Cryptococcosis is one of the most frequent and severe AIDS defining illnesses.
AimsWe present a patient with advanced HIV/AIDS disease and a diffuse meningoencephalitis due to Cryptococcus neoformans. The patient developed an acute and bilateral blindness associated with high cerebrospinal fluid pressure and optic neuropathy.
MethodsPost-mortem anatomopathologic study revealed a high number of Cryptococcus in the central nervous system, including the optic nerves and the optic chiasm.
ConclusionThe patient's sudden visual loss appeared to be related to the perineuritic arachnoiditis and the massive invasion of the optic nerves by the fungus.
La criptococosis es una de las más frecuentes y graves enfermedades marcadoras del sida.
ObjetivosSe describe el caso de un paciente con enfermedad VIH/sida avanzada y meningoencefalitis por Cryptococcus neoformans que presentó un cuadro de amaurosis bilateral aguda asociada con aumento de la presión intracraniana y neuropatía óptica.
MétodosEl paciente evolucionó de manera desfavorable, falleció y en la necropsia se observaron un gran número de levaduras compatibles con Cryptococcus que infiltraban las meninges, la vía óptica y el quiasma.
Conclusiónla amaurosis fue el resultado de la arachnoiditis perineurítica y de la infiltración y necrosis del nervio y quiasma óptico por levaduras de Cryptococcus.
Cryptococcosis is the most common fungal infection that compromises the central nervous system (CNS) in AIDS patients.15Cryptococcus neoformans is a ubiquitous and encapsulated yeast that can affect patients with severe compromise of cell-mediated immunity, especially those with advanced HIV/AIDS disease.10 Also, but less frequently, cryptococcosis involves other immunocompromised patients as those with prolonged corticosteroid therapy, lymphomas, solid organ transplant recipients and chemotherapy and perhaps in HIV-negative patients.2 In both, HIV-seropositive and seronegative patients, disseminated cryptococcosis with CNS involvement is a life-threatening fungal infection.
Neuro-ophthalmologic signs of AIDS are common when AIDS patients are studied carefully. Here we report a case of sudden blindness secondary to bilateral optic nerve cryptococcosis in a patient with AIDS.
Case reportA 34-year-old heterosexual man, intravenous illicit drug user, with diagnosis of human immunodeficiency virus and hepatitis C virus coinfection since 1989, was admitted to our hospital with fever, headache, vomiting, meningismus and altered sensorium in June 2007.
He had history of pulmonary tuberculosis in 1997 and disseminated cryptococcosis in 1998. In January 1999, he started on antiretroviral therapy based on zidovudine, lamivudine and indinavir, with a good clinical, virological and immunological initial response. In November 2001 laboratory findings showed an undetectable plasma viral load (<50copies/mL) and a CD4 T cell count of 202cell/μL. In 2002, he decided for himself to discontinue antiretroviral therapy.
At admission, physical examination revealed fever (38°C), tachycardia (102beats/min) and weight loss (approximately 10kg in the last three months). Respiratory and cardiovascular systems were normal. Abdomen examination was also normal. He had a stiff neck and other signs of meningeal involvement. Pupils were equally reactive and there were no cranial nerve palsies. During the hospitalization he presented symptoms consistent with gradually increasing intracranial pressure such as headache and altered mental status that required multiple lumbar punctures to reduce intracranial hypertension (30–45cm H2O).
Initially, relevant laboratory findings were anemia with hematocrit 30%, hemoglobin 11,6g/dl, leukocytes 3200/mm3, platelet count 65000/mm3, plasma glucose level 67mg/dL and creatinine clearance was normal. Liver enzyme levels, coagulation tests and chest radiograph were normal. Blood and urine cultures for bacteriae, mycobacteriae and fungi were negative. The CD4T cell count was 47cell/μL and the plasma viral load was of 27 949copies/mL.
Cerebrospinal fluid (CSF) biochemical examination showed hyperproteinorrachia 1.08g/L, glucose concentration 40mg/dL with less than 5cell/μL. Direct microscopic examination of CSF with India ink showed the presence of a large number of rounded and encapsulated yeasts compatible with Cryptococcus. CSF cultures on Sabouraud dextrosa agar at 28 and 37°C showed colonies compatible with Cryptococcus that were identified as C. neoformans var. grubii by urease and phenol-oxidase production, and the lack of growth on CGB, Salbin (glycine-cyclaneximide-phenol red) and CDBT media. Cryptococcal antigen detection in CSF by latex aglutination test was positive (1/10000). Computerized tomography brain scan showed no abnormalities.
Initially, the patient was treated with intravenous amphotericin B deoxycholate at a dose of 0.7mg/kg/24h, with a poor response. Five days later, he was switched to amphotericin B in colloidal dispersion. Ten days after the hospitalization, he developed a generalized tonic–clonic seizure that was controlled with anticonvulsivant therapy. However, after this episode, the patient referred a sudden, simultaneous and bilateral blindness. Despite the optimal antifungal therapy high intracranial pressure persisted and the patient died 2 weeks after the hospitalization probably due to cerebellar tonsillar herniation.
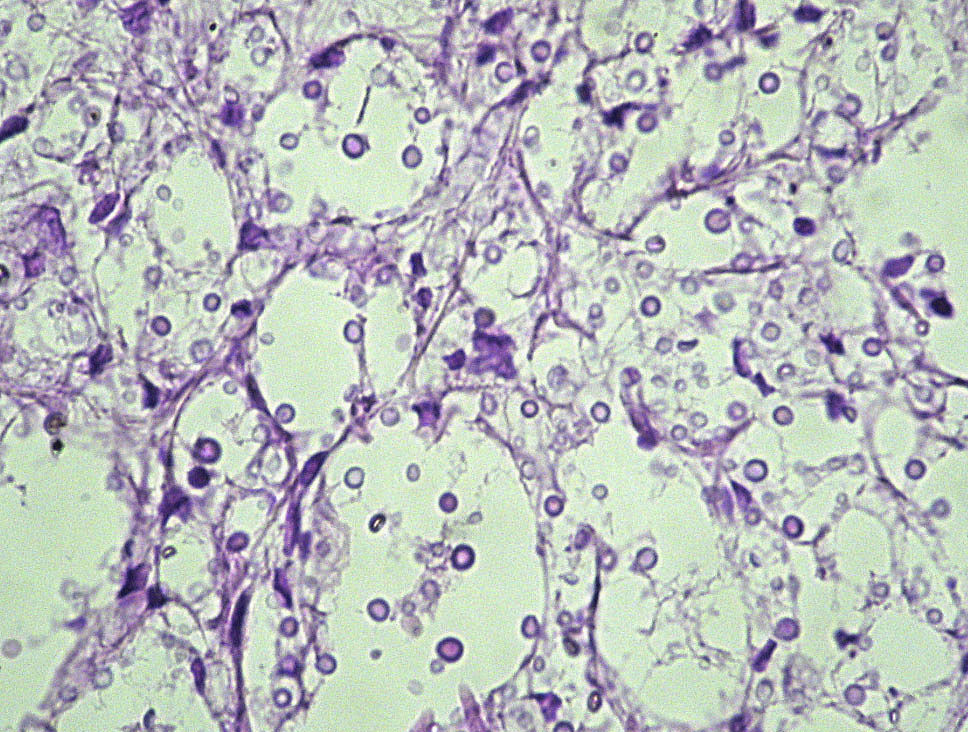
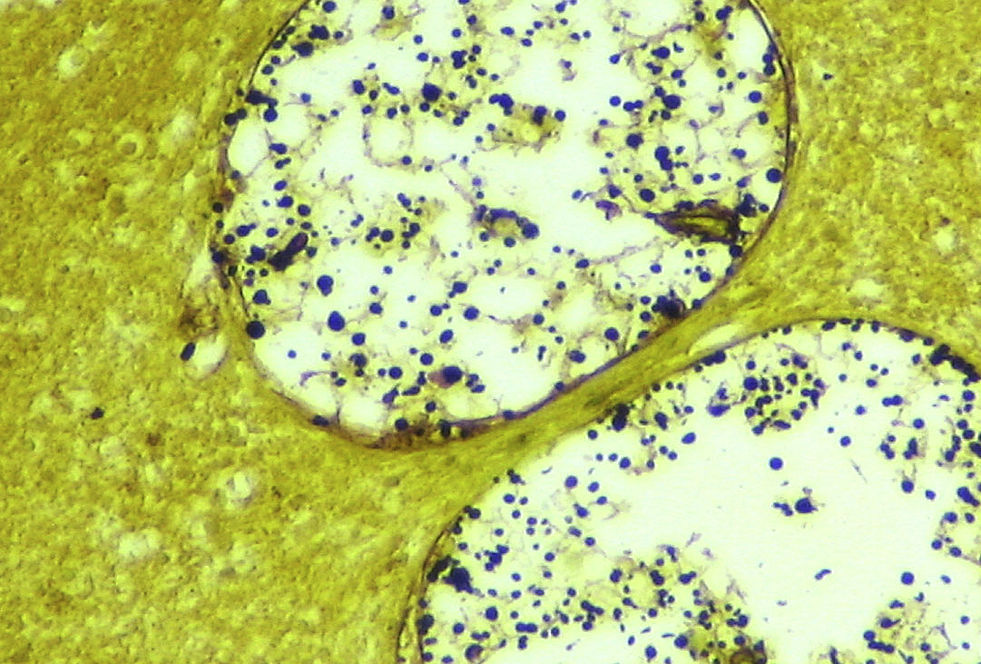
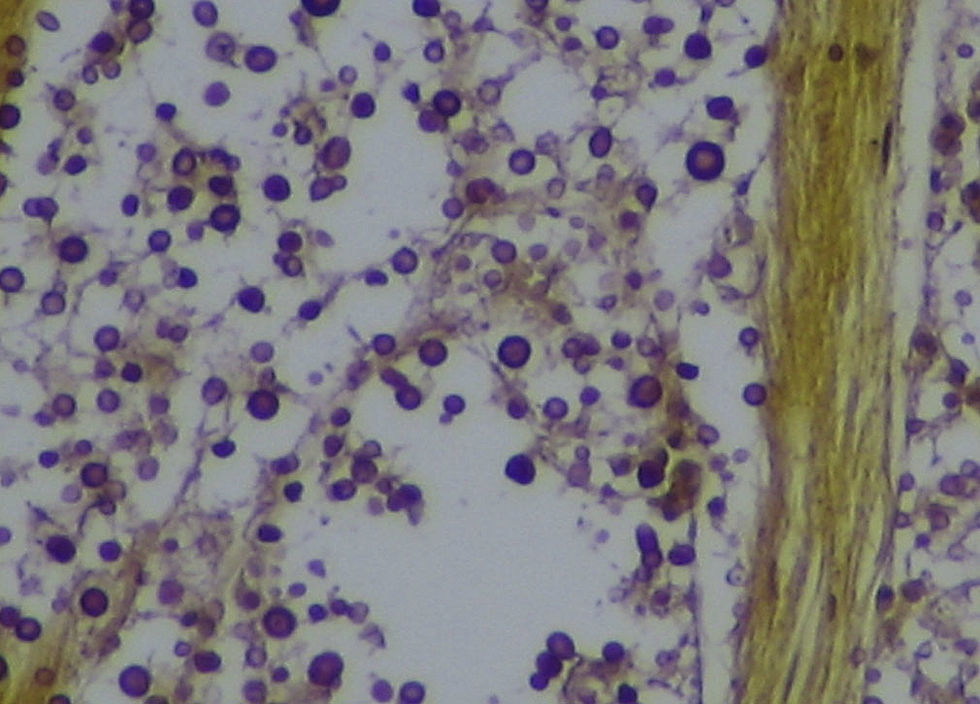
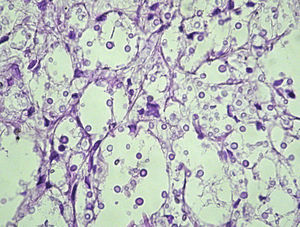
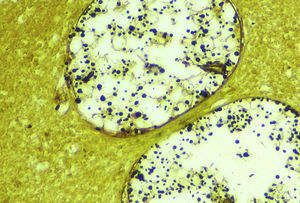
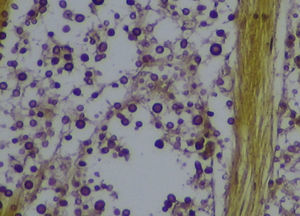
Autopsy study was performed; carefully histopathological and microscopic examination showed that the meninges were infiltrated by a large number of Cryptococcus cells (Fig. 1). The Virchow–Robin perivascular spaces showed the presence of a large number of Cryptococcus (Fig. 2). The periphery of the optic chiasm contiguous with the meningeal membranes, the optic tracts, the optic nerves and the optic chiasm were also heavily infiltrated by Cryptococcus (Fig. 3).
Cryptococcosis is an infectious disease caused by Cryptococcus neoformans and Cryptococcus gattii, encapsulated yeasts. The majority of patients with AIDS who are infected with C. neoformans develop a diffuse meningoencephalitis.11 Cryptococcal meningoencephalitis is a typical brain basal meningitis and is still the most common manifestation of systemic fungal infection in HIV-infected patients and remains associated with significant morbidity and mortality.4 The most common clinical form of neurocryptococcosis is the diffuse meningoencephalitis that presents with fever and headache in the majority of AIDS patients. Less frequently, patients may also present meningeal signs, confusion, seizures, vision loss generally due to papilledema and, rarely, focal neurological deficit.14
CNS involvement is secondary to the haematogenous spread, usually after reactivation from a prior pulmonary infection. The basal meninges of the brain are especially affected; in the meninges, the organism appears to be embedded in a mucoid material derived from the capsule of C. neoformans and C. gattii. Meningeal infection may involve the brain parenchyma or may extend along the Virchow–Robin spaces. As C. neoformans spreads along these spaces, the perivascular spaces may dilate with the mucoid gelatinous material produced by the capsule of the fungus.2
Ophthalmic manifestations of cryptococcosis in human immunodeficiency virus seropositive patients are frequent. Neuro-ophthalmic abnormalities may occur in up to one-third of patients with cryptococcal meningitis.5 In a series of eighty AIDS patients with cryptococcal infection, Kestelyn et al.8 observed papilledema as the most common clinical manifestation (32.5% of cases).
Visual loss and ocular cranial nerve palsy occurred in seven patients of this series (9%) and only two patients (2.5%) had optic nerve atrophy. Keane,7 in a series of 50 patients with AIDS, observed visual abnormalities in 18 patients (papilledema in eight, and neuropathy in four). In this series, the most common aetiologies of papilledema were cryptococcal meningitis and Toxoplasma encephalitis, and Cryptococcus and Treponema pallidum were the most frequent cause of optic neuropathy. Seaton et al.13 reviewed the ophthalmic findings in 82 immunocompetent patients in whom C.gattii caused 95% of cases. Visual loss occurred in 52.6% of survivors and was associated with optic atrophy following optic disc swelling in 60.9%. The high rate of visual loss in this series of immunocompetent patients infected predominantly with C.gattii may be associated with immune mediated optic nerve dysfunction.
There are two distinct forms of visual loss: the rapid visual loss associated with a clinical syndrome that is suggestive of optic neuritis, and the slow visual loss characterized by a progressive visual loss which may be due to the effects of intracranial pressure.12 Ophthalmic complications in cryptococcal meningitis associated with AIDS have been associated, at least in part, with persistent intracranial hypertension, as in our patient. The majority of cases of visual complications are related to increased intracranial pressure.6 Arachnoiditis may lead to subacute to chronic optic neuropathy with atrophy and visual field loss, which may be partially reversible. Limitations of eye movements may also occur by a similar mechanism.3 Finally, invasion and infection of the optic nerves and the chiasm by the fungus can occur and can be associated with acute and sudden bilateral blindness, as in our patient.9 The presence of cryptococcal organisms throughout the basal meninges and in the sheaths of the optic nerves and the chiasm, as we saw in our patient, suggests that cryptococcal meningitis may produce visual loss by fulminant necrosis of the anterior visual pathway.1