Medical education has a major social impact because it ultimately influences the quality and safety of the health service offered to the population. Several studies have acknowledged the relationship between medical knowledge on transfusion medicine and the proper use of this therapy. The rational use of blood has become a worldwide concern. In this context, the aim of the present study was to evaluate medical residents’ knowledge on transfusion medicine in hospitals located in Rio de Janeiro, Brazil, and their training during their medical education.
MethodsOne hundred and six residents from eight medical specialties of four hospitals participated. A questionnaire developed by the Biomedical Excellence for Safer Transfusion (BEST) group was applied to evaluate the participants’ medical knowledge. Another questionnaire was also applied to evaluate participant profiles regarding frequency of transfusion prescriptions, self-perceived knowledge and relevance of the subject.
ResultsThe mean number of correct answers to the questionnaire on knowledge about transfusion practices was 43.5% (range: 15–80%). A relationship between training during medical residency and the obtained result was observed (p-value=0.0007). Most residents (73%) did not receive training in transfusion medicine during their graduation or residency and 93% would like to receive additional training.
ConclusionA clear deficit in the knowledge of transfusion medicine was verified, indicating the need for change in the teaching of this specialty. This result is similar to some developed countries.
Transfusion of blood components is one of the most common medical procedures in the world.1,2 In Brazil, about 3,000,000 transfusions are performed annually.3 Transfusion therapy is capable of saving lives, but, if misused, it may expose recipients to unnecessary risks,2,4,5 generate costs for the health system and waste a scarce resource.6 Concern over the rational use of blood has increased in recent years, and approaches such as Patient Blood Management, which proposes that transfusion medicine practice should be evidence-based, have gained strength in the clinical practice.7,8
Medical education has a social impact because it ultimately influences the quality and safety of the health service offered to the population. Brazil currently has 299 medical schools registered in the Ministry of Education's e-MEC online platform (http://emec.mec.gov.br/)9 and is the second in the rank of the number of medical schools in the world. Therefore, the quality of teaching offered in these schools is a concern. Added to this is the fact that transfusion medicine, even after the advent of AIDS in the 1980s, has not been privileged in the curricula of medical schools in Brazil or in the world. So, there are still important gaps in physician training regarding knowledge of transfusion medicine, which interferes with proper medical practices and may compromise patient safety.10 In teaching hospitals, most transfusions are indicated by resident physicians6; this accentuates concern regarding their knowledge on the subject. Numerous studies in different countries around the world have shown insufficient knowledge of newly graduated physicians on transfusion medicine and the need to expand and improve the teaching of transfusion medicine at graduate and postgraduate levels.11–13
In Brazil, most physicians do not receive training in transfusion medicine at the undergraduate level or during medical residency.14 An assessment of medical knowledge in transfusion medicine is, therefore, necessary in order to identify major gaps in knowledge and propose strategies to reduce them. In this context, the aim of the present study was to evaluate the knowledge of resident physicians in teaching hospitals in Rio de Janeiro about transfusion medicine and the existence or non-existence of previous training concerning this issue.
MethodsA total of 106 resident physicians from eight specialties and with a specialization degree for differing numbers of years were interviewed. These physicians worked in four public hospitals in the city of Rio de Janeiro that act as teaching hospitals, including a university hospital, an emergency hospital, a cancer treatment center and a maternity. The number of participants from each specialty varied according to the number of places offered in the respective medical residency programs.
The applied research protocol was approved by the Oswaldo Cruz Institute – FIOCRUZ – Ethics Committee (CAAE 46175015.4.0000.5248) and all participants signed an informed consent form.
A questionnaire, developed by members of the Biomedical Excellence for Safer Transfusion (BEST) Collaborative Group in conjunction with the American Society of Clinical Pathology (ASCP), was used to evaluate medical knowledge regarding transfusion medicine. The development and validation of the instrument were described in a previous publication.15 The authors of the BEST group used the modified Delphi method, which is a structured approach to reach consensus among experts. The specialists who participated in the construction of this questionnaire came from ten different countries. To define which questions would be part of the final questionnaire, the Rasch analysis model was used and statistical analyses were performed. According to this international group of experts, the instrument includes priority knowledge and skills in transfusion medicine for non-specialist physicians. The questionnaire consists of 20 multiple-choice questions with a unique correct answer for each. Authorization was obtained from the main author of the article to use this evaluation instrument and followed his instructions regarding the questionnaire application and the non-disclosure of copies of the questionnaires and answers. The questionnaire was translated into Portuguese and the translation was submitted to a back translation (Portuguese to English). The original English version and the back translation were compared and a final version in Portuguese was attained. This was applied in a pilot study conducted with seven hematology and hemotherapy specialists and six internal medicine specialists, in order to evaluate the clarity and understanding of the questions.
A survey was also carried out regarding the socio-professional profile of the participants, whether they had received previous training in transfusion medicine at the undergraduate level or during their medical residency, where they worked and the frequency of transfusion prescriptions. The perception of their knowledge on transfusion medicine, the importance of the issue in their practice, and the usefulness of additional training were verified through a five-point Likert scale. The questionnaires were applied from April 2016 to April 2017.
Statistical analysesDescriptive statistics such as means and percentages were used to describe the profile of the participating medical residents, their performance in the evaluation questionnaire and their self-perception of knowledge on transfusion medicine.
In order to compare the different specialty groups and groups with or without training in transfusion medicine, as well as those with a higher self-perception of knowledge, the first step was to verify sample normality by the D’Agostino Pearson test. A Gaussian distribution was observed on comparing the performance of hematology residents to the other participants. Thus, a parametric test was used. When the data did not follow this distribution, a suitable non-parametric test was used. Graphs were plotted and tests were performed using the Graph Pad PRISM 5 software package (San Diego, California, USA) at a significance level of 5% (p-value <0.05).
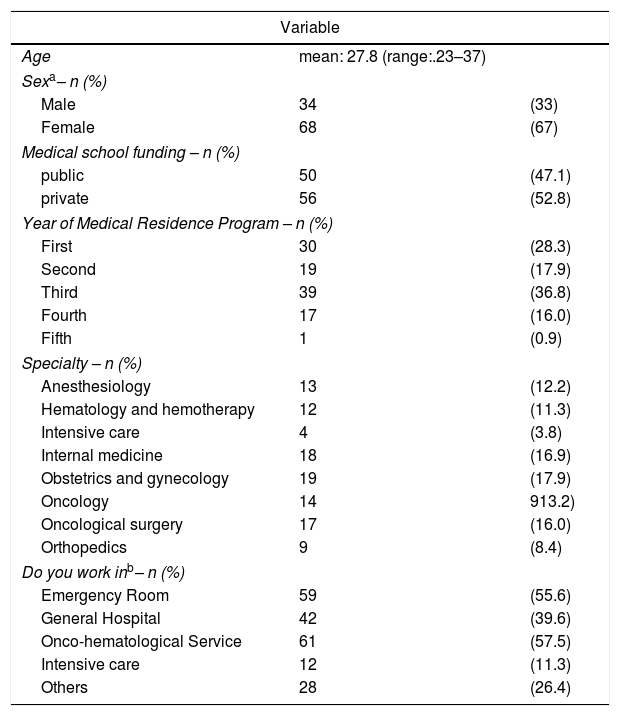
ResultsParticipant profiles are displayed in Table 1. An elevated number of resident physicians participating in the study work in services that routinely use a high amount of blood components, such as emergency, onco-hematology and intensive care units.
Participant profiles.
| Variable | ||
|---|---|---|
| Age | mean: 27.8 (range:.23–37) | |
| Sexa– n (%) | ||
| Male | 34 | (33) |
| Female | 68 | (67) |
| Medical school funding – n (%) | ||
| public | 50 | (47.1) |
| private | 56 | (52.8) |
| Year of Medical Residence Program – n (%) | ||
| First | 30 | (28.3) |
| Second | 19 | (17.9) |
| Third | 39 | (36.8) |
| Fourth | 17 | (16.0) |
| Fifth | 1 | (0.9) |
| Specialty – n (%) | ||
| Anesthesiology | 13 | (12.2) |
| Hematology and hemotherapy | 12 | (11.3) |
| Intensive care | 4 | (3.8) |
| Internal medicine | 18 | (16.9) |
| Obstetrics and gynecology | 19 | (17.9) |
| Oncology | 14 | 913.2) |
| Oncological surgery | 17 | (16.0) |
| Orthopedics | 9 | (8.4) |
| Do you work inb– n (%) | ||
| Emergency Room | 59 | (55.6) |
| General Hospital | 42 | (39.6) |
| Onco-hematological Service | 61 | (57.5) |
| Intensive care | 12 | (11.3) |
| Others | 28 | (26.4) |
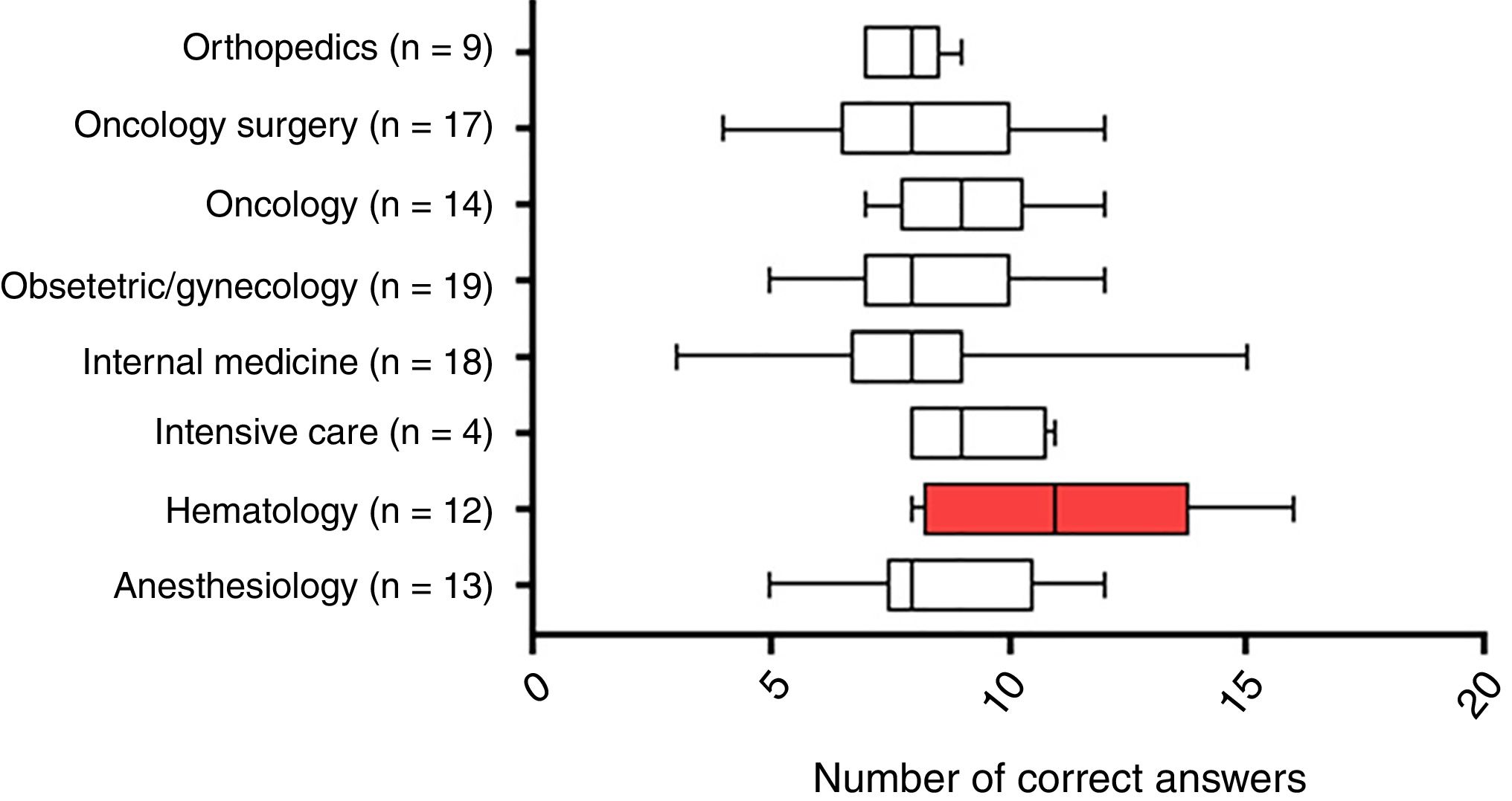
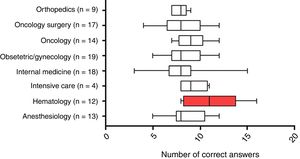
The mean number of correct answers to the questionnaire was 43.5% (range: 15–80%). No significant differences were found between the different specialties, except for the hematology and hemotherapy specialty, which obtained a higher average score than the rest of the group, with means of 56% correct answers (p-value=0.0047; CI: −4.676 to −1.059, Welch's test) (Figure 1).
Number of correct answers by specialty. Box plot indicating the number of correct answers by specialty with the respective number of participants. There was a significant difference (p-value <0.005) between the group marked in red when compared to the other specialties (One-Way ANOVA and Tukey's post-test).
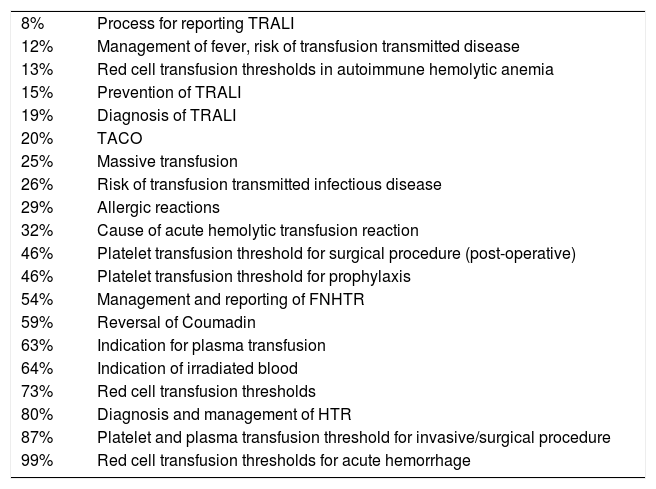
The questions with the highest percentages of correct answers were those related to the prescription of blood components (99% for packed red blood cells and 87% for platelets) and diagnosis of hemolytic transfusion reactions (HTR – 80%). The lowest percentages of correct answers were obtained for questions about transfusion-related acute lung injury (TRALI – 15%), the process for reporting TRALI (8%) and management of transfusion reaction, such as febrile reactions (12%) and transfusion-associated circulatory overload (TACO – 20%). The indication of transfusions in patients diagnosed with autoimmune hemolytic anemia also presented a small percentage of correct answers. (Table 2)
Correct questionnaire answers by subject.
| 8% | Process for reporting TRALI |
| 12% | Management of fever, risk of transfusion transmitted disease |
| 13% | Red cell transfusion thresholds in autoimmune hemolytic anemia |
| 15% | Prevention of TRALI |
| 19% | Diagnosis of TRALI |
| 20% | TACO |
| 25% | Massive transfusion |
| 26% | Risk of transfusion transmitted infectious disease |
| 29% | Allergic reactions |
| 32% | Cause of acute hemolytic transfusion reaction |
| 46% | Platelet transfusion threshold for surgical procedure (post-operative) |
| 46% | Platelet transfusion threshold for prophylaxis |
| 54% | Management and reporting of FNHTR |
| 59% | Reversal of Coumadin |
| 63% | Indication for plasma transfusion |
| 64% | Indication of irradiated blood |
| 73% | Red cell transfusion thresholds |
| 80% | Diagnosis and management of HTR |
| 87% | Platelet and plasma transfusion threshold for invasive/surgical procedure |
| 99% | Red cell transfusion thresholds for acute hemorrhage |
TRALI: Transfusion-related acute lung injury; TACO: Transfusion-associated circulatory overload; FNHTR: Febrile non-hemolytic transfusion reactions; HTR: Hemolytic transfusion reactions.
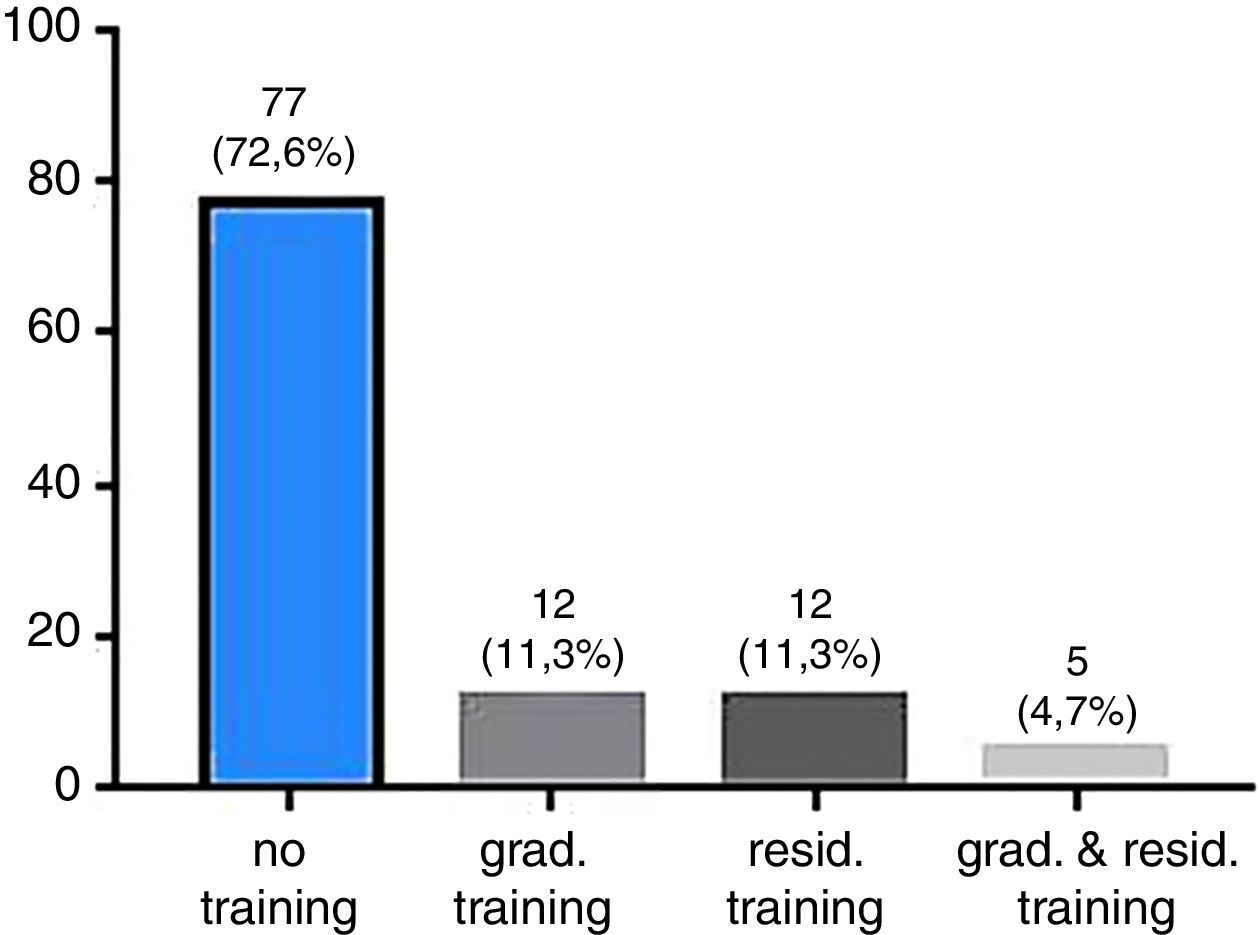
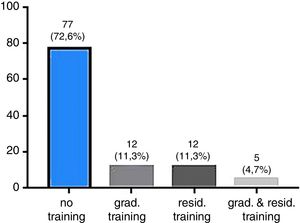
Only 12 (11%) of the participating physicians reported receiving transfusion medicine training during their graduations, while another 12 (11%) reported receiving training during their medical residency. A small group of five participants (4.71%) received both undergraduate and residency training (Figure 2). The score obtained by the participants who received training during their medical residency was higher than the other groups (Mann–Whitney test; p-value=0.0007). It is important to note that most of these participants belong to the hematology and hemotherapy specialty. No statistical difference between participants who received undergraduate training and the other participants was observed (Mann–Whitney test; p-value=0.1858).
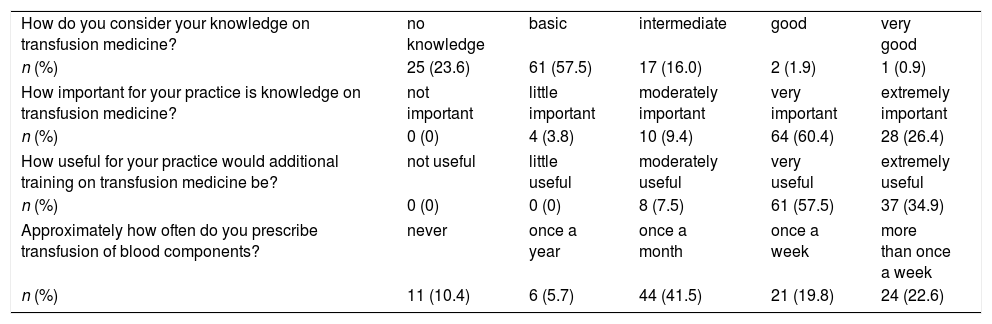
The results regarding participant self-perception knowledge on transfusion medicine and frequency of blood transfusion prescriptions are shown in Table 3. Only three participants (2.8%) considered their knowledge as good or very good. No statistically significant difference was observed between the means of this group compared to the other participants. Most participants considered their knowledge basic (57.5%).
Consciousness on transfusion medicine among residents.
| How do you consider your knowledge on transfusion medicine? | no knowledge | basic | intermediate | good | very good |
| n (%) | 25 (23.6) | 61 (57.5) | 17 (16.0) | 2 (1.9) | 1 (0.9) |
| How important for your practice is knowledge on transfusion medicine? | not important | little important | moderately important | very important | extremely important |
| n (%) | 0 (0) | 4 (3.8) | 10 (9.4) | 64 (60.4) | 28 (26.4) |
| How useful for your practice would additional training on transfusion medicine be? | not useful | little useful | moderately useful | very useful | extremely useful |
| n (%) | 0 (0) | 0 (0) | 8 (7.5) | 61 (57.5) | 37 (34.9) |
| Approximately how often do you prescribe transfusion of blood components? | never | once a year | once a month | once a week | more than once a week |
| n (%) | 11 (10.4) | 6 (5.7) | 44 (41.5) | 21 (19.8) | 24 (22.6) |
Eighty-six percent of the participants considered transfusion medicine to be very important or extremely important to their clinical practice and over 90% said they would find additional training on the subject very useful or extremely useful.
DiscussionThe results obtained in the present study are similar to the results observed by Haspel et al.13 using the same instrument to evaluate knowledge on transfusion medicine of resident physicians in Australia, Canada, England, Ireland, Italy, Germany, the Netherlands, Spain and the United States. The mean of correct answers of this study (43.5%) is similar to the mean observed by those authors (45.7%). This score was considered basic knowledge with less than 50% of correct answers.13 The same questionnaire was also applied to resident physicians at the University of Toronto, who obtained an average of 50±18%.16 It is noteworthy that the study by Haspel et al.13 enrolled only residents in internal medicine training before they entered another specialty, unlike the present study, that included residents from different specialties. Thus, most of the participants had already completed the prerequisites, for example, the cancer surgery residents must have attended the general surgery residency program and clinical oncology residents must have attended the residency in internal medicine. Thus, even physicians already attending their second residence program obtained a low average of correct answers, corroborating previous studies that indicate that the level of knowledge regarding transfusion medicine does not correspond to the post-graduation level.12,17
In Brazil, hematology and transfusion medicine constitutes a single specialty named hematology and hemotherapy. In this specialty, transfusion medicine accounts for about 30% of the two-year program.14 Residents belonging to this specialty obtained a mean of 56% in the questionnaire (range: 40–80%), significantly higher than the other residents (p-value=0.0047). However, this mean was low when compared to a study performed by Lin et al. published in 2016 that applied the same instrument to hematology residents (61.6%).18 In a study carried out in Canada, the average accuracy of hematology residents was also higher than that of other specialties.16 In another study using a different evaluation instrument, Graham also observed a significant difference in the evaluation of hematology residents when compared to residents from the first two years. However, in this case the scores obtained by hematology residents were higher than 80%.12 The score obtained by hematology residents in the present study, even though superior to the other specialties, is still considered basic. This is very worrisome; if we consider that these residents are habitual prescribers of blood components and the important aspects of onco-hematological disease therapy depend on transfusion support.
The main deficiency observed in this study was concerned with transfusion-related acute lung injury (TRALI) and the management of transfusion reactions; results similar to those obtained in previous studies.6,11,13,18 These data deserve attention since the correct diagnosis of this type of reaction, differentiating it from other reactions such as TACO, for example, and its proper management and reporting are very important, as these are events that may result in high morbidity rates, including death.5
It is important to note that a very small percentage of the participating physicians had undergraduate training (17%). This result is consistent with a previous survey that indicated that only 27% of Brazilian medical schools mentioned the content or offered the subject of transfusion medicine or hematology in their curricula available online.19
The same percentage (17%) of participants reported having been trained in the subject during their medical residency program. In contrast to previous studies, a significant difference was not observed between participants who received undergraduate training and those who did not.6,13 This difference was observed only for those who received training during their residence program, which mainly corresponded to hematology and hemotherapy residents. Only five participants who did not belong to the hematology and hemotherapy specialty were trained in transfusion medicine during their medical residency. In most of the published studies from other countries where knowledge of resident physicians on transfusion medicine was assessed, the percentage of participants who received some degree of transfusion medicine training, even though it may have been considered insufficient, was much higher than in the present study.11,20 Only one result similar to the results of this study was observed; a study conducted with 85 participants in a tertiary hospital in India, where the percentage of residents who reported receiving transfusion medicine training at the graduate level was of 15.3%.21 In the study conducted by O’Brien et al. with 116 first-year residents in Washington, USA, 58.6% of the interviewed residents had received some degree of training in transfusion medicine.11 In a study conducted in Iran in 2011, 69.7% of 135 first-year residents reported receiving undergraduate transfusion medicine training.20 In the study by Haspel et al., that included residents of nine countries, namely Australia, Canada, England, Italy, Germany, the Netherlands, Ireland, Spain and the United States, 87.9% of the participants declared to have received some training during their residence program, even though the majority of the training only comprised lectures of between one and two hours.13 In a study conducted in Canada with 192 obstetricians 71 of whom were trainees, 58% of the trainees received formal transfusion instruction in their post-graduate training.21 In another study conducted in England with 787 residents, 70% of the participating resident physicians reported receiving training in transfusion medicine during graduation.12 Karp et al., in a survey conducted in US universities, found that 83% of the 86 medical schools that participated in the study offered at least a one-hour lecture on the subject, while only 17% reported having no classes on transfusion medicine in their curricula.23
The path to the rational and adequate use of blood components with evidence-based transfusion indications, such as Patient Blood Management and safer transfusion practices for patients, must necessarily pass through training with improved medical knowledge of transfusion medicine.7 Friedman states that the main obstacle to the use of these practices and alignment with available guidelines is the lack of medical knowledge and the fact that there will be little impact on how transfusions are performed as long as there is such a gap in medical education.10 Studies in several countries,12,13,21 including Brazil,14,24 have already pointed out the need for additional training in transfusion medicine as a way to improve medical transfusion practices. Considering evidence-based education, this subject should be taught in a structured way, with a minimum number of hours allowing the subject to be taught with clear learning objectives in order to develop a clinical skill in the student and with adequate evaluations.25 It is also necessary to discuss the use of different teaching methods, such as e-learning and case simulations, that may be useful tools to achieve these goals.26–28
In Brazil, no reports in the literature are available concerning the evaluation of knowledge of resident physicians with a validated instrument that could guide the planning of educational actions in the area, whether at the graduation level, during medical residency or as a manner of ongoing education. According to Lin and Haspel, the development of a curriculum for transfusion medicine requires problem identification and assessments.28 Although the present study has as a limitation that the participants came from four teaching hospitals in a single municipality, it brings forth data on the knowledge of transfusion medicine of resident doctors in agreement with international studies and can aid in the formulation of educational strategies. Another limitation of this study was the lack of information on the number of hours of transfusion medicine training, since previous studies have shown that the number of hours is related to the physicians’ knowledge level.6,13 However, it is noteworthy that most participants did not receive any type of training, thus still indicating the need for more training.
Regarding self-perception knowledge, the majority of the interviewees considered that they did not possess knowledge or only basic knowledge on the subject. Similar results were obtained in the studies performed by Haspel et al. and O’Brien et al.,11,13 in which more than 90% of participants felt that additional training would be very useful for their medical practice. This has been repeated in several different studies.13,18,21,22 Lin and Haspel suggest that the last years of graduation and the first years of medical residency would be ideal targets for training in transfusion medicine.28 Previous studies have indicated that training in this subject received in the previous five years had repercussions on the results of the evaluation, and also that the greater the time after training the worse the results obtained by physicians in the evaluation.6 So, continuous education in transfusion medicine is an important point for the implementation of a more adequate and safe transfusion practice for patients. It is noteworthy that 42.4% of the participants reported that they prescribe transfusions at least once a week and, when adding this value to those who report that they prescribe once a month, this percentage reaches 83.9%. In other words, most participating physicians, while acknowledging their insufficient knowledge in transfusion medicine, frequently prescribe this therapy, which may favor the excessive and inappropriate use of blood components and expose patients to reaction risks that many of these physicians do not know how to handle.
ConclusionsThis study demonstrated that most participants had no training in transfusion medicine at the undergraduate or postgraduate level. This also brings forth a concern that the level of knowledge in transfusion medicine assessed through a validated instrument was considered only basic, similar to results from international studies. That is, the deficiency in the knowledge about transfusion medicine pointed out in this study crosses several countries with different socioeconomic situations. The need to revise the curricula or teaching modalities used is necessary to minimize the risks of inadequate transfusion practice.
Discussion regarding the inclusion of this matter in Brazilian medical graduation, as well as at a post-graduation level, is urgent, since a very small percentage of medical schools offer training in transfusion medicine. Even in countries where this is already in place, studies have demonstrated the need to improve and expand the teaching of this specialty with the aim of improving transfusion practice. As Brazil is a country of continental dimensions, future studies regarding assessments of knowledge, also including the evaluation of transfusion practices in other centers, may be useful to indicate changes in medical education aiming at improvements in the current scenario.
Author contributionsMV and LA participated in the formulation and design of the study hypothesis. MV collected the data. MV and LA contributed to the data analysis and the drafting of the initial manuscript. All authors approved the final manuscript for submission.
Data sharingThe datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
FundingFundação de Amparo à Pesquisa do Estado do Rio de Janeiro – FAPERJ, Instituto Oswaldo Cruz and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
Conflicts of interestThe authors declare no conflicts of interest.
The authors thank Dr. Richard Haspel for allowing the use of questionnaire. The authors also wish to thank Roberto Lannes, Roberto Esporcatte, Luis Felipe R. Pinto, Ana Elisa Baião, Fabio Russomano and all the professionals that somehow made the accomplishment of this study possible. The authors also thank the residents who participated in this study.