Two predictions derived from a recently introduced model of psychotherapy outcome were tested, assuming the dynamical relationship between the individual's emotional trajectory and the force of intervention necessary to change this trajectory: (a) only a high intensity treatment would succeed to lower the increasing trajectory of anxiety, and (b) high as well as low intensity treatments would equivalently lower the non-increasing trajectory of anxiety. Methods: Seventy-four adolescents (58.40% girls; M=14.65 years, SD=0.53) were randomly assigned to a high intensity treatment condition, a low intensity treatment condition, or a waiting list condition. Results: Only the high intensity treatment reduced the anxiety when participants showed an increasing trajectory (p<.01). None of the treatments reduced anxiety when a previously non-increasing trajectory was shown. Conclusions: These findings support the theoretical predictions and underscore the need to consider not only how severe the anxiety is but also the time course of anxiety in applied treatment settings.
Este informe breve tiene por objetivo poner a prueba dos predicciones derivadas de un reciente modelo sobre los resultados en psicoterapia: (a) solo un tratamiento de alta intensidad sería capaz de cambiar de dirección una trayectoria ascendente de ansiedad, y (b) tanto un tratamiento de alta como de baja intensidad podrían influir en una trayectoria no-ascendente de ansiedad. Método: Setenta y cuatro adolescentes (58,40% chicas; M=14,65 años, DT=0,53) fueron asignados aleatoriamente a una de estas condiciones: tratamiento de alta intensidad, tratamiento de baja intensidad o lista de espera. Resultados: Solo la aplicación del tratamiento de alta intensidad permitió reducir los niveles de ansiedad en los adolescentes con trayectoria creciente de dicha sintomatología (p<0,01). Además, ambos tratamientos redujeron de forma equivalente la sintomatología en individuos con trayectoria no ascendente de ansiedad. Conclusiones: Estos resultados apoyan las predicciones teóricas propuestas y subrayan la necesidad de considerar no solamente la magnitud de la sintomatología ansiosa sino también su curso temporal, en contextos clínicos.
In this brief report we used unpublished data from a treatment study to statistically test two main hypotheses derived from the theoretical model on therapy outcomes introduced by Bornas, Noguera, Pincus, and Buela-Casal (2014). The treatment study was carried out within a longitudinal research project (see Bornas, Llabres, Balle, de la Torre-Luque, & Fiol-Veny, 2014; de la Torre-Luque, Fiol-Veny, Balle, & Bornas, 2016) focused on the trajectories of anxious symptomatology in adolescents. According to that model, treatment outcome depends upon the interaction between the emotional inertia (or resistance to change, Kuppens, Oravecz, & Tuerlinckx, 2010; see also Kuppens, Allen, & Sheeber, 2010) and the treatment's energy (the force a treatment has to overcome inertia). In Physics, inertia is formally defined as “the property of matter by which it retains […] its velocity along a straight line so long as it is not acted upon by an external force”. Similarly, emotional inertia would be the property of human emotion by which it retains its course so long as it is not acted upon by an external (e.g. environmental or cognitive) force. One core statement of the theoretical model is that “the stronger the pull is toward a negative attractor region (…) the more power that is needed to return some flexibility to the system” (Bornas, Noguera et al., 2014, p. 235). Much like more energy is required to down a balloon that is ascending, more forceful treatments are required to down the anxiety when it is increasing.
Based on this model two testable predictions were made. First, only a high intensity treatment would succeed to lower the increasing (or ascending) trajectory of anxiety, since the pull toward a negative attractor region is stronger when anxiety increases; the change induced by a low intensity treatment would not be significant/meaningful. Second, high as well as low intensity treatments would equivalently lower the non-increasing trajectory of anxiety.
Anxiety trajectories were determined from two assessment points (T1 and T2) with a 6-month interval between them. Participants whose anxiety scores were higher at the second point were labeled as ‘increasing anxiety’ (IA) adolescents. The rest of them were labeled as ‘non-increasing anxiety’ (NIA) adolescents. There is no robust classification of psychological treatments based on its energy but some guidelines were proposed by the British National Institute for Health and Care Excellence, NICE (see, for instance, National Institute for Health and Care Excellence, NICE, 2011, pp. 95-96 and pp. 135-137). Likewise, clinicians would probably agree that evidence-based treatments have more energy and clearer protocols (e.g., exposure in Taboas, Ojserkis, & McKay, 2015) than psychoeducation or self-help strategies (see Bornas, Noguera et al., 2014). Treatments in this study were chosen based on these criteria.
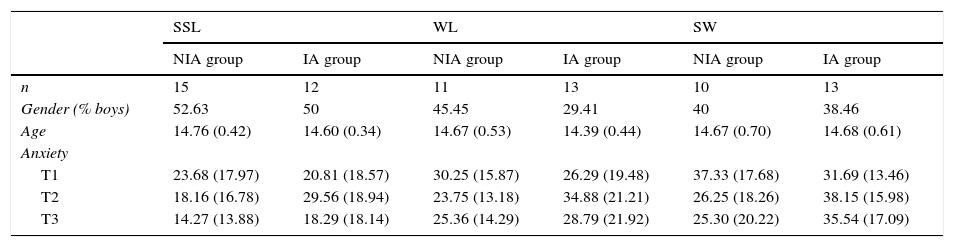
MethodsParticipantsSeventy-four Spanish adolescents (58.40% girls; M=14.65 years, SD=0.53) participating into the TrAns study were randomly assigned to one of these three conditions: treatment (n=27, 48.27% with increasing anxiety), placebo (n=23, 56.52% with increasing anxiety), and waiting list (WL, n=24, 50% with increasing anxiety). No significant differences were found regarding gender, age and anxiety at the pre-treatment assessment. When the trajectory of anxiety was taken into account, six groups were made up (see Table 1) and submitted to statistical analysis.
Descriptive features for the study groups.
| SSL | WL | SW | ||||
|---|---|---|---|---|---|---|
| NIA group | IA group | NIA group | IA group | NIA group | IA group | |
| n | 15 | 12 | 11 | 13 | 10 | 13 |
| Gender (% boys) | 52.63 | 50 | 45.45 | 29.41 | 40 | 38.46 |
| Age | 14.76 (0.42) | 14.60 (0.34) | 14.67 (0.53) | 14.39 (0.44) | 14.67 (0.70) | 14.68 (0.61) |
| Anxiety | ||||||
| T1 | 23.68 (17.97) | 20.81 (18.57) | 30.25 (15.87) | 26.29 (19.48) | 37.33 (17.68) | 31.69 (13.46) |
| T2 | 18.16 (16.78) | 29.56 (18.94) | 23.75 (13.18) | 34.88 (21.21) | 26.25 (18.26) | 38.15 (15.98) |
| T3 | 14.27 (13.88) | 18.29 (18.14) | 25.36 (14.29) | 28.79 (21.92) | 25.30 (20.22) | 35.54 (17.09) |
Note. Mean and standard deviations (between brackets) displayed for numerical data, and percentage of cases for gender.
SSL=Treatment group; WL=Waiting-list group; SW=Placebo group; NIA group=Non-increasing anxiety group; IA group=Increasing anxiety group. Anxiety was measured by the RCADS total anxiety scale (measured in 6-month intervals from T1 to T3).
The Revised Child Anxiety and Depression Scale (RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000) is a 47-item self-report questionnaire, to evaluate symptomatology of anxiety disorders (separation anxiety disorder, social phobia, generalized anxiety disorder, panic disorder, obsessive-compulsive disorder) and major depressive disorder. Moreover, an overall scale as a total level of anxiety symptoms can be obtained. The internal consistency of the overall anxiety scale was ranged from α=.94 and α=.95 within our sample, across assessments.
ProcedureThe University Bioethics Committee approved all the study procedures, and participants and their parents/tutors provided written consent.
In accordance with the TrAns project schedule, adolescents’ anxiety was assessed every six months (T1, T2 or pre-treatment, and T3 or post-treatment). The treatment group received the Super-AD programme, that is the Super Skills for Life (SSL; Essau & Ollendick, 2013) version for Spanish adolescents (de la Torre-Luque, Essau, Fiol-Veny, Balle, & Bornas, 2015). Super-AD constitutes a transdiagnostic preventive intervention focused on averting the onset of internalising syndromes. It consists of eight cognitive-behavioral group sessions. An 8-session group School work (SW) programme was delivered in the placebo group (adolescents did their homework with supervision and school habits and study skills were strengthened). Participants in the WL group followed the regular school activities and received no intervention.
Analytic strategyRCADS scores were transformed into a loglineal scale to preserve normalized distributions. A mixed repeated-measure ANOVA with one three-level factor Time (T1, T2, T3) and one six-level factor Condition (IA_SSL, IA_SW, IA_WL, NIA_SSL, NIA_SW, and NIA_WL) was performed to evaluate within- as well as between-group differences in the RCADS total scores. The anxiety scores from the WL groups along the three assessment points allowed for observing the maturational trajectory of anxiety. Bonferroni adjusted post hoc tests were used to test for pairwise comparisons.
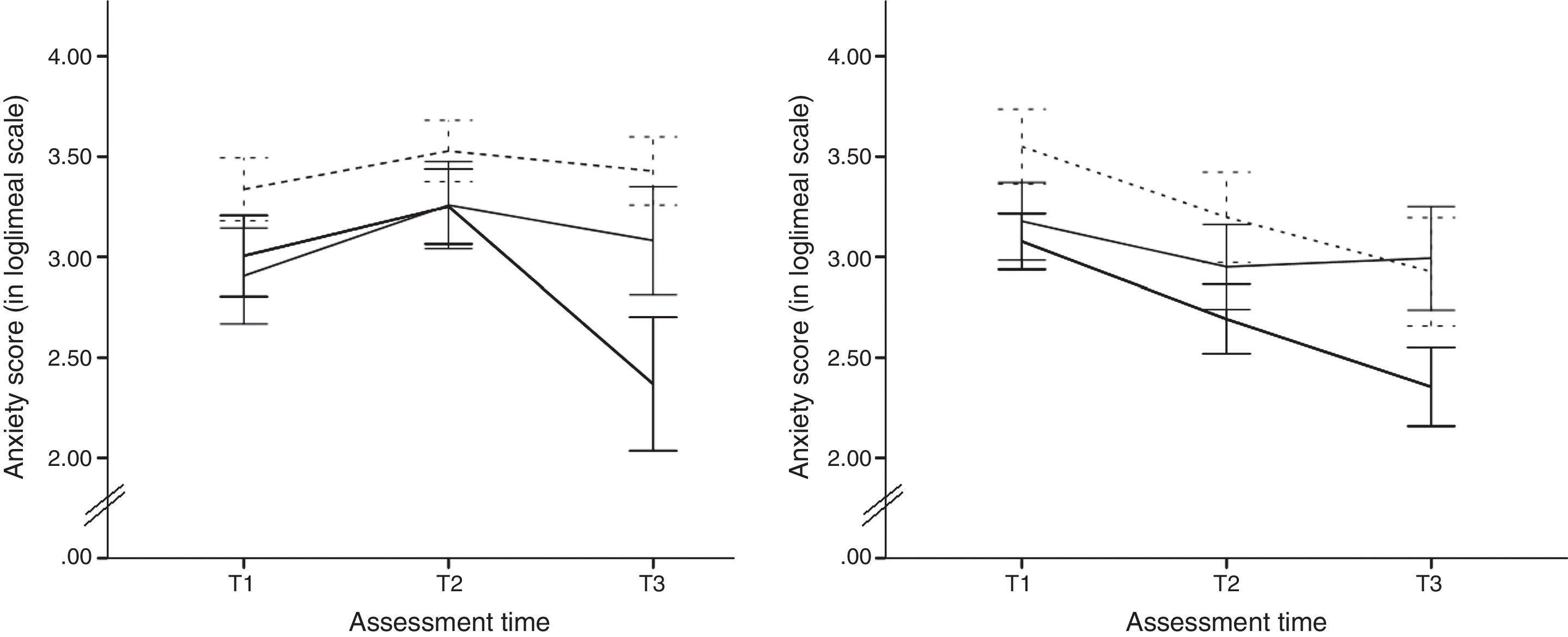
ResultsA significant interaction effect Time x Group, F (10, 136)=6.13, p<.001, η2partial=.31, was revealed by the ANOVA, as well as a significant main effect of Time, F (2, 136)=17.76, p<.001, η2partial=.21. No significant main effect of Group was found (p>.10). The IA groups did not differ in anxiety scores at any assessment time (see Figure 1). Each group showed a significant change in anxious symptomatology scores from T1 to T2. To test the specific predictions derived from the theoretical model we looked at the differences from T2 to T3 in each group. The IA_SSL group was the only one showing a large decrease in anxiety scores from pre- to post-treatment, with a Bonferroni-adjusted t (11)=5.32, p<.001, d=1.29. As to the maturational trajectory shown by the WL groups, there was not a decrease from T1 to T3 in the scores of the NIA_WL group (p>.05) whereas the NIA_SSL and the NIA_SW groups showed significant decreases in their anxiety scores, Bonferroni-adjusted t (14)=4.66, p<.001, d=1.12, and t (9)=3.28, p=.009, d=0.53, respectively. Changes in the IA groups from T1 to T3 were not significant (see Figure 1).
The trajectories of anxious symptomatology for the increased anxiety (IA) groups (left) and the non-increased anxiety (NIA) groups (right) across the three assessment times.
Note. Anxiety scores, displayed under a loglineal transformation, from the treatment (SSL) groups (dark lines), the waiting-list groups (solid grey lines), and the placebo (SW) groups (dashed grey lines).
Error bars depict the standard error of the mean.
According to a recently presented model of psychotherapy outcome (Bornas, Noguera et al., 2014) only forceful treatments can successfully overcome the patient's emotional inertia when the trajectory of anxiety is ascending/increasing. Low intensity treatments may succeed if the trajectory is not increasing. These predictions were statistically tested using data from a larger study where three groups of adolescents received three treatment conditions (SSL as the high intensity treatment, SW as the low intensity treatment, and WL or no treatment). Based on the individual anxiety trajectory (ascending or non-increasing) each group was divided into two subgroups (IA or NIA). This classification was validated by the differences in anxiety scores from T1 to T2 in all the groups. Anxiety scores from the WL groups along T1, T2, and T3 were taken as the best approach to the maturational trajectory of the anxious symptomatology scores.
The first prediction was confirmed by the results of the ANOVA. Only the high intensity treatment (SSL) largely reduced the anxiety symptomatology from pre- to post-treatment of participants with a previous increasing trajectory. Further, the energy of the SW treatment should be considered very low since the anxiety scores from the IA_WL group did not change either. In other words, the SW treatment was not able to change the maturational time course of anxiety. It is worth to say that the anxiety scores from the three IA groups at T3 (post-treatment) were statistically equivalent, i.e. all groups showed similar anxiety scores. This is not contrary to our hypothesis (the SSL did decrease the anxiety whereas the other two condition did not), but it shows that the SSL package is not a very forceful treatment. Indeed, the SSL treatment has a preventive character and it is not designed to treat severe anxiety disorders. This finding confirms the need to use more intense treatments to overcome the emotional inertia of very anxious adolescents as well as adolescents suffering from a diagnosed anxiety disorder.
The second prediction stated that the effect of high and low intensity treatments when the anxiety trajectory was non-increasing would equivalently deviate the non-increasing trajectory of anxiety. The results partly confirmed this prediction. Neither the SSL nor the SW conditions significantly lowered the anxiety scores of the NIA groups from T2 to T3, and therefore their effects were “equivalent”. We are aware, however, that the expected effect of any psychological intervention is not the “unchange” of the target (in this study, the anxiety scores). If we look at the changes in the NIA_WL group we see that its anxiety scores remained at the same level from T1 to T3. Therefore, the maturational course of anxiety along this period or time (and at this age) tends to stabilize. Since the NIA groups that received psychological treatment reduced the anxiety scores from T1 to T3, we can speculate that both of them had at least a weak impact on the maturational trajectory of anxiety. On the other hand, a floor effect may help to understand this result. Obviously, anxiety is not expected to decrease forever, and therefore the decreasing trajectory of the NIA groups should stabilize at some moment (i.e. when it reaches the “floor”). It is not reasonable, therefore, to expect that any treatment, disregarding its energy, will reduce the anxiety beyond this floor. The floor effect may be helpful also to understand why the SSL treatment reduced the anxiety of the IA group but it did not reduce the scores of the NIA group. The IA group anxiety at T2 was far from the floor and could be much reduced whereas the anxiety level in the NIA group at T2 was too close to the floor.
To sum up, this brief report underscores the need to consider (when possible) not only how severe the anxiety is but also the time course of anxiety. In this way, the effects of treatments can be explained not only by their energy (e.g. degree of protocolization and scheduling, use of tested techniques, etc.) but also by their impact on systems (adolescents’ emotions) that move and follow specific trajectories across time.
FundingThis study was supported by the Spanish Ministry of Economy and Competitiveness grant ref. PSI2012-34780.
All authors would thank to Dr. Essau (University of Roehampton, UK) for the training and supervision in the SSL intervention.