Asthma and other inhaled allergies are some of the most common paediatric diseases. The association of exposure to allergens with induction and exacerbation of symptoms has been proven. The majority of allergens are permanently or periodically suspended in the air, which leads to impaired quality of life for sensitive patients. Therefore, many methods of prevention and therapy of allergic diseases have been developed. The method of allergen exposure avoidance is often the first and the most significant measure. The present research has been conducted to evaluate, based on scientific data, which measures have the most reliable evidence of effectiveness. Environmental allergen avoidance methods, despite limited evidence supporting their clinical efficacy, are listed as the main therapeutic approaches in most recommendations. The significance of the holistic approach is also emphasised: only simultaneous introduction of several avoidance methods can bring possibly beneficial effects for the patient.
Sensitisation to inhaled allergens is considered the main factor contributing to the development of bronchial asthma and allergic rhinitis. Exposure to inhalant allergens is common, which is reflected in data showing that sensitisation to inhaled allergens in four-year-olds (19.2%) is much more common than sensitisation to food allergens (3.5%).1 That is why most clinical guidelines recommend identification of the allergen that triggers clinical signs and symptoms, and then intervention to decrease its negative influence.
The guidelines indicate that in order to relieve clinical signs and symptoms linked with allergy, the triggering allergens should be avoided, which should be one of the first recommendations issued during an allergic consultation.2 Hence attention should be paid to the most current attitudes towards theoretical and practical aspects of environmental intervention aiming at the prevention of inhaled allergy symptoms.
To date, hundreds of inhalant allergens have been identified, all of them capable of inducing clinical signs and symptoms of allergy, and many more are awaiting identification. However, of all these allergens, several most significant and widespread groups can be distinguished. These are allergens from house dust mites, pet fur, pollen, rodents, moulds and fungi, as well as cockroaches.
House dust mitesHouse dust mites, Dermatophagoides farinae and D. pteronyssinus, are a year-long source of allergens at home. Mites inhabit household environments and are found at the sites where dust and lost human epidermis accumulate. They need a warm and humid environment to develop (humidity of at least 50%). Their main reservoirs include: bedding, mattresses, pillows, carpets, clothes, and upholstery.3 More than 33 groups of mite allergens have been described so far, of which Der p1, 2, 23 and Der f1, 2, 23 induce IgE response in the majority of patients. These are mostly proteins contained within mites’ excrements, which persist in the air for approximately 30min after suspension.4,5
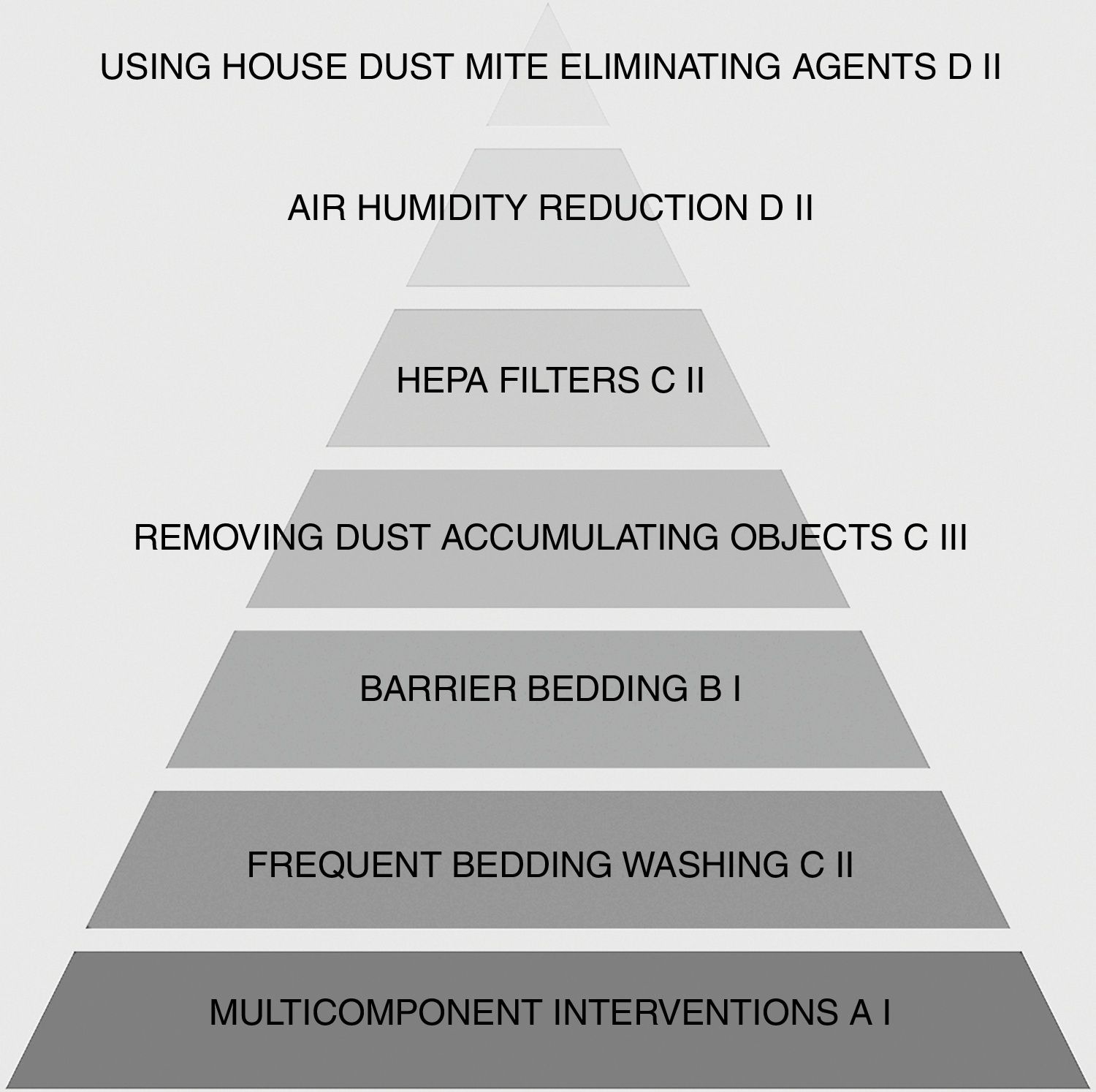
A number of methods to reduce exposure to allergens produced by house dust mites (HDM) have been developed. They are mainly based on direct elimination of mites from the household environment or removal of their allergens. However, there are no robust and unequivocal data to show the clinical efficacy of their application. Despite this, various guidelines do recommend the use of comprehensive mite elimination methods, which is dictated by the otential benefits associated with allergy symptom improvement.6
What allergen avoidance methods are worth recommending?Should special bedding (so-called barrier bedding) be recommended?Pillows, duvets and mattresses are the primary sources of mite-produced allergens in a household. Of various available technologies, exposure can be significantly reduced only by allergen- and mite-proof covers. It is crucial to apply materials with a pore diameter lower than 10 μm: this guarantees allergen-impermeability, and, at the same time, enables free air inflow, without which the comfort of use would be unsatisfactory for most patients.7 However, according to the current scientific knowledge, their isolated use, uncombined with any other anti-allergy method, is insufficient to achieve better control of asthma and exacerbations, does not reduce required steroid doses, and has no positive impact on the quality of life (QoL). All of this is true despite their supported efficacy in reducing HDM-allergen exposure.8
Should air humidity reduction be recommended?Mites need humidity of at least 50% to develop and reproduce. In order to decrease the size of the mite population, it seems reasonable to attempt to keep a humidity level in the household below this value. Unfortunately, there are no studies that would indicate unquestionable efficacy of lowering air humidity in relieving asthma symptoms.
Singh et al. demonstrated a statistically significant increase in peak expiratory flow (PEF) in evening measurements after 12 months of using humidity-lowering appliances.9 Sulser et al. maintained humidity constantly below 50% for 17 months and noted a reduction in live dust mites from 401/g of dust to 8/g of dust.10 However, difficulties associated with maintaining such values at home settings and the fact that even a transient increase in humidity for 1.5h enables dust mites to develop anew question the relevance of this intervention.3
Should chemical agents be applied to eradicate dust mites?It has been shown that the use of dust mite-eliminating agents, i.e. acaricides (benzyl benzoate, tannic acid), not only causes an insignificant and impermanent reduction in the number of dust mites, but that their population is rapidly restored after acaricide use. Furthermore, the direct effect of these chemical agents on the patient’s health is uncertain.7 That is why these chemicals are not recommended for patients with a house dust mite allergy.
What is the impact of washing bedding frequently?Various guidelines recommend washing all bedding at least once a week, ideally at a temperature of over 55°C, which, according to some studies, reduces the number of live dust mites practically by 100%.11 It has also been demonstrated that washing in low temperatures removes approximately 80% of mites and washing in low temperatures combined with automatic drying increased this rate to approximately 93%. A similar reduction rate concerned dust mite allergens.12 This effect may seem impressive, but still, evidence for the efficacy of this method as the only intervention to reduce clinical signs and symptoms is lacking. It occurs, however, that frequent washing in high temperatures is a justified element of a multicomponent intervention to reduce the number of dust mite allergens in household environments.13
Should carpets, window curtains etc. be removed?The presence of a carpet in a room has been associated with an increased number of house dust mite allergens. It has been shown that the presence of a carpet in a bedroom more than doubles the number of dust mite allergens in bedding. It therefore seems sensible to remove all carpets and other objects that might accumulate dust, such as upholstery, soft toys or blankets.5 Carpets have often been removed in multicomponent interventions, where significant allergen reduction rates have been achieved. However, outcomes pertaining to the severity of signs and symptoms as well as the number of exacerbations remain inconclusive.8 Further studies are therefore needed to establish the clinical usefulness of this method of secondary inhaled allergy prevention.
Should one purchase appliances with HEPA filters?High efficiency particulate absorber (HEPA) filters capture approximately 99.97% of particles with the diameter of at least 0.3μm. They can be used in air filters or vacuum cleaners. In some studies, the application of air filters equipped with the HEPA technology reduced symptoms of inhaled allergy, but only when combined with comprehensive methods of allergen exposure reduction.14 The use of a HEPA filter as a single method does not provide measurable clinical benefits.15–17
Very good outcomes have been obtained in studies with the use of filtering systems with a high-efficiency (120 m3/hour) laminar air flow system. In a study among 30 patients with moderate-to-severe and uncontrolled asthma, sensitised to at least one group of inhalant allergens (house dust mites/animal fur/moulds/others), the use of a device providing laminar flow of purified air in the bedroom at night for a year improved symptoms and enabled better asthma control. An annual asthma exacerbation rate was reduced from 3.6 to 1.3, and the hospitalisation rate dropped from 72% to 23%. The most significant evidence for the efficacy of the above-mentioned intervention seems to be the reduction of the rate of patients with uncontrolled asthma, which declined from 55% at baseline to 0% after 12 months of using TLA (temperature-controlled laminar airflow).18
Regular and frequent vacuuming with a vacuum cleaner fitted with HEPA filters offers a significant reduction in the concentration of dust mite allergens. Wu et al. reported a 10-fold reduction (from 4μg to 0.4μg) in the number of dust mite allergens in bedding that was vacuumed every day for eight weeks using a vacuum cleaner with a HEPA filter.19
To conclude, there is some evidence supporting the efficacy of devices equipped with filters (vacuum cleaners, portable devices, TLA), both those with HEPA filters and those using other methods of air filtration. The application of a filter itself provides minor clinical benefits. Taking into account the fact that HEPA filters affect only the number of allergens and not dust mites themselves, it must be underlined that the use of these technologies is justified only when combined with other comprehensive methods of dust mite and allergen reduction.20
Do multicomponent strategies work?There have been numerous studies evaluating the efficacy of comprehensive methods of allergen elimination, including HDM allergens. It seems that the clinical efficacy of this management cannot be confirmed either.21
A large, randomised clinical trial, conducted by Smith et al., has shown that, after 12 months using comprehensive methods of allergen elimination from the environment of patients aged 6–16 years with asthma or allergic rhinitis, statistically clinical improvement, measured in the Rhino-conjunctivitis and asthma symptom score and Paediatric Allergic Disease Quality of Life Questionnaire (PADQLQ), occurred only for allergic rhinitis.22 It should be noted, however, that there have been no significant differences in the rate of patients reporting subjective improvement in allergy symptoms or in the number of days unable to pursue usual activities (Fig. 1).
Similar conclusions were also reached in 2014 by the authors of a meta-analysis of 14 randomised clinical trials on the avoidance of inhaled allergens, which included 4082 patients with a clinically confirmed inhaled allergy or a high risk of such an allergy.23 The only benefit in high-risk infants was demonstrated for the risk of asthma symptoms and wheezing. Allergen avoidance reduced neither the risk of atopic dermatitis, nor allergic rhinitis or cough in these infants. Patients previously sensitive to inhalant allergens (usually house dust mites and cockroaches) showed no improvement in general pulmonary efficiency after the implementation of allergen avoidance methods, but a significant reduction was noted for the number of days with asthma symptoms.
Owing to these results, the Global Initiative for Asthma (GINA) currently does not recommend the widespread use of comprehensive methods to avoid exposure to house dust mite allergens.
However, some authors question these conclusions and suggest that “multifaceted interventions are effective in reducing exposure to triggers, decreasing asthma symptoms and acute health-care use, and improving quality of life”.24
Moreover, a review25 of 23 original studies on the use of combined interventions for allergen avoidance has shown benefits in the form of fewer days with asthma symptoms (a mean reduction by 21 days annually), fewer missed days at school (a mean reduction by 12.3 days annually) and approximately 0.57 Emergency Department visit less. However, no significant improvement in physiological asthma parameters (%FEV1) was shown, and a negligible number of studies on the use of these methods included adults. The study also underlines the efficacy and value of home visits to ensure doctor–patient alliance in implementing methods of allergen exposure avoidance in home settings.
Based on these data, one cannot recommend multicomponent interventions in treating and mitigating allergy symptoms with full certainty. Proper use of several of these interventions will surely reduce allergen exposure and is associated with high costs, but will never warrant clinical benefits.
Nevertheless, the authors of this article, taking into account the results of at least several well designed and performed clinical trials,14,25 are convinced that a well performed avoidance regime consisting of multiple avoidance measures may be successful in alleviating allergy symptoms in selected patients.
Furry petsAnimals are a frequent source of inhaled allergens in home settings and in schools, universities, workplaces and public places. As estimated by Rönmark, E. and Bjerg, A. et al. in 2009, cat and dog allergies account for 19.1% and 15.7% of school-age allergies, respectively. Multicentre, cross-sectional studies have shown that hypersensitivity to inhaled dog and cat allergens is significantly associated with the incidence and severity of asthma exacerbations, the amount of and frequency of bronchodilators usage, and FeNO increase.26 According to the estimates of Statista.com made in 2017, there are 102.7 million cats and 85 million dogs in European households, which translates into 42% of European households with at least one pet.27 Moreover, it is observed that the number of pets is rising worldwide, particularly in developing countries. This leads to increased exposure to allergens produced by animals with fur. The risk concerns not only individuals living at a house with a pet, but also, as shown in research, a marked risk of asthma exacerbation is present in, for instance, classmates of these individuals.28
Attention should also be paid to the phenomenon of cross-reactivity, i.e. a situation when allergens from various sources may induce allergy symptoms in one individual. In this field, there are numerous case reports. An example may be that of a Polish patient allergic to cat-produced Fel d 1, who developed a severe allergic reaction upon contact with big cats from the family of Felidae in a circus.29
The most common inhalant allergens secreted by pets are: Can f 1, produced mainly in canine sebaceous glands and present in large quantities in dog’s fur, epidermis and saliva; it is responsible for approximately 70% of hypersensitivity reactions to dog allergens, and Fel d 1, the main cat allergen, produced in the feline salivary, lacrimal and sebaceous glands; even as many as 95% of patients allergic to cat allergens react to it. These allergens are transferred to the human respiratory tract on the animal epidermis with a diameter below 5μm that is suspended in the air. Another animal-produced allergen frequently present in households is Mus m 1. It occurs in the murine epidermis, fur and urine and is found in greater quantities in households of people with a low financial status.
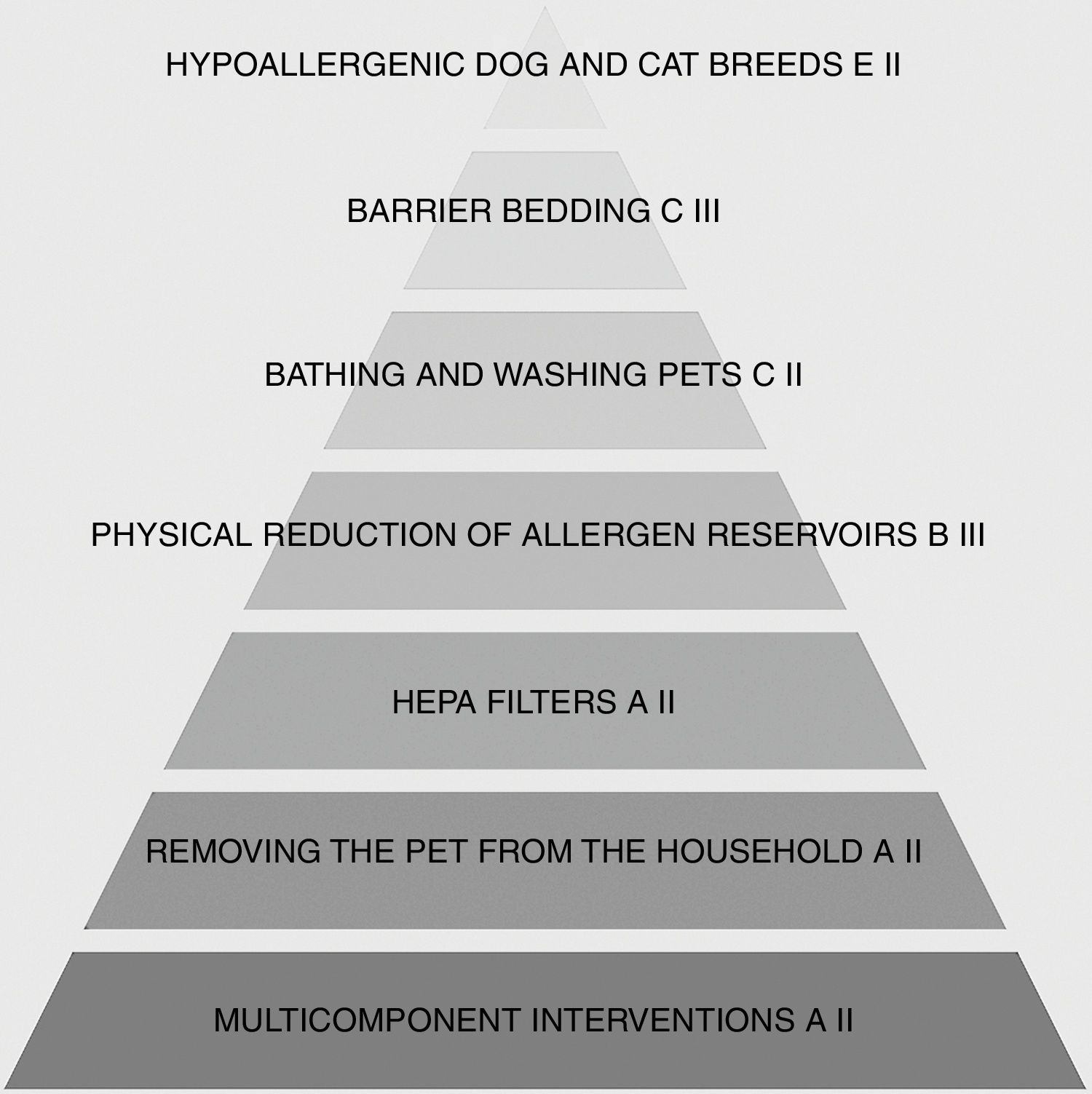
What allergen avoidance methods are worth recommending?Should the favourite pet be removed from the household?The easiest and the most effective animal allergen avoidance method that is recommended by numerous allergy associations is removal of a pet from the household. This inhibits the processes of an increase of inhaled allergens in the patient’s environment, and, with additional allergen elimination methods, facilitates their reduction. Unfortunately, for many reasons, particularly emotional, this intervention is often unacceptable to patients and compliance rates are negligible.30 In two studies conducted in Colombia and Sweden, only 4% and 8.5% of patients, respectively, removed their pets to which they were surely allergic after receiving clear medical recommendations to do so.31,32 Keeping pets outside the house or restricting their access to certain rooms, mainly bedrooms, is a less restrictive intervention. However, as pet-produced inhaled allergens are easily airborne and can be transmitted on clothes, as well as due to their thermal stability and long degradation time (cat allergens persist for an average of 24 weeks after stopping the contact with a cat), this intervention is not fully effective.33
Are air purifiers worth installing?As with allergy to house dust mites, pollen or fungi, air filters and purifiers fitted with a HEPA system are a frequently recommended method of reducing the quantity of inhalant allergens derived from pets. Based on a current literature review, the most effective, from the efficacy and economic viewpoints, are free-standing, portable HEPA filters, central air filtration systems and laminar air flow systems. Unfortunately, reports on their efficacy are conflicting. Sulser et al. have shown that 12-month usage of laminar flow filters only slightly reduced the quantity of inhalant allergens in the air and did not significantly affect bronchial hypersensitivity.10 Nevertheless, another study, conducted by Sicco van der Heide et al., revealed that three-month use of a HEPA air purification system significantly reduced bronchial reactivity and decreased the amplitude of PEF (Peak Expiratory Flow).34 Despite inconsistencies and doubts regarding the efficacy of this method in animal-produced inhalant allergen reduction, it seems to be worth recommending and can be used as part of a multifaceted approach.35
Frequent and intensive cleaningAn important intervention reducing the quantity of allergens in households is physical reduction of allergen reservoirs, such as removal of carpets, old furniture, meticulous cleaning, vacuuming and removal of toys, especially soft toys. These methods are particularly efficacious in combination with removal of a pet from the household or with other above-mentioned interventions, and when used regularly. Unfortunately, the constant presence of a pet in the house will render these measures eventually ineffective. High temperatures have no effect on reducing the quantity of inhalant allergens as they are characterised by high thermal stability. After application of a temperature of 140°C for 60min, 50–70% of cat and dog allergens remained unchanged.36
Should pets be washed frequently?Bathing and washing pets is another frequently used method of reducing the number of inhaled allergens in the patient’s environment. As shown in the research, this leads to a reduction of cat and dog allergens, but has no effect on clinical signs and symptoms. This is mainly due to the long preservation of allergens in the environment and rapid reproduction of primary (i.e. from before washing) allergen concentrations in the air. It has been shown that a significant reduction of Can f 1 can be achieved when dogs are washed twice a week.37
Are there any hypoallergenic dog and cat breeds?It is a common phrase that certain dog and cat breeds are “hypoallergenic.” Numerous studies have revealed that the number of allergens in animals depends on various factors, such as sex or age, and is characterised by individual variability.38
It must be underlined, however, that no statistically significant conclusions pertaining to the presumed hypoallergenic nature have been drawn for any breeds.39
Are special types of bedding worth recommending?As with HDM, attempts are made at animal-produced allergen avoidance by using barrier duvet and pillow covers with pores smaller than 6μm. They have been shown to reduce the quantity of allergens in bedding. Unfortunately, no significant evidence for a reduction of asthma symptoms and other allergic diseases has been provided so far. It is worth remembering, however, that bedding without barrier covers is an important reservoir for various allergens.30
Do multicomponent strategies work?Although removing the pet from the household clearly is the best way to reduce allergen exposure there are many cases when, due to many reasons, mostly emotional, this intervention is unacceptable to patients. In these situations introducing a combination of allergen avoidance measures, such as removing reservoirs (carpets, window curtains etc.), keeping the pet out of the bedroom, washing the pet twice a week, using HEPA filters in room air cleaners and vacuum cleaners and buying barrier bedding may be helpful. This may lead to a reduction of allergen concentration in the household environment but achieving clinical improvement remains uncertain (Fig. 2).30
Should murine allergens befeared?The main technique for murine Mus m 1 avoidance is preventing the settling and reproduction of rodents in the household environment. Food should be stored adequately, household wastes disposed of properly and rat disinfestation conducted when needed. It is also recommended to seal any holes that may constitute a potential mouse habitat. Studies recently published in JAMA reported a significant reduction in the concentration of murine allergens in house dust and air after the implementation of multicomponent interventions for murine allergen removal. At least a 75% reduction in a murine allergen concentration in house dust was obtained in 58% of investigated households.40
PollenOne of the most common groups of allergens comprises pollen of trees, grasses and other plants. Their increased air concentration, noted in the pollination period typical of a given plant, leads to the exacerbation of allergic diseases, mainly asthma, allergic rhinitis or allergic conjunctivitis in sensitive individuals. Pollen concentrations vary depending on different factors, such as the time of day, climate conditions and temperature.
The phenomenon of asthma exacerbations occurring during and directly after heavy storms has recently been reported.41,42 This is explained by release of allergen particles from plant seeds upon contact with rain. This may be caused by seed microruptures resulting from osmotic differences between plant tissue and water.43
What allergen avoidance interventions are worth recommending?Due to the widespread presence of plants and their pollen in the environment, total elimination of allergen exposure is impossible. There are, however, various methods that can reduce the exposure to a sensitising factor, mainly during the periods of its highest air concentration.
What should be recommended when one needs to go outside?The most often recommended strategies include shutting windows and doors, avoiding going outside and, when returning home, washing clothes, taking a bath, wearing glasses to protect eyes from contact with allergens, using HEPA filters at home and on air-conditioning systems in the car.
It must also be underlined that patients must be aware of which pollen sensitises them. In that way they know when to exercise these pollen avoidance measures to gain most benefit.13 At present, there are various methods and smartphone applications that support patients’ knowledge regarding pollination periods.44
Fungi and mouldsAnother significant factor affecting the incidence, frequent recurrences and exacerbations of asthma symptoms and of other allergic diseases caused by inhaled allergens are spores and fungal allergens present in households.45 Visible moulds are often conglomerates of various species, usually of the Penicillium, Alternaria, Cladosporium, and Aspergillus genera. The exacerbation of symptoms caused by sensitisation to fungal spores is observed from spring to autumn.46 It is estimated that even 20–40% of houses in Northern Europe and Canada and 40% of houses in the USA are highly contaminated with mould and fungal allergens.47
The use of appropriate mould removal methods in houses is highly effective in reducing symptoms associated with inhaled allergies and asthma.48,49
What allergen avoidance methods are worth recommending?The basic method of avoiding inhaled allergens produced by moulds is elimination of all mouldy areas.49 Mould is often found on ceilings, walls, floors, carpets and toys. These surfaces should be cleaned with agents containing antifungal substances and additionally frequently dried and vacuumed.
What should be done at home?The application of proper drying and mould removal methods may result in an even 20-fold decrease in the number of mould spores suspended in the air. If a given area cannot be cleaned in a satisfactory way, it or its part (e.g. a part of wallpaper, wood panelling, carpet) should be removed. This is often required in old houses or after flooding. Reducing air humidity, ideally to below 50%, is an important measure in reducing the number of fungal allergens. This can be achieved by installing and using ventilators in rooms with greater humidity (especially in bathrooms, cellars or attics), sealing and insulating pipes and places of leaks or water deposition, reducing the number of plants that need frequent watering as well as using ventilation and air-conditioning in months when air humidity is increased.46 Frequent sites for allergy-causing fungus presence are air-conditioning devices in both houses and cars. They should be often inspected and filters replaced as, instead of decreasing the number of allergens in the patient’s environment, they may contribute to greater air contamination with spores and fungal allergens.
What should be done outside the house?As in the case of pollen, it is possible to determine the circumstances at which the risk of increased fungal spore concentrations in the air is high. This usually happens in the summertime, with given species characterised by different preferences concerning air humidity. Owing to the widespread presence and the impossibility to remove fungi from the environment, the only sensible strategies seem to be staying indoors when the concentration of spores is at its highest, using HEPA filters at home and taking a bath upon returning home. The aforementioned smartphone applications may also come in handy.50
CockroachesCockroaches, due to secreting small protein particles with a sensitising potential, are another factor contributing to the development of allergic diseases and to increased allergy-related hospitalisation rates. The presence of cockroaches is usually associated with a low socio-economic status, neglected household hygiene and inappropriate disposal of household wastes. A reduction in the number of deaths among children from poorer districts with sensitivity to inhaled allergens produced by cockroaches has been correlated with the implementation of effective methods to reduce the number of cockroaches and their habitats. This has also led to a decline in the number of exacerbations and severity of asthma and allergy symptoms in these children.51,52
What allergen avoidance interventions are worth recommending?There are various methods and recommendations that can contribute to a reduction in the concentration of cockroach-produced allergens in an environment. The most significant is eradication of cockroaches by their direct extermination as well as regular and thorough house cleaning to remove their habitats. The use of insecticides and cockroach traps is also recommended. Moreover, it is important not to leave leftovers, which are the main sources of food for these pests. Unfortunately, as studies indicate, even systematic use of these comprehensive interventions for over 12 months may not reduce the concentration of allergens to the level that does not trigger symptoms.51,53
ConclusionsEnvironmental interventions preventing inhaled allergen exposure are listed as the major element of primary prevention and treatment of allergy symptoms in numerous guidelines despite the lack of unequivocal evidence for their clinical efficacy. The relevance of multicomponent interventions is also underlined as only simultaneous use of several allergen elimination methods offers some clinical benefits for patients. Over the years, a number of ideas on reducing patient exposure to sensitising factors have emerged.
Conflict of interestThe authors have no conflict of interest to declare.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. English proof reading assistance was funded by Fundacja Respira.