Surgery is the only potentially curative treatment for colorectal cancer liver metastases (CRLM) and its indication and results have varied in the last 30 years.
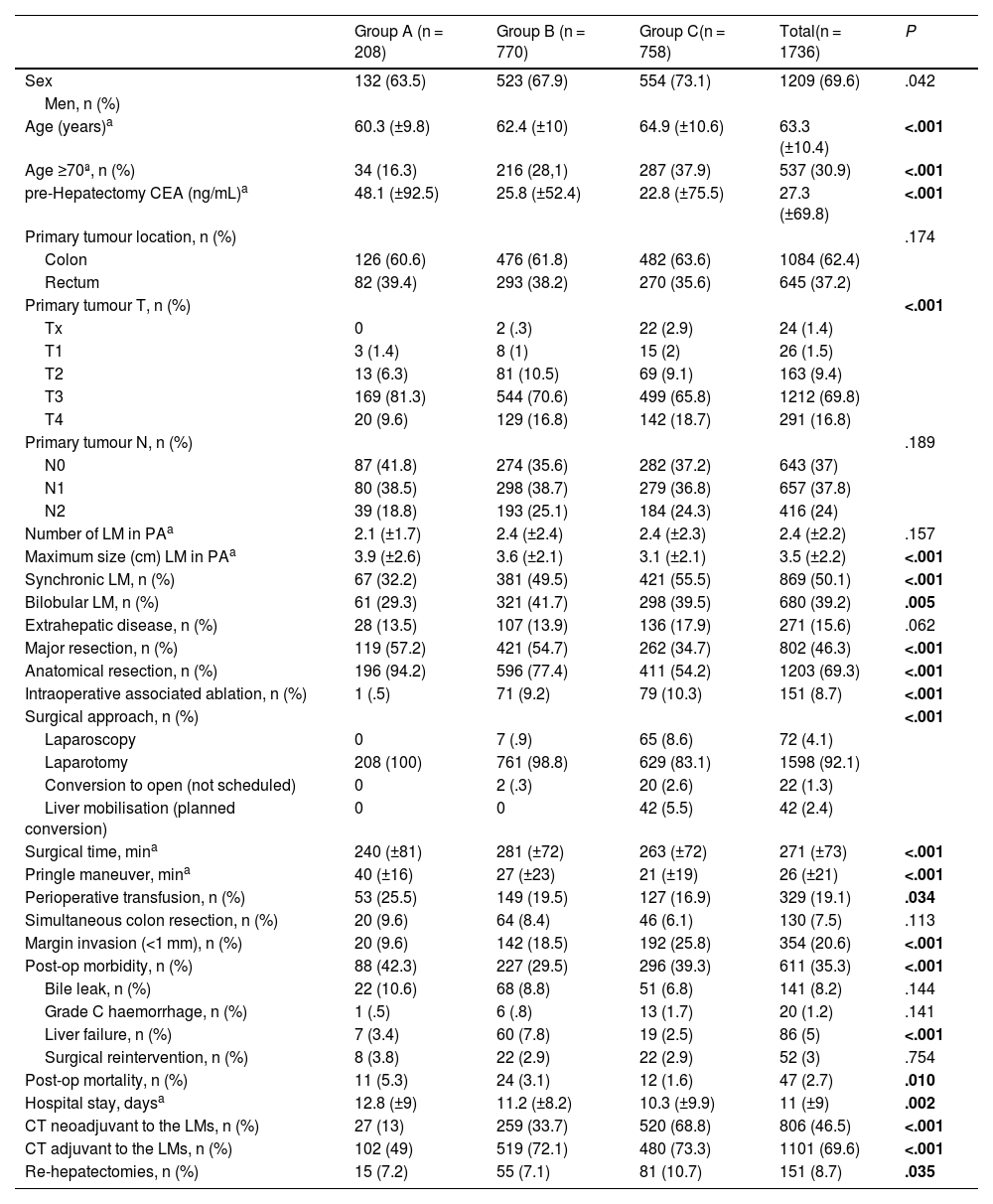
MethodsAll patients operated on for CRLM in our centre from 1990 to 2021 were prospectively collected, establishing 3 subgroups based on the year of the first surgery: group A 1990–1999, group B 2000–2010, group C 2011−2021. Clinical characteristics and the results of survival, recurrence and prognostic factors were compared.
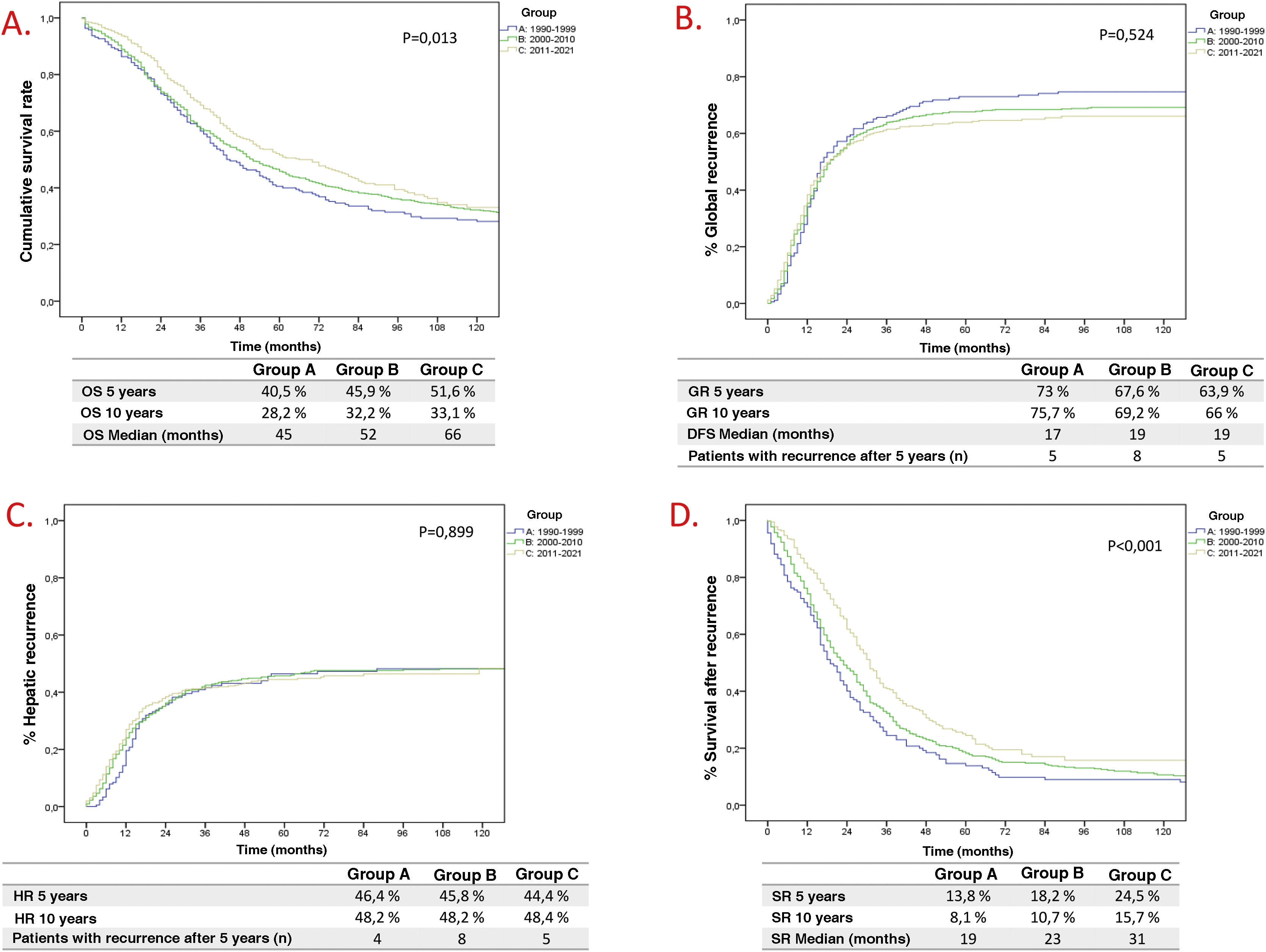
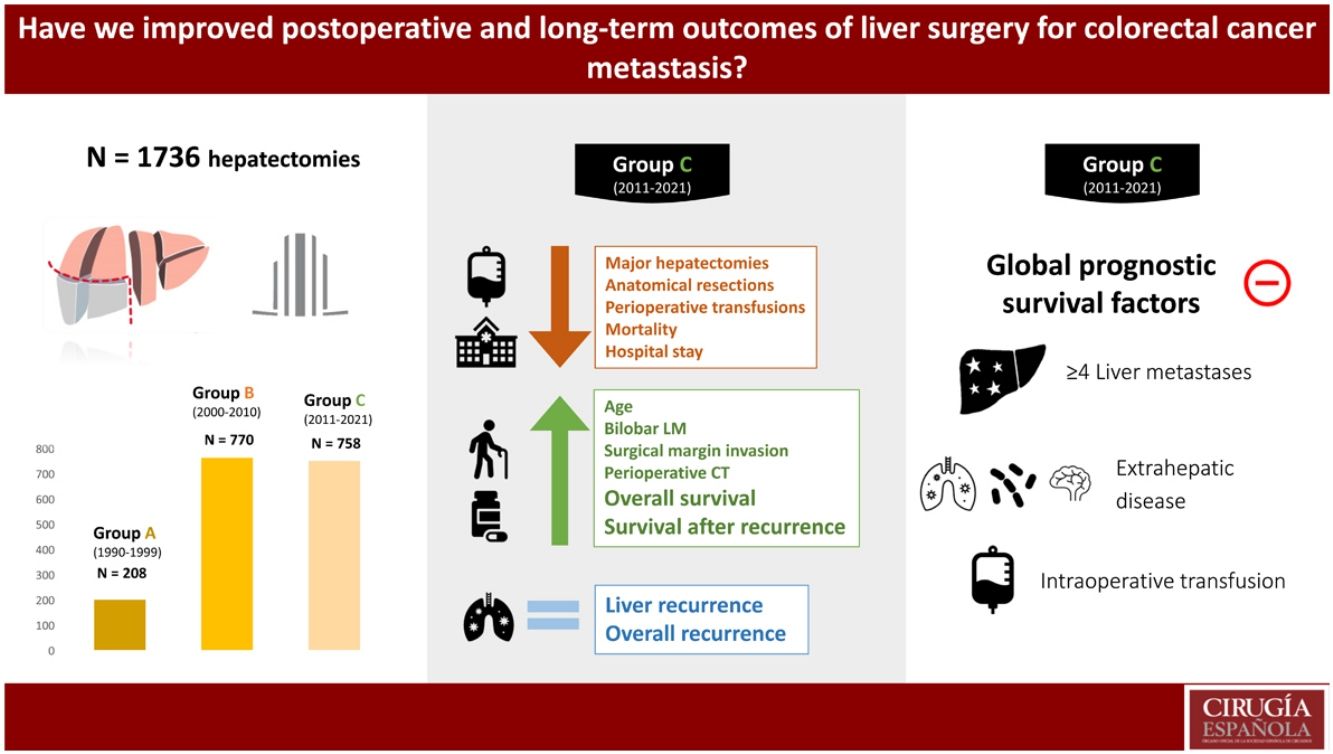
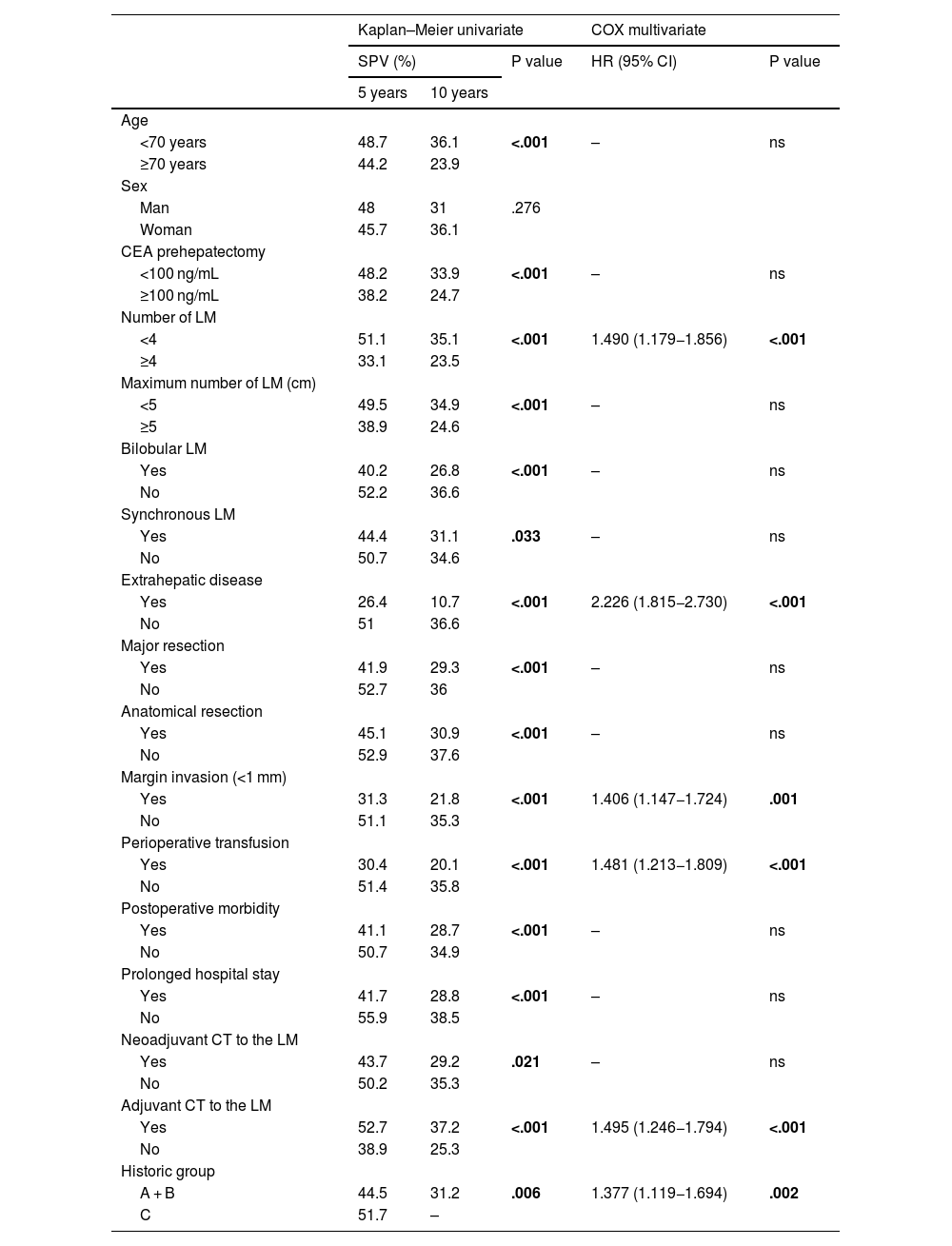
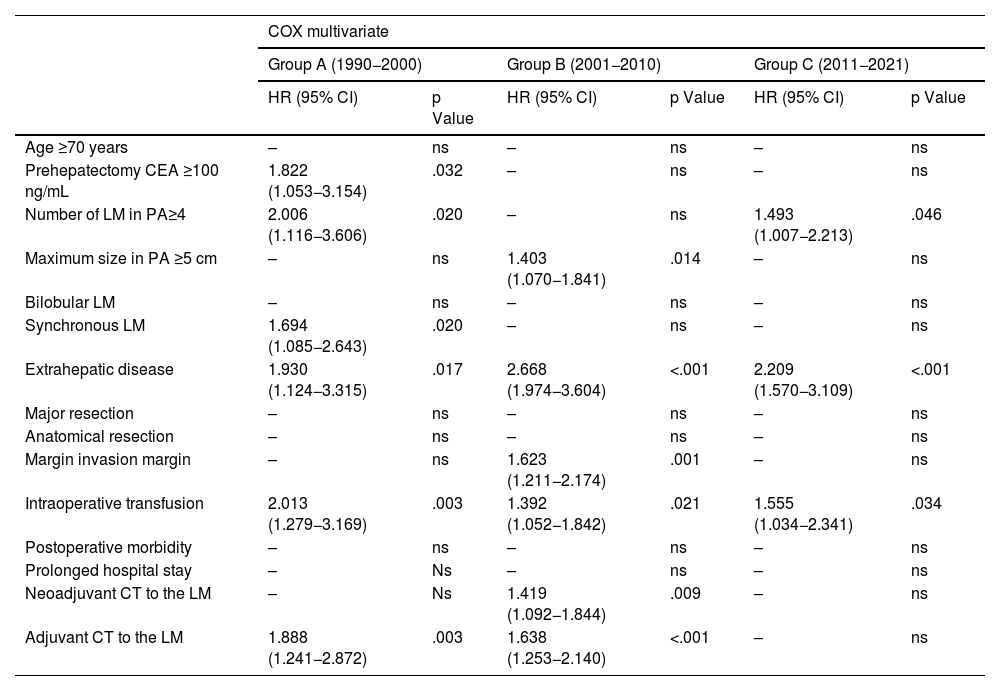
Results1736 hepatectomies were included (Group A n = 208; Group B n = 770; Group C n = 758). Patients in group C had better survival at 5 and 10 years (A 40.5%/28.2%; B 45.9%/32.2%; C 51.6%/33.1%, p = 0.013), although there were no differences between groups in overall recurrence at 5 and 10 years (A 73%/75.7%; B 67.6%/69.2%, and C 63.9%/66%, p = 0.524), nor in liver recurrence (A 46.4%/48.2%; B 45.8%/48.2%; and C 44.4%/48.4%, p = 0.899). An improvement was observed in median survival after recurrence, being 19 months, 23 months, and 31 months (groups A, B and C respectively). Prognostic factors of long-term survival changed over the 3 study periods. The only ones that remained relevant in the last decade were the presence of >4 liver metastasis, extrahepatic disease at the time of hepatectomy, and intraoperative blood transfusion.
ConclusionsSurvival after surgery for CRLM has improved significantly, although this cannot be explained by a reduction in overall and hepatic recurrence, but rather by an improvement in post-recurrence survival. Involvement of the resection margin has lost prognostic value in the last decade.
La cirugía es el único tratamiento potencialmente curativo de las metástasis hepáticas de cáncer colorrectal (LMCCR) y su indicación y resultados han variado en los últimos 30 años.
MétodosTodos los pacientes operados por LMCCR en nuestro centro de 1990 a 2021 fueron recogidos prospectivamente, estableciendo 3 subgrupos en función del año de la hepatectomía: grupo A 1990–1999, grupo B 2000–20010, grupo C 2011−2021. Se compararon características clínicas, supervivencia, recidiva y factores pronósticos.
ResultadosSe incluyeron 1736 hepatectomías (Grupo A n = 208; Grupo B n = 770; Grupo C n = 758).En el grupo C mejoró la supervivencia a 5 y 10 años (A: 40,5%/28,2%; B: 45,9%/32,2%; C: 51,6%/33,1%, p = 0.013), sin encontrar diferencias en recidiva global a 5 y 10 años (A: 73%/75,7%; B: 67,6%/69,2%, C: 63,9%/66%, p = 0,524), ni en recidiva hepática (A: 46,4%/48,2%; B: 45,8%/48,2%; C: 44,4%/48,4%, p = 0,899). Se observó una mejoría en la supervivencia mediana tras recidiva, siendo de 19 meses, 23 meses y 31 meses (grupos A, B y C respectivamente). Los factores pronósticos de supervivencia a largo plazo variaron en las 3 épocas, los únicos que mantuvieron relevancia en la última década fueron la presencia de >4 metástasis, la enfermedad extrahepática al momento de la hepatectomía y la transfusión perioperatoria.
ConclusionesEn los pacientes operados por LMCCR la supervivencia ha mejorado de forma significativa, sin que pueda explicarse por una reducción de la recidiva global y hepática, pero si por una mejoría de la supervivencia después de la recidiva. La afectación del margen de resección ha perdido valor pronóstico en la última década.