We aimed to evaluate how the corona virus disease of 2019 (COVID-19) outbreak influenced emergency department (ED) admissions for urolithiasis, hospitalizations and clinical management of the hospitalized Patients.
Patients and methodsWe conducted a multicentric retrospective analysis of ED admissions in three high volume urology departments (one directly involved in COVID-19 patients management and two not involved) in Rome - Italy between March and April 2020 and in the same period of 2019. Statistical analysis was conducted on the number of admissions for urolithiasis, rate of complications, hospitalization and the type of treatment received.
Results304 patients were included in the analysis. A significant reduction in the global number of patients admitted to ED for urolithiasis between 2019 and 2020 (48.8%) was noted. Moreover, regarding the choice of treatment of hospitalized patients, a statistically significant increase of stone removal procedures versus urinary drainage was reported in 2020 (P = .015).
ConclusionsDuring the COVID-19 pandemic in Rome there has been a significant reduction of emergency admissions for urolithiasis. Patients admitted to ED had more complications, more frequently need hospitalization and regarding clinical management early stone removal was preferred over urinary drainage only. All the urologists should be aware that in the next months they could face an increased number of admissions for urolithiasis and manage more complicated cases.
Nuestro objetivo fue evaluar el impacto de la enfermedad del coronavirus de 2019 (COVID-19) en los ingresos en los servicios de urgencias (SU), las hospitalizaciones y el manejo clínico de los pacientes con urolitiasis.
Pacientes y métodosRealizamos un análisis retrospectivo multicéntrico de las admisiones en los servicios de urgencias de tres departamentos de urología de gran volumen (uno directamente implicado en el tratamiento de los pacientes de COVID-19 y dos no implicados) en Roma (Italia) entre marzo y abril de 2020 y en el mismo período de 2019. Se realizó un análisis estadístico del número de admisiones por urolitiasis, la tasa de complicaciones, hospitalización y el tipo de tratamiento recibido.
Resultados304 pacientes fueron incluidos en el análisis. Se observó una reducción significativa en el número global de pacientes ingresados en urgencias por urolitiasis entre 2019 y 2020 (48,8%). Además, con respecto a la elección del tratamiento de los pacientes hospitalizados, se informó un aumento estadísticamente significativo de los procedimientos de extracción de cálculos en comparación con el drenaje urinario en 2020 (P = ,015).
ConclusionesDurante la pandemia de COVID-19 en Roma ha habido una reducción significativa de los ingresos en urgencias por urolitiasis. Los pacientes ingresados en el SU tuvieron más complicaciones, necesitaron hospitalización con mas frecuencia y en cuanto al manejo clínico, se prefirió la extracción temprana de los cálculos en vez del drenaje urinario. Todos los urólogos deben ser conscientes de que en los próximos meses podrían enfrentarse a un mayor número de admisiones por urolitiasis y al manejo de casos más complicados.
Urolithiasis is a common disease worldwide, affecting roughly 9% of the US population and renal colic represents an actually relevant cause of emergency department (ED) visit.1,2 In Italy there is an estimated prevalence of 7.5% in the population older than 18 years.3 Urolithiasis represents a frequent cause of ED admissions, accounting for 1%–2% of emergency visits4: in a report from a large series of patients admitted to ED in a big Italian hospital, 16% of patients with non-traumatic abdominal pain had a diagnosis of renal or ureteral stone.5 In a report from the US about the percentage of patients admitted to ED for urinary stones that received a urologic treatment in the next days after the emergency visit, only 5% of the patients were treated by a urologist in the 7 days after the visit and only 12.6% in the next 90 days.6 In a similar analysis from South Korea, the patients admitted to ED for stone disease were 336,711 and 13.2% needed to be hospitalized for a treatment.7 Therefore, we can assume that renal colic is a relevant disease in emergency, accounting for 1%–2% of emergency visits, but only few patients experience a real emergency and need hospitalization and surgical treatment.
After the lockdown of initial foci of the corona virus disease of 2019 (COVID-19) in northern Italy, a national quarantine was imposed at the beginning of March in order to restrict the movement of the population only for necessity, work and health circumstances, with the closure of non-essential activities. During the lockdown a lot has changed in hospital departments, from ED to elective surgeries.
In Italy not all the regions were affected by the same overload of COVID-19 cases; some cities had the opportunity to select the hospitals in which infected patients had to be admitted, leaving some structures free from COVID-19 patients. Therefore, in Rome some hospitals were almost exclusively dedicated to the management of the pandemic and became the referral centers for all other emergency departments in the city.
Aim of this study was to explore how the COVID-19 emergency influenced ED admissions for urolithiasis, hospitalizations and urologic management of the hospitalized Patients.
Materials and methodsWe performed a multicentric retrospective analysis of ED admissions for urolithiasis in three high volume urology department (>100 surgical procedures for stone disease per year) in Rome - Italy between March and April 2020 and in the same period of 2019.
Data from three different hospitals were collected: two hospitals that were not involved in COVID-19 patients’ treatment (Centre 1 and 2) and were therefore labelled as non COVID-19 hubs. One hospital was a COVID-19 referral center with dedicated areas (Centre 3) and was labelled as COVID-19 hub.
All Patients underwent radiological imaging with abdomen ultrasound or low dose computerized tomography, in order to confirm the diagnosis of urolithiasis. Demographics and clinical key data were reported on a standardized study proforma as well as the occurrence of any complication such as fever, acute kidney failure or perinephric fluid collection. The total number of ED admissions for any cause and for urolithiasis, the number of patients hospitalized, and the type of treatment received were also reported.
The relationship between the time of admission and the other variables was studied using non-parametric tests (Chi Square and Mann-Whitney). Statistical significance was considered at P < .05. All analyses were performed with SPSS 25 (IBM corp, Armonk, NY, USA). Data were analyzed globally and for single centers, therefore stratified in COVID-19/non COVID-19 hub.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent was not required.
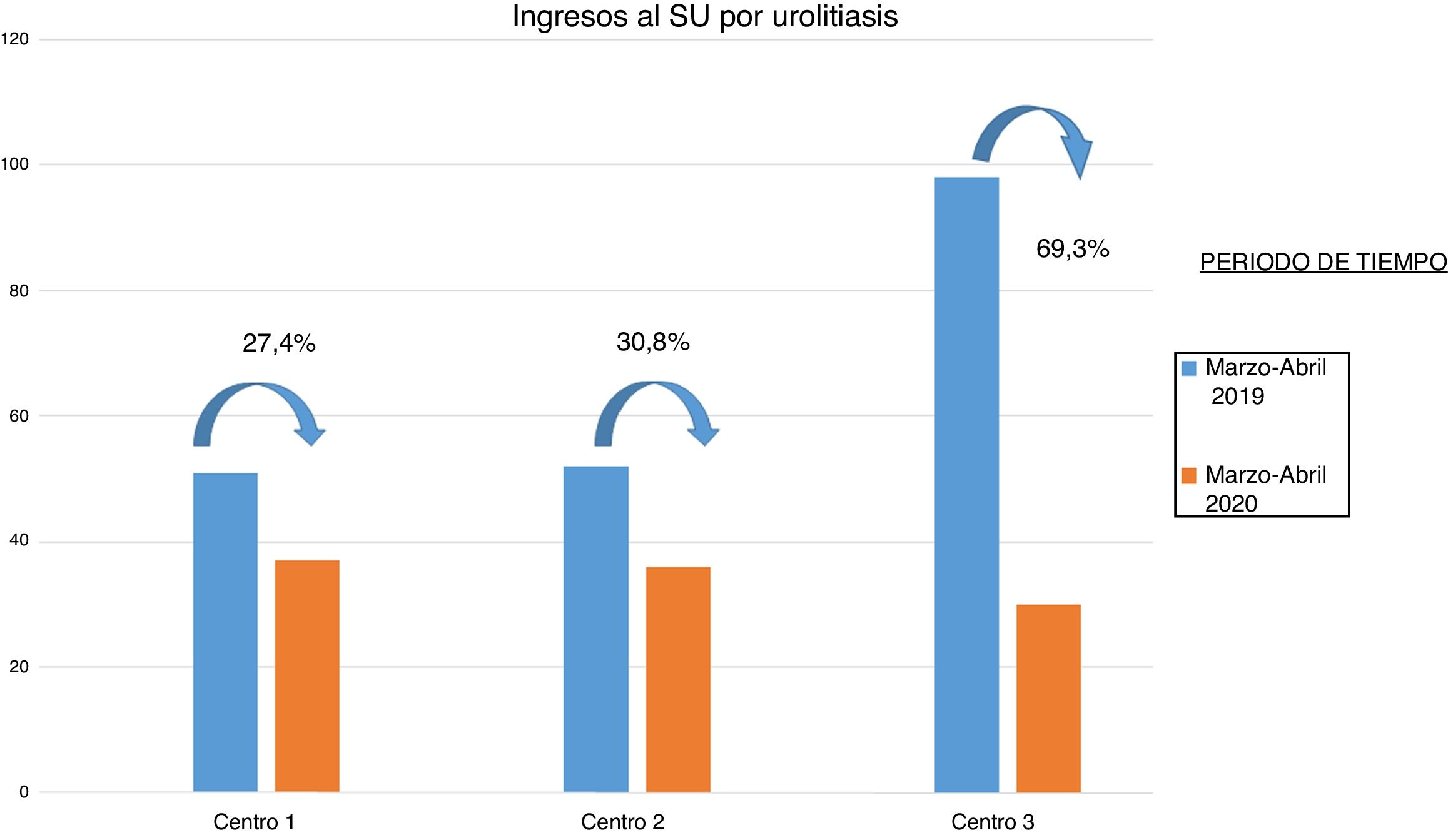
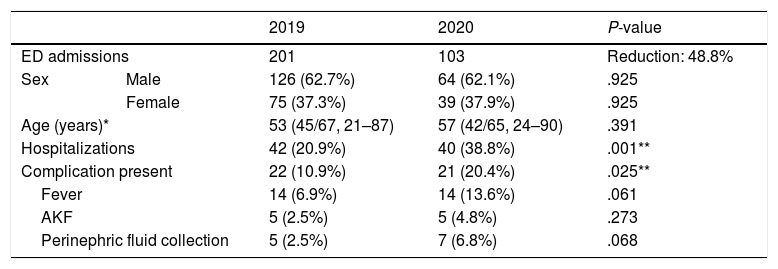
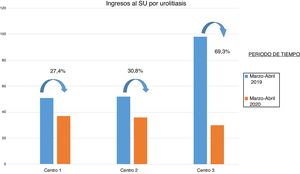
ResultsOverall, we evaluated 304 patients admitted to ED for flank pain associated with urolithiasis. The total number of admissions decreased of 48.8% (201 in 2019 vs 103 in 2020). The largest decrease was noted in center 3 (COVID-19 hub) where the reduction of admissions was 69.3% compared to 2019, but also in center 1 and 2 (non COVID-19 hubs) a reduction of roughly 30% of admissions was reported (Fig. 1). Regarding patient’s characteristics the results, stratified by year of admission, showed a statistically significant difference in hospitalization rate (P = .001) and presence of associated complications (P = .025) (Table 1). Considering gender and age, no statistically significant differences have been noticed between 2019 and 2020.
Characteristics of Patients admitted in ED with diagnosis of urolithiasis in March-April 2019 and 2020.
| 2019 | 2020 | P-value | ||
|---|---|---|---|---|
| ED admissions | 201 | 103 | Reduction: 48.8% | |
| Sex | Male | 126 (62.7%) | 64 (62.1%) | .925 |
| Female | 75 (37.3%) | 39 (37.9%) | .925 | |
| Age (years)* | 53 (45/67, 21–87) | 57 (42/65, 24–90) | .391 | |
| Hospitalizations | 42 (20.9%) | 40 (38.8%) | .001** | |
| Complication present | 22 (10.9%) | 21 (20.4%) | .025** | |
| Fever | 14 (6.9%) | 14 (13.6%) | .061 | |
| AKF | 5 (2.5%) | 5 (4.8%) | .273 | |
| Perinephric fluid collection | 5 (2.5%) | 7 (6.8%) | .068 | |
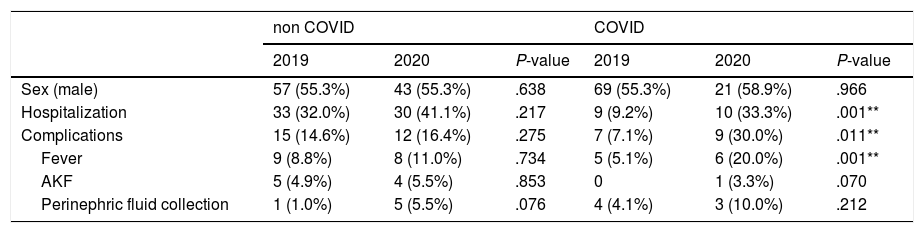
Table 2 shows sub-analysis of data stratified by non COVID-19 hubs (Centre 1 and 2) and COVID-19 hub (Centre 3). The difference in hospitalization rate and complications rate remained statistically significant only in center 3, but the percentage of hospitalization also in non COVID-19 hubs increased from 32% in 2019 to 41.1% in 2020.
Characteristics of Patients admitted from ED with diagnosis of urolithiasis in March-April 2019 and 2020, stratified by COVID-19 hubs.
| non COVID | COVID | |||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | P-value | 2019 | 2020 | P-value | |
| Sex (male) | 57 (55.3%) | 43 (55.3%) | .638 | 69 (55.3%) | 21 (58.9%) | .966 |
| Hospitalization | 33 (32.0%) | 30 (41.1%) | .217 | 9 (9.2%) | 10 (33.3%) | .001** |
| Complications | 15 (14.6%) | 12 (16.4%) | .275 | 7 (7.1%) | 9 (30.0%) | .011** |
| Fever | 9 (8.8%) | 8 (11.0%) | .734 | 5 (5.1%) | 6 (20.0%) | .001** |
| AKF | 5 (4.9%) | 4 (5.5%) | .853 | 0 | 1 (3.3%) | .070 |
| Perinephric fluid collection | 1 (1.0%) | 5 (5.5%) | .076 | 4 (4.1%) | 3 (10.0%) | .212 |
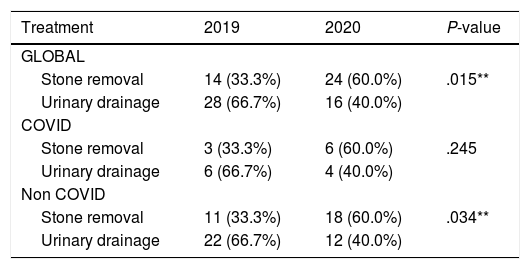
Table 3 shows treatment of the hospitalized Patients (endoscopic stone removal versus urinary drainage – stent or nephrostomy) which significantly differed between 2019 and 2020 (P = .015): 14/42 (33.3%) patients underwent stone removal versus 24/40 (60.0%) in 2020.
Treatment of hospitalized Patients admitted from ED with diagnosis of urolithiasis in March-April 2019 and 2020, stratified by COVID-19 hubs.
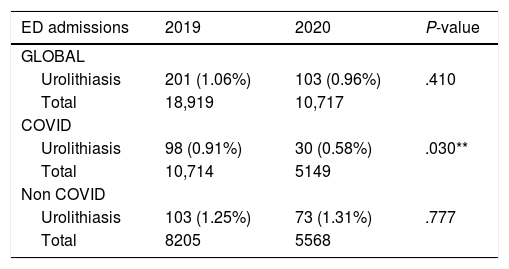
The percentage of patients admitted with a diagnosis of urolithiasis over the total number of patients admitted to ED (Table 4) showed a significant reduction (P = .030) in center 3, while it was roughly stable in center 2 and center 1.
Number of ED admissions for urolithiasis compared to total ED admissions.
| ED admissions | 2019 | 2020 | P-value |
|---|---|---|---|
| GLOBAL | |||
| Urolithiasis | 201 (1.06%) | 103 (0.96%) | .410 |
| Total | 18,919 | 10,717 | |
| COVID | |||
| Urolithiasis | 98 (0.91%) | 30 (0.58%) | .030** |
| Total | 10,714 | 5149 | |
| Non COVID | |||
| Urolithiasis | 103 (1.25%) | 73 (1.31%) | .777 |
| Total | 8205 | 5568 | |
As all the other specialties, even urology services have been affected by the COVID-19 outbreak, with a significant reduction of elective surgeries and outpatient visits, and sometimes with the need to reallocate manpower and resources to the frontline departments.8 Many urological societies have produced recommendations on urological diseases management, but currently there are no studies evaluating the impact of pandemic outbreak of COVID-19 on everyday practice. Therefore, we aimed to analyze how the COVID-19 emergency in our region influenced ED admissions for urolithiasis, hospitalizations and urologic management of the hospitalized Patients.
In order to reduce the risk that the results could be influenced by the overload of COVID-19 patients admitted to ED, data were collected from three different hospitals with different roles in the regional emergency plan. To our knowledge, this is the largest study evaluating ED admissions for urolithiasis in the period of the pandemic.
Our data analysis showed a general reduction of ED admissions for urolithiasis (48%) in the period of interest. A decrease of ED admissions for urological disease have been reported in the first period of the COVID-19 pandemic in some regions from the north of Italy.9 This reduction affected mostly renal colic, enforcing the idea that there is usually an abuse of hospital consultation from low complexity cases that could be managed outside the hospital. Our data show that the reduction of admissions, as expected, occurred mainly in Covid-19 hub (69.3%) but was relevant even in the other centers (27.4% and 30.8%).
This finding, according to other clinical report of different diseases,10 might be explained with the fear of contagion at the hospital that has reduced the access to ED for urolithiasis from non-urgent patients particularly after the diffusion by the media of the news about the spread of COVID-19 in hospitals and across healthcare workers. Regarding urolithiasis moreover, the reduction of ED admissions should be attributed to the increase of conservative medical therapy for stone disease in the pandemic period.
The percentage of patients with urolithiasis over the total number of patients admitted to ED are similar to literature.4 There was significant reduction (P = .030) in this percentage only for COVID-19 hub in 2020. This result might be attributed to the higher rate of ED admission of Patients with COVID-19 like symptoms, which accessed to that hospital during the period in exam.
Furthermore, a significant increase in hospitalization rate (P = .001) and presence of associated complications (P = .025) was also noted in patients during pandemic in 2020. These data enforce the idea that mostly real urgent patients have been evaluated in the pandemic period with worse clinical presentation and a higher need of hospitalization and surgical treatment. This trend also emerges in a recent online survey from the EULIS (European Association Urology Section of Urolithiasis) collaborative research working group involving urologists from all Europe.11 The majority stated that they changed the routine approach to elective surgery for renal stones; the paper also outlined how the management of patients in the emergency department have changed during the pandemic period. The urologists treated more patients with complicated urolithiasis such as patients with acute renal failure and pyelonephritis and only 6.4% of the respondents referred that the approach to stone patients in ED was the same as before.
As expected, the differences in hospitalization and complications were more evident in Covid-19 hub, in which the impact of pandemic was more significant and therefore mainly real urgent urolithiasis patients have been admitted to ED; however, even in the other two centers the percentage of hospitalization and complications were higher in 2020 compared to 2019.
Regarding treatment of the hospitalized Patients (endoscopic stone removal versus urinary drainage – stent or nephrostomy), a statistically significant difference was noted between 2019 and 2020. In further sub-analysis the difference was statistically significant only in non COVID-19 hub, but the results of COVID-19 hub might be related to the small numbers of procedures performed in 2020, which affected statistical significance.
Therefore, whenever possible considering the capacity and demand of all the clinical structures involved, the strategy of a surgical procedure with stone removal was preferred over the simple urinary drainage in order to completely treat the urolithiasis reducing the need for further hospital admissions.
On the other hand in the EULIS survey11 89.4% of the experts involved stated that they changed their treatment strategy for emergency patients, favoring drainage of the collecting system and postponing elective intervention for stones and 17% did not perform surgery at all during the period.
From our point of view, taking in account that the first aim is to keep all the possible resources for the emergency situation, the choice to postpone stone removal must be counterbalanced by the potential harms of a delayed surgery. The strategy of early stone removal, whenever possible, aimed to reduce the risk of an overload of complicated cases in the next months after the emergency as well as the risk of adding extra procedures to the overwhelmed waiting list in which all the elective patients have been already postponed.
Among urological diseases, urolithiasis represents the most frequent cause of ED admission and in the last decade the admissions for renal colic increased; moreover, even the number of emergency procedures increased probably due to the greater availability of specific equipment compared to the past.2
Despite this trend, there is not any clear guidelines regarding management of patients admitted to ED for urolithiasis. However, during the pandemic, some algorithms have been proposed in order to help urologists to better define the correct management of these patients and to ensure an adequate treatment especially in this period in which the availability of operating room and ventilators is scarce.12,13 In our opinion these algorithms might be useful also in the next months when we should expect an increase ED admissions for urolithiasis and probably a worsening in clinical presentation of stone patients (impacted ureteral stones, renal function impairment from long term obstruction, pyelonephritis) due to the reduced number of patients evaluated and treated during the pandemic outbreak.
Our study is not devoid of limitations. First, its retrospective nature. Nevertheless, the short period of data collecting in order to obtain rapid data analysis. Second, being multicentric it might suffer of lack of standardization due to different attitude of the urologists working in the centers. Third, the COVID-19 pandemic outbreak in Rome does not reflect the global situation; it might be comparable only to areas that have the same COVID-19 prevalence. Finally, a longer-term follow-up could highlight greater number of complications and strengthen our findings.
ConclusionsDuring the COVID-19 pandemic in Rome there has been reduction of ED admissions for urolithiasis, associated to an increase in complication rates and worse clinical presentation. “Early stone removal” strategy was preferred over urinary drainage only. Urologists should be aware that in the next future they could face and increased number of ED admissions for urolithiasis and manage more complicated cases, demanding attention by healthcare management and public regulatory agencies.
Conflict of interestThe authors declare that they have no conflict of interest.
Authors would like to acknowledge Colleagues and all the healthcare professionals working in the Emergency Departments at their institution for their outstanding effort during this pandemic period.
Please cite this article as: Antonucci M, Recupero SM, Marzio V, De Dominicis M, Pinto F, Foschi N, et al. El impacto de la COVID-19 en las admisiones al servicio de urgencias, hospitalizaciones y manejo clínico de la urolitiasis en el centro de Italia: análisis multicéntrico. Actas Urol Esp. 2020;44:611–616.