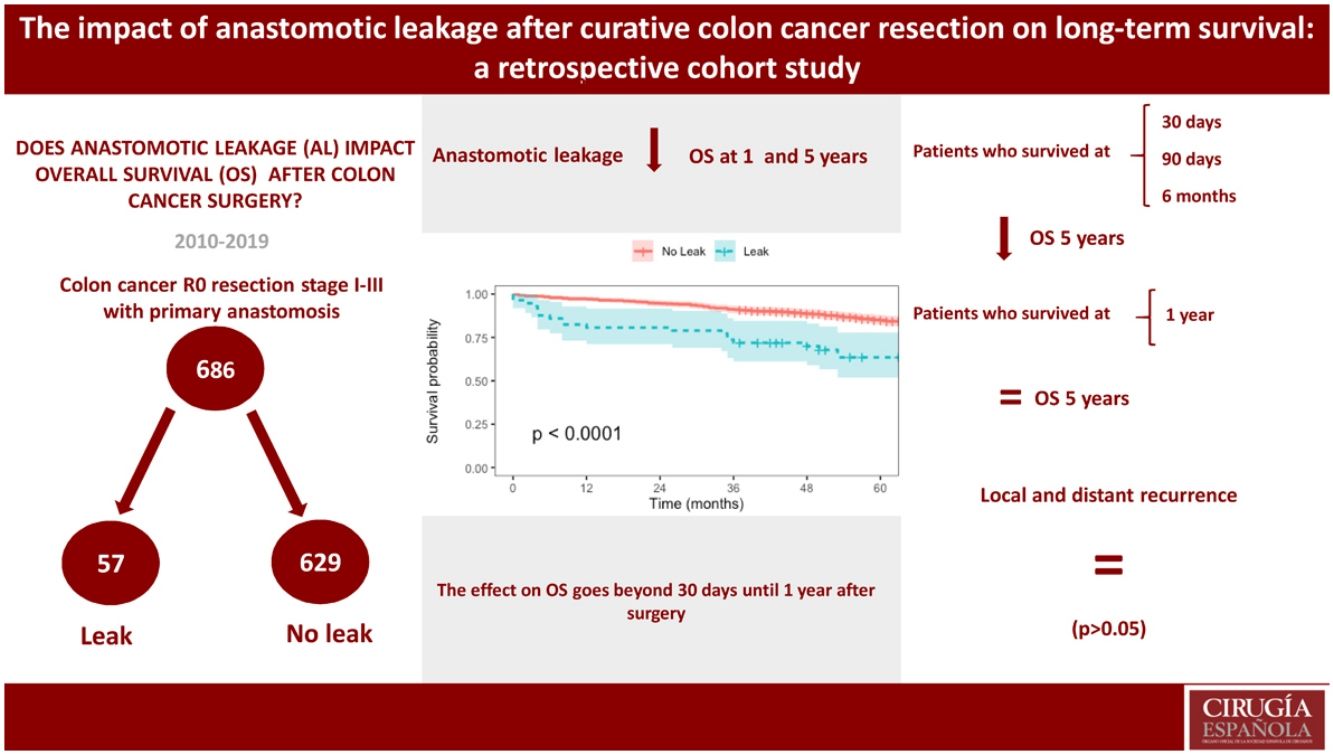
Anastomotic leakage (AL) is one of the most feared postoperative complications in colon cancer surgery due to an association with increased morbidity and mortality, although its impact on long-term survival is not consensual. The aim of this study was to investigate the influence of AL on long-term survival of patients undergoing curative colon cancer resection.
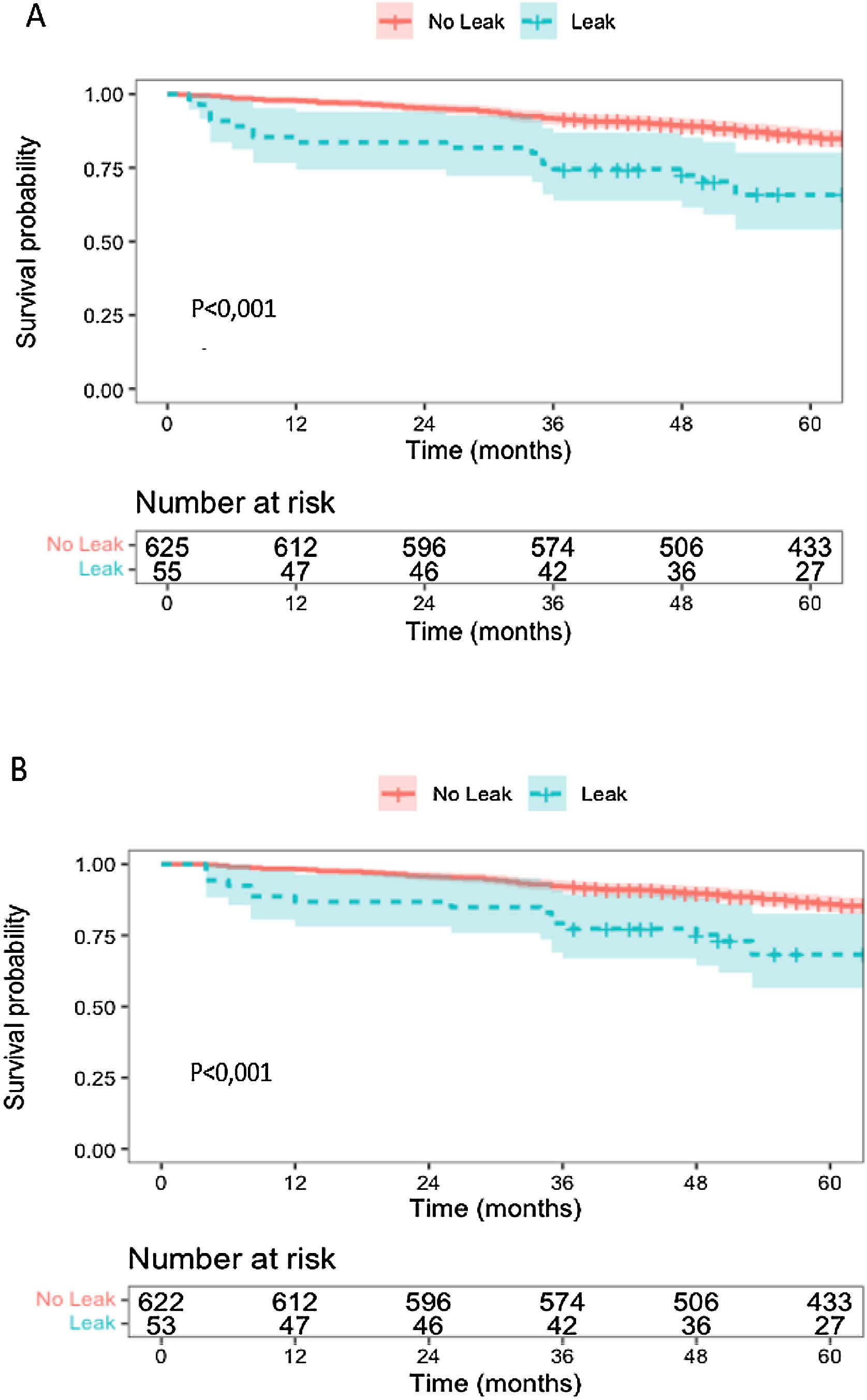
MethodsA single-centre retrospective cohort study was designed. Clinical records of all consecutive patients undergoing surgery at our institution between 01/01/2010 and 12/31/2019 were reviewed. Survival analysis was performed by Kaplan–Meier method to estimate overall and conditional survival and Cox regression to search for risk factors impacting survival.
ResultsA total of 2351 patients submitted to colorectal surgery were screened for eligibility, of which 686 with colon cancer were included. AL occurred in 57 patients (8,3%) and was associated with higher postoperative morbidity and mortality, length of stay and early readmissions (P < 0,05). Overall survival was inferior in the leakage group (Hazard Ratio 2,08 [1,02–4,24]). Conditional overall survival at 30, 90 days and 6 months was also inferior in the leakage group (P < 0,05), but not at 1 year. Risk factors independently associated with reduced overall survival included AL occurrence, higher ASA classification and delayed/missed adjuvant chemotherapy. AL did not impact local and distant recurrence (P > 0,05).
ConclusionAL has a negative impact on survival. Its effect is more pronounced on short-term mortality. AL does not appear to be associated with disease progression.
La fuga anastomótica (FA) es una complicación postoperatoria temida en la cirugía del cáncer de colon por asociación con mayor morbimortalidad, aunque su impacto en la supervivencia a largo plazo no es consensuado. Nuestro objetivo fue investigar el efecto de la FA en la supervivencia a largo plazo de pacientes sometidos a resección curativa del cáncer de colon.
MétodosSe realizó un estudio de cohorte retrospectivo unicéntrico de pacientes consecutivos intervenidos quirúrgicamente entre 01/01/2010 y el 31/12/2019. El análisis de supervivencia se realizó por el método de Kaplan-Meier para evaluar la supervivencia global (SG) y condicional y una regresión de Cox para evaluar los factores de riesgo con efecto en la supervivencia.
ResultadosDe 2351 pacientes sometidos a cirugía colorrectal, se incluyeron 686 con cáncer de colon. FA afectó 57 pacientes (8,3%) y se asoció con mayor morbimortalidad postoperatoria, duración de estancia hospitalaria y reingresos (P < 0,05). La SG fue inferior en el grupo de fuga (Hazard Ratio 2,08 [1,02–4,24]). La SG condicional a los 30, 90 días y 6 meses fue inferior en el grupo de fugas (P < 0,05), pero no a 1 año. Los factores de riesgo que se asociaron con SG reducida incluyeron la FA, clasificación ASA más alta y quimioterapia adyuvante retrasada/perdida. FA no afectó la recurrencia local y distante (P > 0.05).
ConclusionesFA tiene un impacto negativo en la supervivencia, con efecto más pronunciado sobre la mortalidad a corto plazo, pero no es asociado con la progresión de la enfermedad oncológica.