The first-line treatment for >2cm lithiasis is percutaneous nephrolithotomy (PNL), leaving flexible ureteroscopy (FURS) as a second option. In the present review, the stone-free rate and the complications of both techniques were evaluated in the treatment of 2–3cm stones.
Material and methodsSystematic review of studies that compared both techniques. Studies that were not comparative, as well as those carried out in the paediatric population or with <2cm or >3cm stones, were excluded.
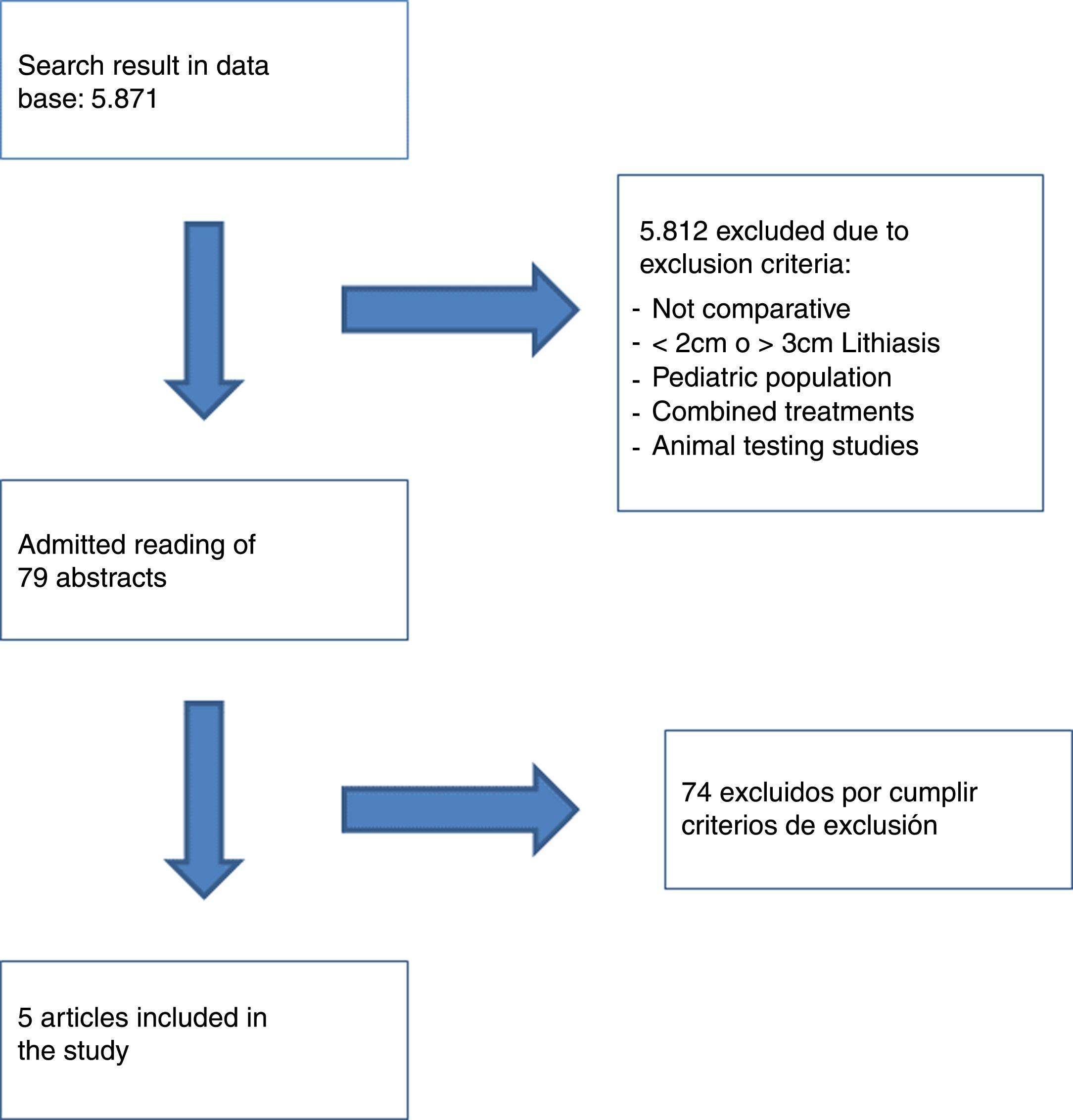
Two researchers independently performed the investigation, obtaining 5 studies that made up a total of 815 patients: 252 belonged to the FURS group and 563 to the PNL group. Four studies were retrospective, and one was non-randomised prospective.
ResultsStone-free rate ranged between 47.0% and 95.0% for the FURS and between 87.0% and 100% for the PNL. The complication rate was 8.8–29.0% in the FURS and 11.9–27.0% in the PNL. FURS required a greater number of procedures, and had a lower decrease in haemoglobin and creatinine rise compared to PNL.
ConclusionsThe stone-free rate was higher for PNL, although the FURS could reach comparable results at the expense of performing several procedures. Both techniques have a similar frequency of complications, but the PNL has more postsurgical analytical alterations.
El tratamiento de primera elección para litiasis >2cm es la nefrolitotomía percutánea (NLP), dejando a la ureteroscopia flexible (URS-F) como una segunda opción. En la presente revisión se evaluaron la tasa libre de litiasis y las complicaciones de ambas técnicas en el tratamiento de litiasis de tamaño entre 2 y 3cm.
Material y métodosRevisión sistemática de estudios que compararon las dos técnicas. Fueron excluidos aquellos estudios que no fueran comparativos, los realizados en población pediátrica o con litiasis menores de 2cm o mayores de 3cm.
Dos investigadores realizaron independientemente la búsqueda, obteniendo 5 estudios que abarcaban un total de 815 pacientes: 252 pertenecieron al grupo de URS-F y 563 al de NLP. Cuatro fueron retrospectivos y uno fue prospectivo no aleatorizado.
ResultadosLa tasa libre de litiasis osciló entre el 47,0 y el 95,0% para la URS-F y entre el 87,0 y el 100% para la NLP. La tasa de complicaciones fue del 8,8-29,0% en la URS-F y del 11,9-27,0% en la NLP. La URS-F requirió un número mayor de procedimientos y tuvo un menor descenso de hemoglobina y ascenso de creatinina en comparación con la NLP.
ConclusionesLa tasa libre de litiasis fue mayor en la NLP, aunque la URS-F podría alcanzar unos resultados comparables a expensas de realizar varios procedimientos. Ambas técnicas tienen una frecuencia de complicaciones similar, pero con más alteraciones analíticas posquirúrgicas en el grupo de NLP.
The size of the renal stone is one of the main factors that influence the choice of treatment to be performed in patients with renal lithiasis.
According to many international guidelines, percutaneous nephrolithotomy (PNL) is the first-choice treatment for stones greater than 2cm,1 leaving the retrograde approach (flexible ureteroscopy (FURS)), as the second option. This is due to the high success rate of PNL in large lithiasis treatment.2 However, this technique is not free of complications,3 and sometimes it cannot be performed due to the patient's characteristics (e.g. obesity, haemorrhagic diathesis, presence of renal tumour).
In this context, the technological advances of FURS, regarding the flexible device and the fragmentation technique, could increase the success of the retrograde approach.4 This fact has prompted research on the efficacy of non-percutaneous techniques in calculi greater than 2cm, reaching a stone-free rate of 91.0–93.0%.5,6 These figures could be even higher in lithiasis of intermediate size, between 2 and 3cm, reaching up to 95.0%.6 This is why the European Association of Urology (EAU) guidelines present the FURS as an equivalent alternative to the PNL in experienced centre.12
The objective of the present systematic review is to compare the results of PNL and FURS in the treatment of 2–3cm renal stones, in terms of lithiasis-free rate, complications and the requirement of second procedures.
Material and methodsWith PRISMA systematic review guidelines, we investigated on Medline (PubMed), Trip database, Embase, Web of Science, Cochrane and Scopus databases using the following terms: ureteroscope, retrograde flexible nephrolithotripsy, ureteroscopy, ureterorenoscopy, RIRS, retrograde intrarenal surgery, retrograde flexible, flexible nephrolithotomy, PCNL and percutaneous lithotripsy.
Two independent investigators selected clinical trials, meta-analyses, cohort studies and series of cases in Spanish and English that compared PNL (standard and mini-percutaneous) with FURS, for the treatment of single or multiple renal stones with sizes ranging from 2 to 3cm.
The studies including stones greater than 3cm or smaller than 2cm, animal testing, combined therapies, treatments including extracorporeal lithotripsy (ESWL) and/or paediatric population were excluded from our research.
The flow diagram of the article selection is shown in Fig. 1.
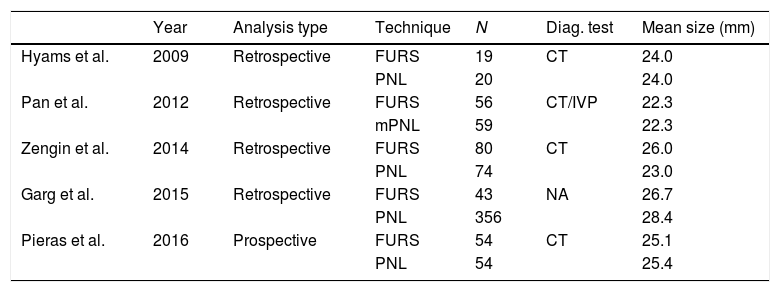
Summary of evidence5 studies were included in the systematic review. Their global characteristics are summarised in Table 1. A total of 815 patients were included. 252 (30.9%) belonged to the FURS group and 563 (69.1%) to the PNL group. Regarding their methodology, all of them were cohort studies; 47–10 were retrospective and one11 was prospective nonrandomized. A meta-analysis was not performed due to the low number of studies and the heterogeneity of the results.
Characteristics of the studies included in the systematic review.
| Year | Analysis type | Technique | N | Diag. test | Mean size (mm) | |
|---|---|---|---|---|---|---|
| Hyams et al. | 2009 | Retrospective | FURS | 19 | CT | 24.0 |
| PNL | 20 | 24.0 | ||||
| Pan et al. | 2012 | Retrospective | FURS | 56 | CT/IVP | 22.3 |
| mPNL | 59 | 22.3 | ||||
| Zengin et al. | 2014 | Retrospective | FURS | 80 | CT | 26.0 |
| PNL | 74 | 23.0 | ||||
| Garg et al. | 2015 | Retrospective | FURS | 43 | NA | 26.7 |
| PNL | 356 | 28.4 | ||||
| Pieras et al. | 2016 | Prospective | FURS | 54 | CT | 25.1 |
| PNL | 54 | 25.4 |
Diag. test: lithiasis measurement and diagnostic and technique.
NA: not available; PNL: percutaneous nephrolithotomy; FURS: flexible ureteroscopy.
The FURS was performed with different flexible devices (Olympus P3 and P5 or Storz Flex X-2). All cases use the holmium laser for fragmentation and postoperative placement of double-J stent. An access sheath was used in all patients8,9,11 in 3 studies. It was used only in some cases7 in one study, and the group by Garg et al. does not make any reference to the use of it.
Regarding PNL, it was performed in the prone position in 4 studies7–10and in the Valdivia position in one.11 Four studies7,9,10 used a 26–24 Fr nephroscope, one used a 14 Fr8 nephroscope, and another study10 does not specify its size. The dilation methods were: Amplatz in 2 studies,8,9 the balloon in one,7 another study alternated balloon and/or Alken dilators11 whereas the last work10 does not mention the performed technique. Regarding the fragmentation instruments: 2 used lasers,8,10 Zengin et al. used a pneumatic system, Pieras et al. ultrasound, while Hyams et al. employed various techniques (laser, pneumatics and ultrasound).
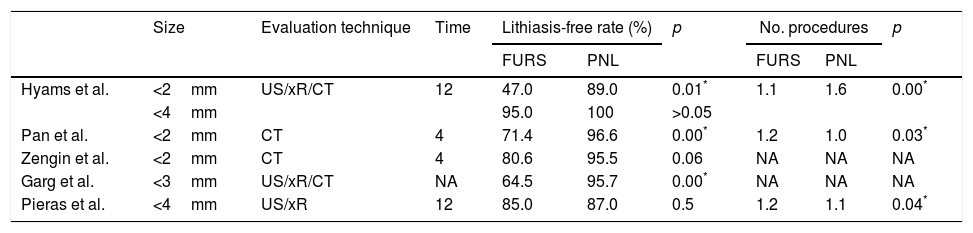
The lithiasis-free rate of FURS ranged between 47.0 and 95.0%, and between 87.0 and 100% for PNL. This lithiasis-free rate was evaluated in different ways. 2 studies8,9 performed a CT one month after surgery, with a limit of 2mm to determine the existence of significant remains. The remaining works performed several imaging tests (ultrasound, xR or CT) using different limits of significant size. In 3 studies8–10 statistically significant differences were found regarding lithiasis-free rate in favour of PNL. 3 studies,8,9,11 analysed the number of procedures performed, and only the work of Hyams et al. obtained a greater number of interventions in the PNL group, as shown in Table 2.
Evaluation of the lithiasis-free rate and number of procedures performed.
| Size | Evaluation technique | Time | Lithiasis-free rate (%) | p | No. procedures | p | |||
|---|---|---|---|---|---|---|---|---|---|
| FURS | PNL | FURS | PNL | ||||||
| Hyams et al. | <2mm | US/xR/CT | 12 | 47.0 | 89.0 | 0.01* | 1.1 | 1.6 | 0.00* |
| <4mm | 95.0 | 100 | >0.05 | ||||||
| Pan et al. | <2mm | CT | 4 | 71.4 | 96.6 | 0.00* | 1.2 | 1.0 | 0.03* |
| Zengin et al. | <2mm | CT | 4 | 80.6 | 95.5 | 0.06 | NA | NA | NA |
| Garg et al. | <3mm | US/xR/CT | NA | 64.5 | 95.7 | 0.00* | NA | NA | NA |
| Pieras et al. | <4mm | US/xR | 12 | 85.0 | 87.0 | 0.5 | 1.2 | 1.1 | 0.04* |
Time: time (weeks) from surgery to control test.
NA: not available; PNL: percutaneous nephrolithotomy; xR: simple abdominal X-ray; FURS: flexible ureteroscopy.
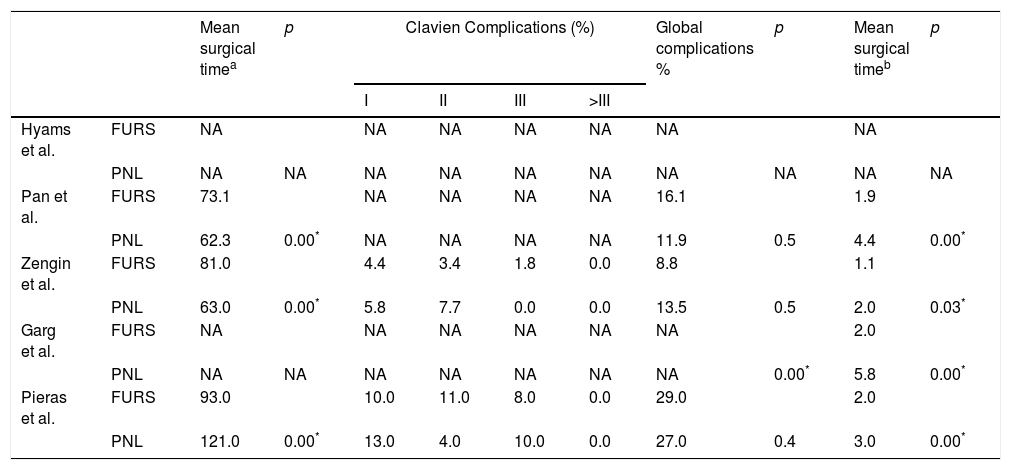
Four studies8–11 collected the complication rate, but only 229,11 classified them according to the Clavien scale. In the FURS group, complications were mainly due to infections, while in the PNL group, it was bleeding and blood transfusion requirement. No Clavien grade IV or V complication was documented. Only one study10 found statistically significant differences in the overall complication rate, but the rates of each group are not mentioned separately. 3 papers8,9,11 compared intervention time, but only one of them11 specifies how the measurement was performed: from cystoscopy to double-J placement for FURS, and from cystoscopy to the placement of the nephrostomy tube for the PNL. 2 studies obtained greater surgical time rates in the FURS and only the work of Pieras et al. obtained a longer average duration in the PNL group, as shown in Table 3. Four studies8–11 analysed the mean length of in- hospital stay, being in all of them greater for PNL, as shown in Table 3.
Surgical time, complications and length of in-hospital stay.
| Mean surgical timea | p | Clavien Complications (%) | Global complications % | p | Mean surgical timeb | p | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | >III | ||||||||
| Hyams et al. | FURS | NA | NA | NA | NA | NA | NA | NA | |||
| PNL | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| Pan et al. | FURS | 73.1 | NA | NA | NA | NA | 16.1 | 1.9 | |||
| PNL | 62.3 | 0.00* | NA | NA | NA | NA | 11.9 | 0.5 | 4.4 | 0.00* | |
| Zengin et al. | FURS | 81.0 | 4.4 | 3.4 | 1.8 | 0.0 | 8.8 | 1.1 | |||
| PNL | 63.0 | 0.00* | 5.8 | 7.7 | 0.0 | 0.0 | 13.5 | 0.5 | 2.0 | 0.03* | |
| Garg et al. | FURS | NA | NA | NA | NA | NA | NA | 2.0 | |||
| PNL | NA | NA | NA | NA | NA | NA | NA | 0.00* | 5.8 | 0.00* | |
| Pieras et al. | FURS | 93.0 | 10.0 | 11.0 | 8.0 | 0.0 | 29.0 | 2.0 | |||
| PNL | 121.0 | 0.00* | 13.0 | 4.0 | 10.0 | 0.0 | 27.0 | 0.4 | 3.0 | 0.00* | |
NA: not available; PNL: percutaneous nephrolithotomy; FURS: flexible ureteroscopy.
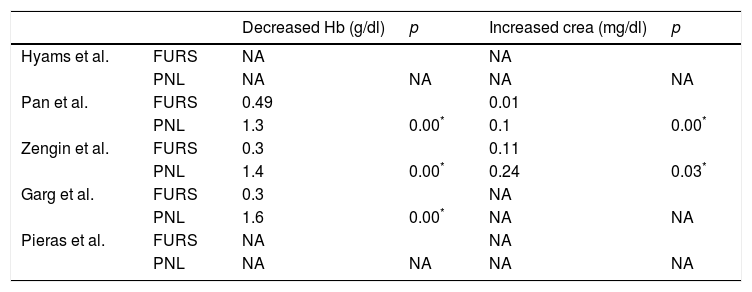
Regarding the analytical variations before and after the intervention, 3 studies analysed differences in haemoglobin8–10 and 2 of them8,9 in creatinine. In all the analyses performed, the decrease in haemoglobin and the increase in creatinine were more severe in the PNL group than in the FURS group. All these differences were statistically significant, as shown in Table 4.
Analytic variations.
| Decreased Hb (g/dl) | p | Increased crea (mg/dl) | p | ||
|---|---|---|---|---|---|
| Hyams et al. | FURS | NA | NA | ||
| PNL | NA | NA | NA | NA | |
| Pan et al. | FURS | 0.49 | 0.01 | ||
| PNL | 1.3 | 0.00* | 0.1 | 0.00* | |
| Zengin et al. | FURS | 0.3 | 0.11 | ||
| PNL | 1.4 | 0.00* | 0.24 | 0.03* | |
| Garg et al. | FURS | 0.3 | NA | ||
| PNL | 1.6 | 0.00* | NA | NA | |
| Pieras et al. | FURS | NA | NA | ||
| PNL | NA | NA | NA | NA |
NA: not available; PNL: percutaneous nephrolithotomy; FURS: flexible ureteroscopy.
To our knowledge, this is the first review that compares PNL and FURS for the treatment of lithiasis with sizes between 2 and 3cm. The results obtained in terms of lithiasis-free rate support what is included in the clinical guidelines. However, there are several details to clarify before reaching conclusions.
The first thing to note is the heterogeneity of the lithotriptic materials and techniques presented in the collected studies. This could influence the results of the different techniques and is a limitation of the analysis.
Regarding the lithiasis-free rate, 3 studies managed to reach statistical significance in favour of the PNL, but it was not significant in the rest: Pan et al., Garg et al. and Hymans et al.
Another relevant aspect to analyse, is the difference between methods and the values to confirm the success or failure of each treatment. In this aspect there is no consensus on the minimum size of a fragment to be considered relevant, or on the right time (after the procedure) to perform its evaluation. Only 2 studies had a similar assessment system: CT scan one month after surgery8,9 and PNL had a significantly higher lithiasis-free rate.9 This variability could lead to underestimate the success of the surgery.
We must add that the number of procedures was mostly higher in the FURS groups. Only Hyams et al. found a greater number of interventions in the PNL group. According to the authors, patients were treated with this technique aiming to obtain the smallest size of lithiasic remains possible. This would justify this result.
Studies that only include the FURS for this size range14 have shown a high stone-free rate of up to 83% for lithiasic remains smaller than 4mm at the expense of performing several treatments, with 1.2 interventions per patient. Other works have compared similar size intervals,13 from 2 to 4cm, observing a higher free-lithiasis rate with PNL with only one treatment: 73.5% for FURS and 91.2% for PNL. This rate tends to balance with a second treatment, reaching 94.1% for FURS after 3 months.
For lithiasis greater than 2cm, the group of Zheng et al. performed a meta-analysis and did not find differences between the lithiasis-free rate among both techniques. Other later studies did find differences in favour of the percutaneous technique16 when comparing FURS with the mini-PNL, but regarding another range of lithiasis size.
There were problems regarding surgical time. Pieras et al.11 is the only group that specifies how time was evaluated. They found shorter time in the FURS. However, the other 2 studies that measured surgical time8,9 had lower results in PNL. This contradiction in the results is not new. Some reviews have obtained shorter times for PNL,15 and some have not found differences at all between techniques.13,14
Complications were collected in 4 studies, 2 of them9,11 with the Clavien system. There were no Clavien complications grade IV or higher, and only one study10 found significant differences, with a higher number of complications in the PNL group. The major complications reported in PNL3 are not present in these studies, and complications of Clavien grade III have not been reported. In turn, as demonstrated by the group16 of Davis et al., there does not seem to be a greater number of complications in the PNL groups compared to those of FURS.
Nonetheless, there is no consensus regarding complications. The group of Zheng et al.15 found a higher bleeding rate in patients treated under NLP.
In other aspects, the collected studies seem to agree. One point to highlight is that both, the decrease in haemoglobin and the increase in postoperative creatinine, were more severe in the PNL group. Another relevant element to consider is length of in-hospital stay, shorter in patients operated with FURS. Although these data are not directly related to complications, they suggest techniques should be adjusted to the needs of each patient; e.g. patients with an increased risk of bleeding, in whom the FURS has shown a safe profile.17
It is also relevant to mention that, while the material evolution of FURS could suppose a greater success in the management of large stones,4,5 the technical improvements of PNL are focused on the reduction of complications. A lower calibre in the material used18 and the possible removal of the nephrostomy tube after surgery19 are two aspects that are being explored to optimise the disadvantages of PNL. This constant renewal of surgical standards requires an updated study of both techniques including their advantages and disadvantages.
Regarding the limitations of this study, the retrospective nature of most of the studies and the absence of randomisation in them are inconveniences of this analysis. In addition, the great differences when evaluating residual fragments make it difficult to analyse common results of each technique. Finally, the absence of recent comparative articles does not allow us to verify if the improvements of the modern systems are gaining better results.
ConclusionsPNL achieves a higher lithiasis-free rate than the one accomplished by FURS in 2–3cm stones. However, FURS is a method that could obtain similar lithiasis-free rate at the expense of performing more than one treatment. Both techniques appear to have comparable profiles regarding complications, but patients undergoing PNL have greater haemoglobin and creatinine alterations and require longer periods of in-hospital stay. Randomised studies are necessary to evaluate both techniques and perform an appropriate direct comparison.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández Alcalde ÁA, Ruiz Hernández M, Gómez dos Santos V, Sánchez Guerrero C, Diaz Pérez DE, Arias Fúnez F, et al. Comparación entre nefrolitotomía percutánea y ureteroscopia flexible para el tratamiento de litiasis renales de entre 2 y 3cm. Actas Urol Esp. 2019;43:111–117.