The aim of this study was to investigate the differences in the prevalence of somatic diseases among combat veterans and their contemporaries who were not exposed to the traumatic experience at the battlefield, and to determine whether socio-demographic factors, exposure to war-time trauma and/or injury might predict individual somatic diseases. The study included 1,558 subjects living in south Croatia: 501 male combat veterans with Posttraumatic Stress Disorder (PTSD) and the corresponding control group of 825 men who were not exposed to combat experience. Veterans with PTSD, regardless of the length of time spent in war, suffered more often from cardiovascular, dermatological, musculoskeletal, pulmonary and metabolic diseases than corresponding control subjects who were not exposed to combat experience. The predictors of cardiovascular, musculoskeletal and malignant diseases in veterans were age, length of time spent in combat, having been wounded. A longer period in the combat zone was associated with arrhythmias in veterans with PTSD complicated with other psychiatric comorbidities. PTSD as a result of exposure to war trauma increases the possibility of developing somatic diseases.
El propósito de este estudio ha sido comparar la frecuencia de trastornos somáticos en veteranos de guerra y personas no expuestas a la experiencia traumática del campo de batalla, así como determinar si la exposición a factores socio-demográficos en tiempo de guerra pueden predisponer a traumas, alteraciones o trastornos somáticos. El estudio incluye 1,558 sujetos del sur de Croacia: 501 varones veteranos de guerra con síndrome de estrés postraumático (TEPT) y un grupo de control de 825 varones no expuestos a la experiencia de combate. Los veteranos con TEPT, independientemente del tiempo pasado en la guerra, desarrollan más a menudo alteraciones gastrointestinales, cardiovasculares, dermatológicas, locomotoras, pulmonares y metabólicas que los sujetos del grupo control. Los indicadores de alteraciones cardiológicas, locomotoras, entre otros, en veteranos han sido la edad, el tiempo pasado en combate y el daño allí sufrido. Un largo período en la zona de combate ha sido asociado con arritmias y otras complicaciones de tipo psiquiátrico. El TEPT, como resultado de la exposición a experiencias traumáticas del campo de batalla, incrementa la posibilidad de desarrollo de trastornos somáticos.
Numerous studies with divergent results have examined the connection between physical and mental health, and the impact of stress and traumatic events on the hypothalamic-pituitary-adrenal (HPA) axis, with the consequent metabolic disorders and impairments of cortisol secretion and lipid status (Ginzburg & Solomon, 2011), or physical health in combat veterans with PTSD (O’Toole & Catts, 2008; Vasterling et al., 2008). These contradictory results support the complexity of this relationship, in addition to the important influences of genetic vulnerability, the HPA axis changes, smoking and substance abuse (Qureshi, Pyne, Magruder, Schultz, & Kunik, 2009; Zen, Whooley, Zhao, & Cohen, 2012). Some studies reported a higher incidence of arthritis, pulmonary disease (O’Toole & Catts, 2008), dermatological disorders (eczema), back and other musculoskeletal disorders, genitourinary disorders in the general population with PTSD (Glaesmer, Brähler, Gündel, & Riedel-Heller, 2011) and veterans (O’Toole & Catts, 2008), while others showed a significant association between PTSD and diabetes (Boyko et al., 2010), psoriasis, thyroid disease (Boscarino, 2004), cardiovascular diseases (Coughlin, 2011; Edmundson & Cohen, 2013) and ulcers (Fink, 2011). The fact that over 50% of veterans with PTSD also have another psychiatric diagnosis (Ginzburg, Ein-Dor, & Solomon, 2010) raises the question of the impact of psychiatric comorbidity on the occurrence of physical illnesses. We are not aware of any previous studies investigating the differences in the prevalence of somatic disorders among veterans with PTSD, with or without comorbid diagnoses. Given the large numbers of veterans with PTSD in Croatia in the aftermath of the 1991-1995 war, who undoubtedly represent a significant public health problem, there is a need to study their physical health.
The aim of this study was to investigate the differences in the prevalence of somatic diseases among combat veterans and their contemporaries who were not exposed to the traumatic experience in the battlefield, and to determine whether socio-demographic factors (education, marital status, employment status), the effects of combat exposure to wartime trauma, and/or injury might be used as predictors of development of somatic diseases. The hypothesis was that veterans will have higher prevalence of somatic disorders compared to the general population matched for age and sex, and that those injuries and traumatic experiences will significantly influence the occurrence of somatic illnesses in veterans. Another aim was to elucidate a prevalence of somatic diseases among veterans with PTSD and psychiatric comorbidities, compared to subjects without comorbid diagnoses.
MethodParticipants and instrumentsThis case control study included 1,558 subjects living in central Dalmatia in the region of Split-Dalmatia County. The test group consists of male combat veterans, 36 to 65 years of age, diagnosed with PTSD resulting from the combat experience after the Homeland war in Croatia, who were in outpatient treatment. The group was formed from a sample of all combat veterans who were diagnosed and/or treated at the Regional Center for Psychotrauma, Split Clinical Hospital Center, from May 2010 to May 2011. A total of 1,023 veterans were examined, of whom 759 were diagnosed with PTSD and 501 agreed to participate in the study. The remaining 258 were excluded from the study due to various reasons; 108 of them did not accepted to participate in the study, with the other 150 questionnaires were not properly filled, (49 of them Mississippi scale was not properly filled, and in 101 the data were insufficient). The diagnosis of PTSD was established according to the diagnostic criteria for PTSD based on the ICD-10 criteria (World Health Organization, 1992), but also with a Structured Clinical Interview (SCID) for DSM-IV (First, Spitzer, Gibbon, & Williams, 2000). All participants were assessed systematically. Particular symptoms were evaluated using the self-report questionnaire of the Mississippi Scale for Combat Related Posttraumatic Stress Disorder (M-PTSD) (Keane, Cadell, & Taylor, 1988). PTSD assessed based on combat/military traumas only. This questionnaire is a 35-item self-report measure that assesses combat-related PTSD in veteran populations. This measure has demonstrated good test-retest reliability (r=.97, 1-week interval), internal consistency (alpha= .94) and diagnostic accuracy (90% diagnostic efficiency) in a sample of Vietnam combat veterans (Kulka et al., 1991). Selected symptoms were collected and diagnoses established by three psychiatrists and two psychologists with an extensive experience in war related psychopathologies who were working with veterans with PTSD. Comorbid diagnoses were established using the ICD-10 and SCID according to DSM-IV.
The average age of the participants was 47.5±6.6 years. Most of them (n=384) had a secondary school education (10–12 years of school). The majority (n=384) were married, 78 were single, 37 were divorced and two were widowed. The largest number (n=358) were retired, while 63 of them were unemployed and 80 veterans were employed. Most of the participants (n=202) had spent more than three years on the battlefield, 104 between 2 and 3 years and 130 between 1 and 2 years. Of the total number, 47 had been wounded.
Control group. The total patient populations of three family medical practices in three different cities were examined, which included persons from urban, rural and island milieus, which were not exposed to war activities. There were a total of 5,000 subjects, of whom 2,389 were men and 825 met the criteria for participation in the study. The inclusion criteria were male gender between 36 and 65 years of age. The exclusion criteria were the existence of psychological problems or psychiatric treatment (all codes from F-01 to F-09, according to the ICD-10) and combat duty in the Homeland war. From all patient population, 913 were younger than 35 or older than 65 years, 561 subjects were involved in acts of war. From the subjects examined, 204 showed psychological problems, of which 114 as a result of participation in the war. Assessment of physical diseases was conducted by systematic examination of the medical records, medical examination by three experienced family physicians who received equivalent training, but unfortunately without rater-interrater reliability. Assessment of psychiatric disorders in the control group was conducted by a family physician, who found no criterion for the diagnosis of disorders of the F 00-F 99 ICD-10. In addition, inspection in the whole life medical records for each of the control respondents did not reveal presence of any psychiatric disorders. Average age of the control group was 46.9±7.9 years. Out of 825 included control subjects, most of the participants (n=607) had a secondary school education (10–12 years of school). The majority (n=643) were married, 157 were single and 25 were divorced or widowed. The largest number were employed (n=591), 148 were retired with pensions and 86 were unemployed.
Procedure and data analysisData were collected by three psychiatrists, two psychologists and four family physicians using a questionnaire especially designed for this purpose. The questionnaire collected data on socio-demographic status (marital status, education, employment status, presence/absence at war and for the group of veterans the length combat duty and wounds). The data on physical illness were divided into gastrointestinal, cardiovascular, dermatological, neurological, metabolic, pulmonary, musculoskeletal systems, tumors, and other disease groups. Information on diseases was obtained from interviews with the subjects, medical examination and inspection of their medical records.
The resulting data described the sociodemographic data, data on the diseases in both groups (veterans and the general population) and differences in diseases, the length of combat duty during the war and wounds incurred, which represented predictors of individual physical illnesses. In the second analysis, the frequencies of physical illnesses in veterans with and without psychiatric comorbidity were compared.
Univariate logistic regression was performed in order to determine the odds ratio for a specific diagnosis in cases and controls. For this purpose, all the variables of a specific diagnose (including Diseases of the Gastrointestinal Tract, Cardiological Diseases, Dermatological Diseases, Diseases of the Locomotor Apparatus, Neurological Diseases, Metabolic Diseases, Pulmonary Diseases, Malignant Diseases and Other) were recoded into variables with two levels (YES= is diagnosed with the specific disease; NO= is not diagnosed with the specific disease). All the binary logistic regression analysis were performed with the inclusion of recoded variables in the model. The adjusted odds ratios were calculated after the inclusion of the following possible confounding factors in the multiple binary logistic regression model: age, education, marital status and employment status. Along with the adjusted odds ratios for a specific disease, Chi squares and a p value of a specific model including the possible confounding factors were reported. The variables were evaluated descriptively (presented as means and standard deviation), and analyzed using binary logistic regression. For a subsequent comparison between the groups, the Student's t-test and χ2 test were used. The software program SPSS 12.0 for Windows (Chicago, IL: SPSS Inc., 2003) was used for data analysis, with the significance level set at .05.
The study was approved by the Ethics Committee of the University of Split Hospital Center. All the subjects were familiarized with the study and gave their written informed consent.
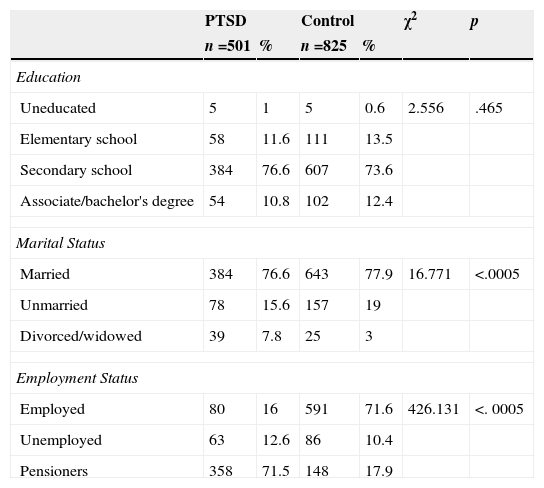
ResultsDifferences in the sociodemographic factorsThere was no significant difference in age of the veterans and control group (t =1.36 p=.174). However, significant difference was detected in marital status (χ2 (2)=16.77; p=.0005) and employment status (χ2 (2)=426.13; p=.0005). In the control group, there was a marginally higher number of unmarried men and a lower number of divorced men and widowers. Regarding employment status, the veterans were more frequently retired and subjects in the control group were more frequently employed (Table 1).
Differences in the sociodemographic factors between veterans with PTSD and the control group.
| PTSD | Control | χ2 | p | |||
|---|---|---|---|---|---|---|
| n =501 | % | n =825 | % | |||
| Education | ||||||
| Uneducated | 5 | 1 | 5 | 0.6 | 2.556 | .465 |
| Elementary school | 58 | 11.6 | 111 | 13.5 | ||
| Secondary school | 384 | 76.6 | 607 | 73.6 | ||
| Associate/bachelor's degree | 54 | 10.8 | 102 | 12.4 | ||
| Marital Status | ||||||
| Married | 384 | 76.6 | 643 | 77.9 | 16.771 | <.0005 |
| Unmarried | 78 | 15.6 | 157 | 19 | ||
| Divorced/widowed | 39 | 7.8 | 25 | 3 | ||
| Employment Status | ||||||
| Employed | 80 | 16 | 591 | 71.6 | 426.131 | <. 0005 |
| Unemployed | 63 | 12.6 | 86 | 10.4 | ||
| Pensioners | 358 | 71.5 | 148 | 17.9 | ||
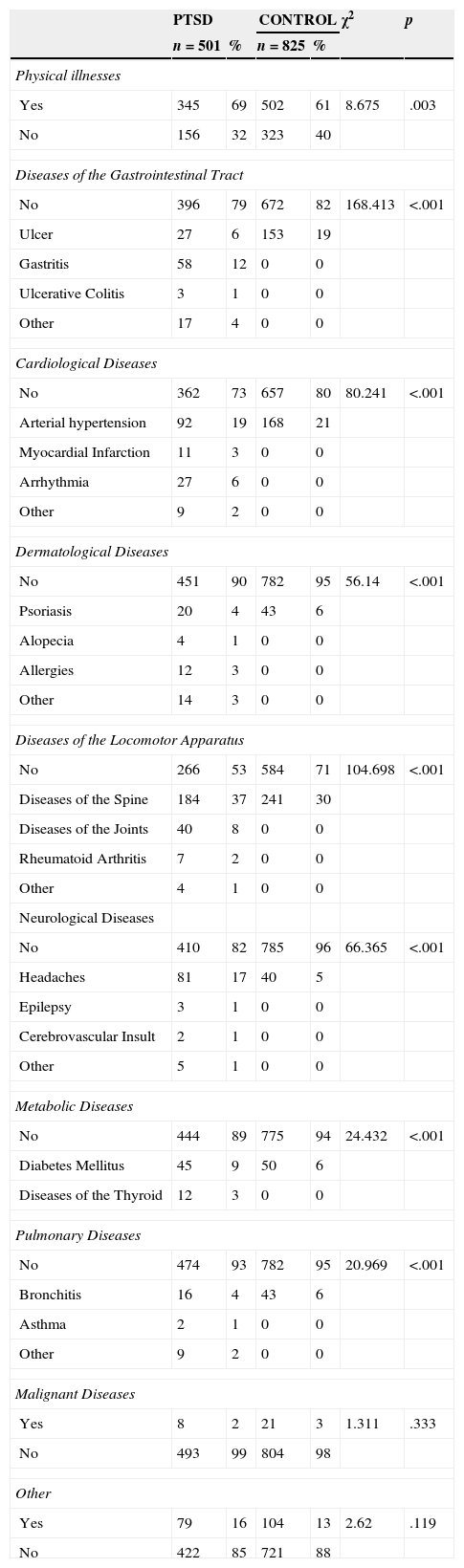
The difference in the overall prevalence of physical illnesses between these two groups was significant (χ2 (1)=8.67; p=.003) in the morbidity from gastrointestinal, cardiac, dermatological, musculoskeletal, respiratory and metabolic diseases (Table 2). With the exception of gastrointestinal illnesses, all other somatic diseases were more prevalent among the combat veterans suffering from PTSD compared to control group. In the group of subjects with gastrointestinal illnesses, ulcer disease was more common in the general population, while gastritis and ulcerative colitis were more prevalent among the combat veterans (Table 2). Although total cardiovascular diseases were significantly more common among the combat veterans, arterial hypertension was more common in the control group, while myocardial infarction, arrhythmia and other illnesses were more common in the group of combat veterans. Out of dermatological diseases, psoriasis was more common in the control population, but allergies, alopecia and other diseases were more frequent in the group of veterans (χ2 (4)=51.14; p=.001). All diseases of the musculoskeletal system were more frequent in combat veterans (χ2 (4)=104.69; p<.001), which include spinal disorders, arthritis and rheumatoid arthritis, compared to control subjects. All neurological diseases were more common in the group of combat veterans (χ2 (4)=66.36; p=.001), with the most common consisting of headache, epilepsy and cerebrovascular insult(s). Metabolic diseases were more common in combat veterans (χ2 (2)=24.432; p<.001), such as diabetes mellitus and thyroid disease, than in control subjects. There were no differences in the frequencies of malignant and other diseases between these two groups (Table 2). All stated differences are statistically significant also when the influence on length of time spent in combat is controlled, and it means that differences in more often physical illnesses in veterans are mainly results of PTSD rather than duration of trauma exposure (Table 3).
Differences in morbidity from physical diseases between veterans with PTSD and the control group.
| PTSD | CONTROL | χ2 | p | |||
|---|---|---|---|---|---|---|
| n=501 | % | n=825 | % | |||
| Physical illnesses | ||||||
| Yes | 345 | 69 | 502 | 61 | 8.675 | .003 |
| No | 156 | 32 | 323 | 40 | ||
| Diseases of the Gastrointestinal Tract | ||||||
| No | 396 | 79 | 672 | 82 | 168.413 | <.001 |
| Ulcer | 27 | 6 | 153 | 19 | ||
| Gastritis | 58 | 12 | 0 | 0 | ||
| Ulcerative Colitis | 3 | 1 | 0 | 0 | ||
| Other | 17 | 4 | 0 | 0 | ||
| Cardiological Diseases | ||||||
| No | 362 | 73 | 657 | 80 | 80.241 | <.001 |
| Arterial hypertension | 92 | 19 | 168 | 21 | ||
| Myocardial Infarction | 11 | 3 | 0 | 0 | ||
| Arrhythmia | 27 | 6 | 0 | 0 | ||
| Other | 9 | 2 | 0 | 0 | ||
| Dermatological Diseases | ||||||
| No | 451 | 90 | 782 | 95 | 56.14 | <.001 |
| Psoriasis | 20 | 4 | 43 | 6 | ||
| Alopecia | 4 | 1 | 0 | 0 | ||
| Allergies | 12 | 3 | 0 | 0 | ||
| Other | 14 | 3 | 0 | 0 | ||
| Diseases of the Locomotor Apparatus | ||||||
| No | 266 | 53 | 584 | 71 | 104.698 | <.001 |
| Diseases of the Spine | 184 | 37 | 241 | 30 | ||
| Diseases of the Joints | 40 | 8 | 0 | 0 | ||
| Rheumatoid Arthritis | 7 | 2 | 0 | 0 | ||
| Other | 4 | 1 | 0 | 0 | ||
| Neurological Diseases | ||||||
| No | 410 | 82 | 785 | 96 | 66.365 | <.001 |
| Headaches | 81 | 17 | 40 | 5 | ||
| Epilepsy | 3 | 1 | 0 | 0 | ||
| Cerebrovascular Insult | 2 | 1 | 0 | 0 | ||
| Other | 5 | 1 | 0 | 0 | ||
| Metabolic Diseases | ||||||
| No | 444 | 89 | 775 | 94 | 24.432 | <.001 |
| Diabetes Mellitus | 45 | 9 | 50 | 6 | ||
| Diseases of the Thyroid | 12 | 3 | 0 | 0 | ||
| Pulmonary Diseases | ||||||
| No | 474 | 93 | 782 | 95 | 20.969 | <.001 |
| Bronchitis | 16 | 4 | 43 | 6 | ||
| Asthma | 2 | 1 | 0 | 0 | ||
| Other | 9 | 2 | 0 | 0 | ||
| Malignant Diseases | ||||||
| Yes | 8 | 2 | 21 | 3 | 1.311 | .333 |
| No | 493 | 99 | 804 | 98 | ||
| Other | ||||||
| Yes | 79 | 16 | 104 | 13 | 2.62 | .119 |
| No | 422 | 85 | 721 | 88 | ||
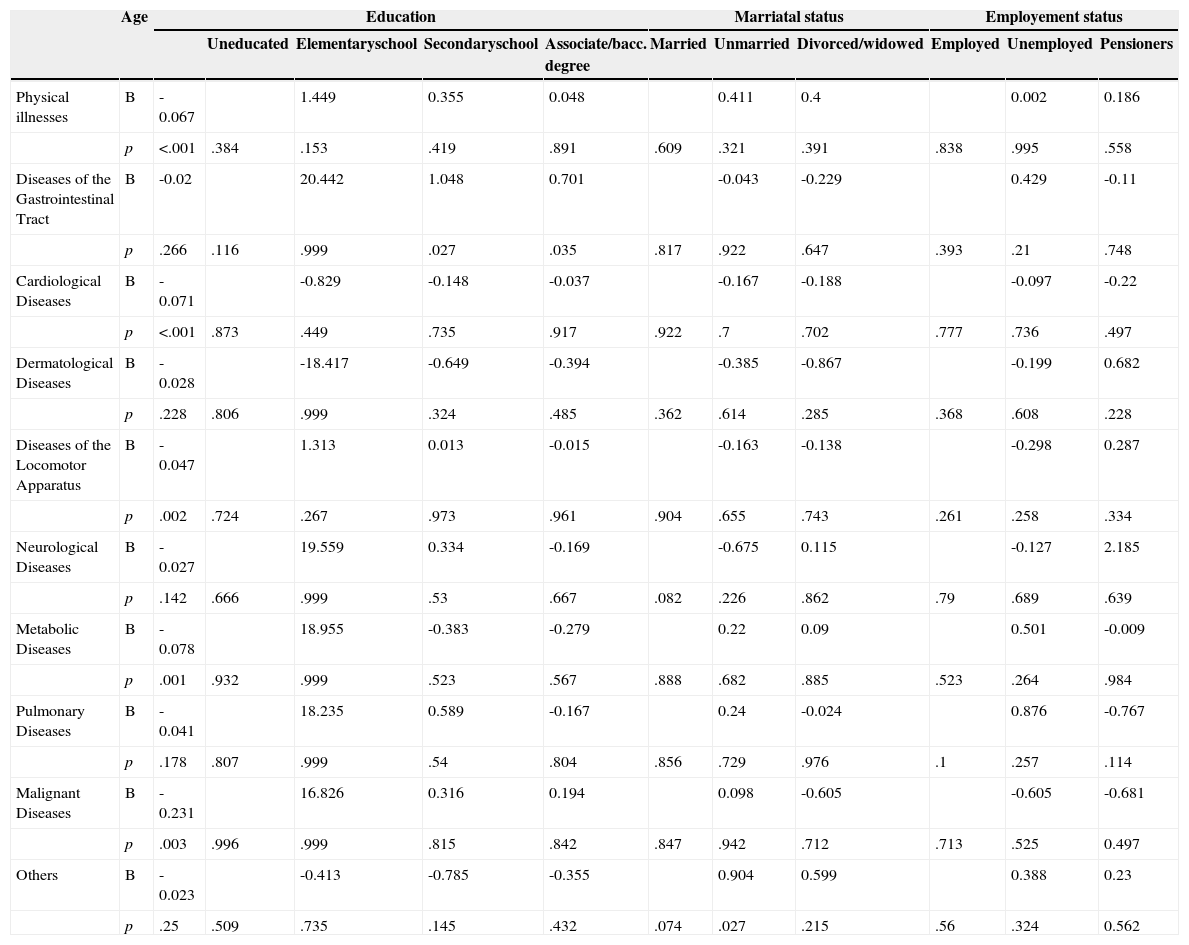
Predictors of morbidity from physical diseases in the combat veterans with PTSD.
| Age | Education | Marriatal status | Employement status | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Uneducated | Elementaryschool | Secondaryschool | Associate/bacc. degree | Married | Unmarried | Divorced/widowed | Employed | Unemployed | Pensioners | |||
| Physical illnesses | B | -0.067 | 1.449 | 0.355 | 0.048 | 0.411 | 0.4 | 0.002 | 0.186 | |||
| p | <.001 | .384 | .153 | .419 | .891 | .609 | .321 | .391 | .838 | .995 | .558 | |
| Diseases of the Gastrointestinal Tract | B | -0.02 | 20.442 | 1.048 | 0.701 | -0.043 | -0.229 | 0.429 | -0.11 | |||
| p | .266 | .116 | .999 | .027 | .035 | .817 | .922 | .647 | .393 | .21 | .748 | |
| Cardiological Diseases | B | -0.071 | -0.829 | -0.148 | -0.037 | -0.167 | -0.188 | -0.097 | -0.22 | |||
| p | <.001 | .873 | .449 | .735 | .917 | .922 | .7 | .702 | .777 | .736 | .497 | |
| Dermatological Diseases | B | -0.028 | -18.417 | -0.649 | -0.394 | -0.385 | -0.867 | -0.199 | 0.682 | |||
| p | .228 | .806 | .999 | .324 | .485 | .362 | .614 | .285 | .368 | .608 | .228 | |
| Diseases of the Locomotor Apparatus | B | -0.047 | 1.313 | 0.013 | -0.015 | -0.163 | -0.138 | -0.298 | 0.287 | |||
| p | .002 | .724 | .267 | .973 | .961 | .904 | .655 | .743 | .261 | .258 | .334 | |
| Neurological Diseases | B | -0.027 | 19.559 | 0.334 | -0.169 | -0.675 | 0.115 | -0.127 | 2.185 | |||
| p | .142 | .666 | .999 | .53 | .667 | .082 | .226 | .862 | .79 | .689 | .639 | |
| Metabolic Diseases | B | -0.078 | 18.955 | -0.383 | -0.279 | 0.22 | 0.09 | 0.501 | -0.009 | |||
| p | .001 | .932 | .999 | .523 | .567 | .888 | .682 | .885 | .523 | .264 | .984 | |
| Pulmonary Diseases | B | -0.041 | 18.235 | 0.589 | -0.167 | 0.24 | -0.024 | 0.876 | -0.767 | |||
| p | .178 | .807 | .999 | .54 | .804 | .856 | .729 | .976 | .1 | .257 | .114 | |
| Malignant Diseases | B | -0.231 | 16.826 | 0.316 | 0.194 | 0.098 | -0.605 | -0.605 | -0.681 | |||
| p | .003 | .996 | .999 | .815 | .842 | .847 | .942 | .712 | .713 | .525 | 0.497 | |
| Others | B | -0.023 | -0.413 | -0.785 | -0.355 | 0.904 | 0.599 | 0.388 | 0.23 | |||
| p | .25 | .509 | .735 | .145 | .432 | .074 | .027 | .215 | .56 | .324 | 0.562 | |
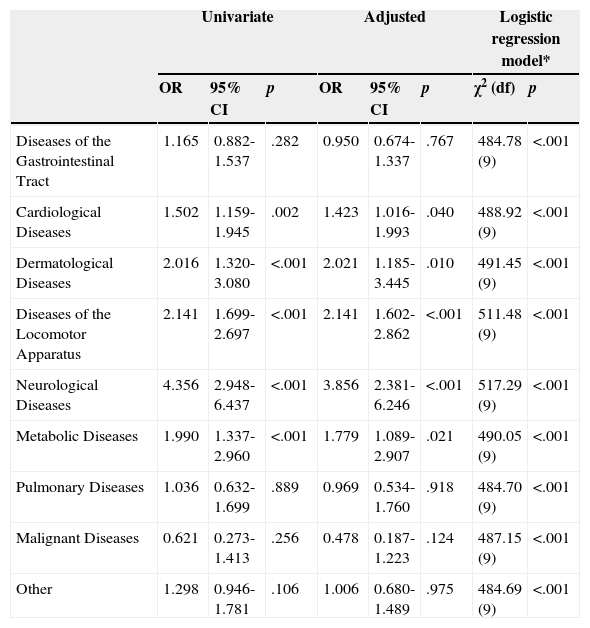
The results of the binary logistic regression confirmed that the patients with PTSD were statistically significantly more likely to be diagnosed with cardiological, dermatological, neurological, metabolic diseases and diseases of the locomotor apparatus (Table 4). When adjusted for possible confounding factors among the cases and controls, including age, education, marital status and employment status, the adjusted odds ratios were still statistically significant in all variables that proved significant in the univariate regression model. After the adjustment, PTSD patients were almost 4 times more likely to be diagnosed with neurological diseases (odds ratio 3.856; 2.381-6.246; p<.001), and two times more likely to be diagnosed with diseases of the locomotor apparatus (odds ratio 2.141; 1.602-2.862; p<.001) and dermatological diseases (odds ratio 2.021; 1.185-3.445; p=.010). Odds ratio for metabolic (odds ratio 1.779; 1.089-2.907; p=.021) and cardiological diseases (odds ratio 1.423; 1.016-1.993; p=.040) were somewhat smaller, but still statistically significant after the adjustment.
Odds ratio for specific diseases in PTSD patients compared to controls in univariate and multiple logistic regression models.
| Univariate | Adjusted | Logistic regression model* | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | χ2 (df) | p | |
| Diseases of the Gastrointestinal Tract | 1.165 | 0.882-1.537 | .282 | 0.950 | 0.674-1.337 | .767 | 484.78 (9) | <.001 |
| Cardiological Diseases | 1.502 | 1.159-1.945 | .002 | 1.423 | 1.016-1.993 | .040 | 488.92 (9) | <.001 |
| Dermatological Diseases | 2.016 | 1.320-3.080 | <.001 | 2.021 | 1.185-3.445 | .010 | 491.45 (9) | <.001 |
| Diseases of the Locomotor Apparatus | 2.141 | 1.699-2.697 | <.001 | 2.141 | 1.602-2.862 | <.001 | 511.48 (9) | <.001 |
| Neurological Diseases | 4.356 | 2.948-6.437 | <.001 | 3.856 | 2.381-6.246 | <.001 | 517.29 (9) | <.001 |
| Metabolic Diseases | 1.990 | 1.337-2.960 | <.001 | 1.779 | 1.089-2.907 | .021 | 490.05 (9) | <.001 |
| Pulmonary Diseases | 1.036 | 0.632-1.699 | .889 | 0.969 | 0.534-1.760 | .918 | 484.70 (9) | <.001 |
| Malignant Diseases | 0.621 | 0.273-1.413 | .256 | 0.478 | 0.187-1.223 | .124 | 487.15 (9) | <.001 |
| Other | 1.298 | 0.946-1.781 | .106 | 1.006 | 0.680-1.489 | .975 | 484.69 (9) | <.001 |
Note. *Including the specific diagnosis and confounding variables age, education, marital status and employment status. CI=95% confidence intervals; OR=odds ratio for negative change; Univariate=univariate binary logistic regression; Adjusted=adjusted or multivariate binary logistic regression controlling for age, education, marital status and employment status.
In the group of veterans suffering from PTSD, the predictors of the incidence of physical illness were age (B=-0.067, p=.005), the length of time spent on the battlefield (B=0.182, p=.063), and whether they were wounded. Higher age was significant predictor of cardiovascular (B=-0.071, p<.005), musculoskeletal (B=-0.047, p=.002) metabolic (B=-0.078, p=.001) and malignant (B=-0.231, p=.003) diseases. Secondary or higher education was a predictor of gastrointestinal diseases (B=0.701, p=.035) (Table 4). A predictor of cardiovascular (B=0.221, p=.026), musculoskeletal (B=0.254, p=.004), neurological (B=0.264, p=.018) and pulmonary (B=-0.475, p=.013) diseases was the length of time spent on musculoskeletal (B=-0.582, p=.073) and malignant (B=-1.972, p=.038) diseases.
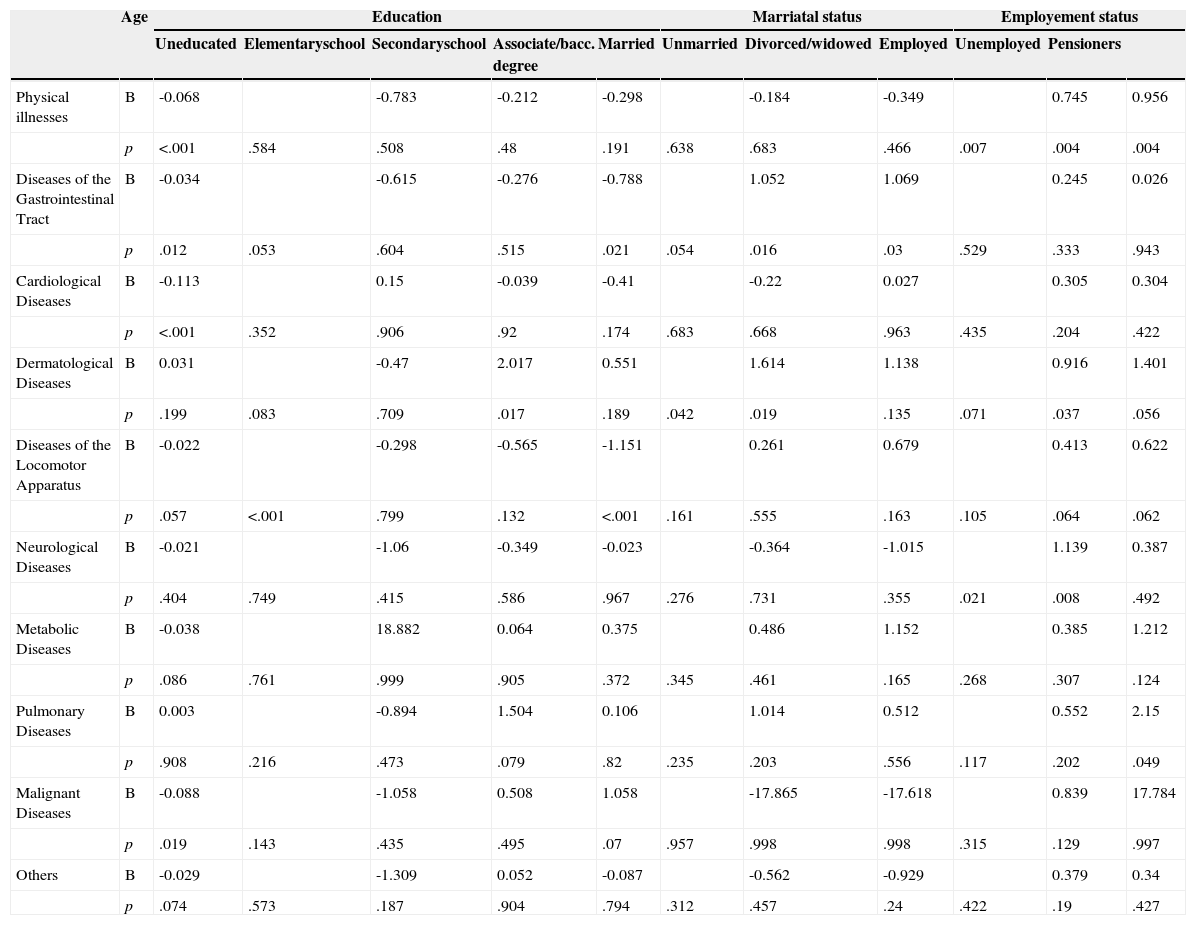
In the control group, age was a predictor of the occurrence of total physical diseases (B=-0.068, p<.005) but also gastrointestinal (B=-0.034, p=.012), cardiovascular (B=-0.113, p<.005) and malignant (B=-0.088, p=.019) diseases, as well as the prediction limit for musculoskeletal diseases (B=-0.022, p=.057). Higher education was a predictor of musculoskeletal diseases and cancer, while being single was a predictor of gastrointestinal diseases. Being employed was a predictor of general physical diseases, particularly regarding dermatological (psoriasis) and neurological (headache) diseases (Table 5).
Predictors of morbidity from physical diseases in the control group.
| Age | Education | Marriatal status | Employement status | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Uneducated | Elementaryschool | Secondaryschool | Associate/bacc. degree | Married | Unmarried | Divorced/widowed | Employed | Unemployed | Pensioners | |||
| Physical illnesses | B | -0.068 | -0.783 | -0.212 | -0.298 | -0.184 | -0.349 | 0.745 | 0.956 | |||
| p | <.001 | .584 | .508 | .48 | .191 | .638 | .683 | .466 | .007 | .004 | .004 | |
| Diseases of the Gastrointestinal Tract | B | -0.034 | -0.615 | -0.276 | -0.788 | 1.052 | 1.069 | 0.245 | 0.026 | |||
| p | .012 | .053 | .604 | .515 | .021 | .054 | .016 | .03 | .529 | .333 | .943 | |
| Cardiological Diseases | B | -0.113 | 0.15 | -0.039 | -0.41 | -0.22 | 0.027 | 0.305 | 0.304 | |||
| p | <.001 | .352 | .906 | .92 | .174 | .683 | .668 | .963 | .435 | .204 | .422 | |
| Dermatological Diseases | B | 0.031 | -0.47 | 2.017 | 0.551 | 1.614 | 1.138 | 0.916 | 1.401 | |||
| p | .199 | .083 | .709 | .017 | .189 | .042 | .019 | .135 | .071 | .037 | .056 | |
| Diseases of the Locomotor Apparatus | B | -0.022 | -0.298 | -0.565 | -1.151 | 0.261 | 0.679 | 0.413 | 0.622 | |||
| p | .057 | <.001 | .799 | .132 | <.001 | .161 | .555 | .163 | .105 | .064 | .062 | |
| Neurological Diseases | B | -0.021 | -1.06 | -0.349 | -0.023 | -0.364 | -1.015 | 1.139 | 0.387 | |||
| p | .404 | .749 | .415 | .586 | .967 | .276 | .731 | .355 | .021 | .008 | .492 | |
| Metabolic Diseases | B | -0.038 | 18.882 | 0.064 | 0.375 | 0.486 | 1.152 | 0.385 | 1.212 | |||
| p | .086 | .761 | .999 | .905 | .372 | .345 | .461 | .165 | .268 | .307 | .124 | |
| Pulmonary Diseases | B | 0.003 | -0.894 | 1.504 | 0.106 | 1.014 | 0.512 | 0.552 | 2.15 | |||
| p | .908 | .216 | .473 | .079 | .82 | .235 | .203 | .556 | .117 | .202 | .049 | |
| Malignant Diseases | B | -0.088 | -1.058 | 0.508 | 1.058 | -17.865 | -17.618 | 0.839 | 17.784 | |||
| p | .019 | .143 | .435 | .495 | .07 | .957 | .998 | .998 | .315 | .129 | .997 | |
| Others | B | -0.029 | -1.309 | 0.052 | -0.087 | -0.562 | -0.929 | 0.379 | 0.34 | |||
| p | .074 | .573 | .187 | .904 | .794 | .312 | .457 | .24 | .422 | .19 | .427 | |
All veterans examined were PTSD diagnosed. Psychiatric comorbidity was present in 62% of the subjects, most commonly Enduring Personality Change After Catastrophic Experience (EPCACE) (F62.0), detected in over half of the subjects, followed by depressive disorder in 38%, and less frequently, anxiety depressive disorder and addictions.
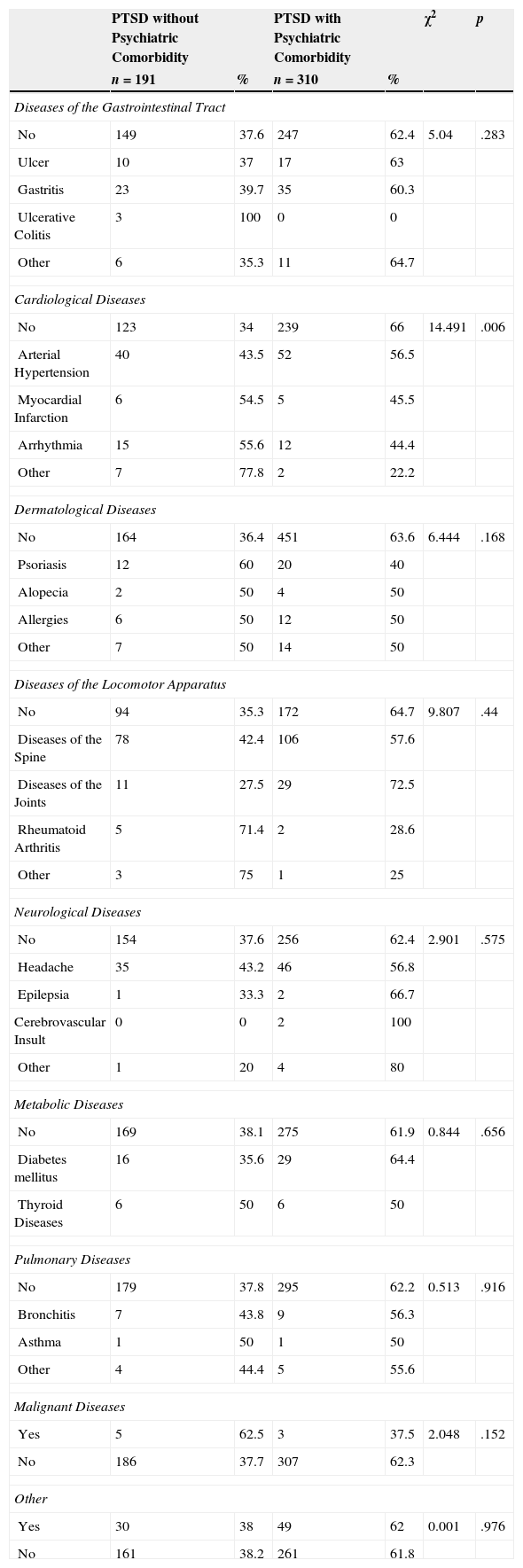
Differences in the sociodemographic indices and physical illnesses in combat veterans, with and without psychiatric comorbiditySociodemographic data were similar between the two groups. However, veterans with psychiatric comorbidities spent a significantly longer period of time on the battlefield than veterans without comorbidities (χ2 (3)=12.44; p=.006). Significantly more frequent cardiovascular diseases (hypertension and myocardial infarction) occurred in veterans without comorbidities (χ2 (4)=14.49; p=.006), while arrhythmias were somewhat more frequent in veterans with comorbidities (Table 6). There were no significant differences in the incidence of other diseases between veterans with or without psychiatric comorbidities.
Differences in morbidity from physical diseases in veterans suffering from PTSD with and without psychiatric comorbidity.
| PTSD without Psychiatric Comorbidity | PTSD with Psychiatric Comorbidity | χ2 | p | |||
|---|---|---|---|---|---|---|
| n=191 | % | n=310 | % | |||
| Diseases of the Gastrointestinal Tract | ||||||
| No | 149 | 37.6 | 247 | 62.4 | 5.04 | .283 |
| Ulcer | 10 | 37 | 17 | 63 | ||
| Gastritis | 23 | 39.7 | 35 | 60.3 | ||
| Ulcerative Colitis | 3 | 100 | 0 | 0 | ||
| Other | 6 | 35.3 | 11 | 64.7 | ||
| Cardiological Diseases | ||||||
| No | 123 | 34 | 239 | 66 | 14.491 | .006 |
| Arterial Hypertension | 40 | 43.5 | 52 | 56.5 | ||
| Myocardial Infarction | 6 | 54.5 | 5 | 45.5 | ||
| Arrhythmia | 15 | 55.6 | 12 | 44.4 | ||
| Other | 7 | 77.8 | 2 | 22.2 | ||
| Dermatological Diseases | ||||||
| No | 164 | 36.4 | 451 | 63.6 | 6.444 | .168 |
| Psoriasis | 12 | 60 | 20 | 40 | ||
| Alopecia | 2 | 50 | 4 | 50 | ||
| Allergies | 6 | 50 | 12 | 50 | ||
| Other | 7 | 50 | 14 | 50 | ||
| Diseases of the Locomotor Apparatus | ||||||
| No | 94 | 35.3 | 172 | 64.7 | 9.807 | .44 |
| Diseases of the Spine | 78 | 42.4 | 106 | 57.6 | ||
| Diseases of the Joints | 11 | 27.5 | 29 | 72.5 | ||
| Rheumatoid Arthritis | 5 | 71.4 | 2 | 28.6 | ||
| Other | 3 | 75 | 1 | 25 | ||
| Neurological Diseases | ||||||
| No | 154 | 37.6 | 256 | 62.4 | 2.901 | .575 |
| Headache | 35 | 43.2 | 46 | 56.8 | ||
| Epilepsia | 1 | 33.3 | 2 | 66.7 | ||
| Cerebrovascular Insult | 0 | 0 | 2 | 100 | ||
| Other | 1 | 20 | 4 | 80 | ||
| Metabolic Diseases | ||||||
| No | 169 | 38.1 | 275 | 61.9 | 0.844 | .656 |
| Diabetes mellitus | 16 | 35.6 | 29 | 64.4 | ||
| Thyroid Diseases | 6 | 50 | 6 | 50 | ||
| Pulmonary Diseases | ||||||
| No | 179 | 37.8 | 295 | 62.2 | 0.513 | .916 |
| Bronchitis | 7 | 43.8 | 9 | 56.3 | ||
| Asthma | 1 | 50 | 1 | 50 | ||
| Other | 4 | 44.4 | 5 | 55.6 | ||
| Malignant Diseases | ||||||
| Yes | 5 | 62.5 | 3 | 37.5 | 2.048 | .152 |
| No | 186 | 37.7 | 307 | 62.3 | ||
| Other | ||||||
| Yes | 30 | 38 | 49 | 62 | 0.001 | .976 |
| No | 161 | 38.2 | 261 | 61.8 | ||
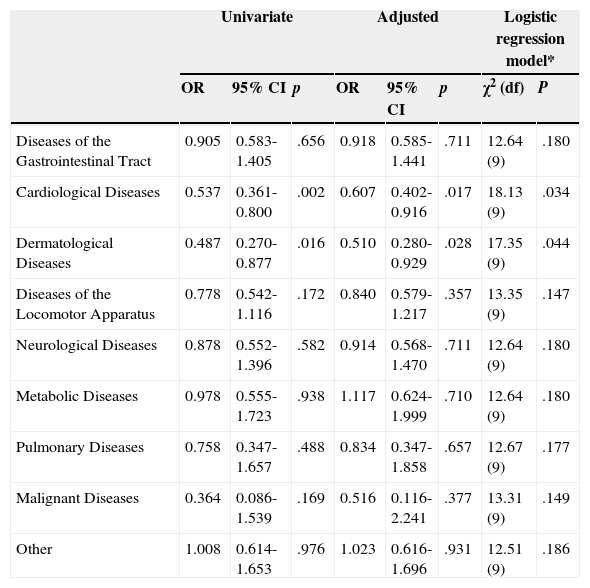
As presented in Table 7, PTSD patients with psychiatric comorbidity were statistically significantly less likely to be diagnosed with cardiological (odds ratio 0.537; 0.361-0.800; p=.002) and dermatological (odds ratio 0.487; 0.270-0.877; p=.016) diseases, in comparison with PTSD patients without psychiatric comorbidity, even after the adjustment for confounding sociodemographic variables (Table 7).
Odds ratio for specific diseases in PTSD patients with psychiatric comorbidity compared to PTSD patients without psychiatric comorbidity, in univariate and multiple logistic regression models (N=501).
| Univariate | Adjusted | Logistic regression model* | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | χ2 (df) | P | |
| Diseases of the Gastrointestinal Tract | 0.905 | 0.583-1.405 | .656 | 0.918 | 0.585-1.441 | .711 | 12.64 (9) | .180 |
| Cardiological Diseases | 0.537 | 0.361-0.800 | .002 | 0.607 | 0.402-0.916 | .017 | 18.13 (9) | .034 |
| Dermatological Diseases | 0.487 | 0.270-0.877 | .016 | 0.510 | 0.280-0.929 | .028 | 17.35 (9) | .044 |
| Diseases of the Locomotor Apparatus | 0.778 | 0.542-1.116 | .172 | 0.840 | 0.579-1.217 | .357 | 13.35 (9) | .147 |
| Neurological Diseases | 0.878 | 0.552-1.396 | .582 | 0.914 | 0.568-1.470 | .711 | 12.64 (9) | .180 |
| Metabolic Diseases | 0.978 | 0.555-1.723 | .938 | 1.117 | 0.624-1.999 | .710 | 12.64 (9) | .180 |
| Pulmonary Diseases | 0.758 | 0.347-1.657 | .488 | 0.834 | 0.347-1.858 | .657 | 12.67 (9) | .177 |
| Malignant Diseases | 0.364 | 0.086-1.539 | .169 | 0.516 | 0.116-2.241 | .377 | 13.31 (9) | .149 |
| Other | 1.008 | 0.614-1.653 | .976 | 1.023 | 0.616-1.696 | .931 | 12.51 (9) | .186 |
Note. *Including the specific diagnosis and confounding variables age, education, marital status and employment. CI=95% confidence intervals; OR=odds ratio for negative change; Univariate=univariate binary logistic regression; Adjusted=adjusted or multivariate binary logistic regression controlling for age, education, marital status and employment status.
The results of this case-control study indicate that combat veterans suffer more often from physical comorbidities, i.e., cardiovascular, dermatological, musculoskeletal, pulmonary and metabolic diseases, than the corresponding control group who was not exposed to combat traumatic experiences in the battlefield. These differences remain even after controlling the possible impact of socidemographic characteristics. PTSD patients were almost 4 times more likely to be diagnosed with neurological diseases, two times more likely to be diagnosed with diseases of the locomotor apparatus and dermatological diseases, odds ratio for metabolic and cardiological diseases were somewhat smaller, but still statistically significant after the adjustment.
The predictors of illnesses were age, length of time spent on the battlefield for veterans with cardiovascular, musculoskeletal, neurological and pulmonary diseases, and having been wounded for the occurrence of cardiovascular, musculoskeletal and malignant diseases. Veterans with PTSD complicated with other psychiatric comorbidities most often spent a long period on the battlefield, but suffered less often from all cardiovascular diseases, except arrhythmias.
These results indicate a far greater tendency among combat veterans to suffer from the majority of somatic diseases (Beckham et al., 2003; O’Toole & Catts, 2008; Qureshi et al., 2009). It seems that PTSD more often influences on veterans to suffer from physical illnesses than the length of time being exposed to combat trauma. In fact, the meta-analysis of PTSD in the general population demonstrated that the majority of studies found a greater incidence of arthritis, while the data on the incidence of coronary disease, diabetes and stroke are inconsistent (Qureshi et al., 2009). In contrast to our study where we compared veterans suffered from PTSD with control group that was not exposed to combat experience, in these studies comorbid physical disorders were evaluated between veterans with or without PTSD (O’Toole & Catts, 2008; Vasterling et al., 2008), indicating that exposure to trauma might have affected physical health, regardless of the PTSD diagnosis.
Although ulcerative colitis was recorded in three veterans with PTSD, but not in control subjects, a surprising finding from our study was that ulcer disease occurred more often in general population, while gastritis was more common among veterans. This observation is in contrast with data from Fink (2011), suggesting the greater significance of stress in the incidence of functional disorders than for ulcer disease.
In line with increased ECG abnormalities (Boscarino, 2004), we have found the higher incidences of myocardial infarction and cardiac arrhythmia in veterans, indicating the significant impact of traumatic experiences as well as PTSD diagnosis on coronary cardiac diseases. These disorders might also be associated with disturbances in the hypothalamic-pituitary adrenal (HPA) and the sympathetic-adrenal-medullary (SAM) stress axes occurring in PTSD, that result in consequent increases in circulating catecholamines and diminished levels of cortisol (Radley et al., 2011). Exposure to stress also leads to suppression of lymphocyte function, impaired proliferation of T lymphocytes and NK-cell activity, which are all associated with impaired immune response (Raison, Capuron, & Miller, 2006). In our study veterans had more dermatological diseases than control subjects. This might be explained by the altered inflammation responsiveness and aberrant allergic mechanisms, that are associated with the significantly larger number of patients with alopecia, allergic reactions and other skin diseases (eczema, dermatitis) (Gupta & Gupta, 2012). We observed a higher incidence of psoriasis in the general population than in PTSD veterans, a finding in contrast with data obtained from U.S. veterans (Boscarino, 2004). The explanation for this finding is at present unclear. Impaired immune response is related to an increased incidence of diseases of the musculoskeletal system and joints, rheumatoid arthritis and back problems, which is consistent with findings from our and other (Boscarino, Forsberg, & Goldberg, 2010; O’Toole & Catts, 2008) studies. The possible disturbances of the immune system were presumably associated with more frequent findings of asthma and other pulmonary diseases among veterans with PTSD compared to control subjects (Boscarino, 2004).
The greater incidence of all the neurological diseases, including headaches, could be associated with tension headaches, frequently within the framework of somatization in PTSD (Ginzburg et al., 2010). Although our study included only a small number of patients with epilepsy (EPI) and cerebrovascular insult (CVI), significantly higher incidence of CVI in veterans may be associated with atherosclerotic events that lead to coronary cardiac diseases. The reason for higher incidence may be a lifestyle (smoking eg), but unfortunately we have not explored in the study.
Consistent with recent findings of the increased incidence of diabetes in patients suffering from PTSD (Boyko et al., 2010), and disruptions in thyroid hormone levels, associated with disturbances of the hypothalamus-pituitary-thyroid (HPT) axis in subjects with civilian PTSD (Glaesmer et al., 2011; Olff, Güzelcan, de Vries, Assies, & Gersons, 2006), metabolic diseases (i.e. diabetes mellitus and diseases of the thyroid gland) were significantly more common among the veterans with PTSD than in control group.
The results suggesting that age was a predictor of morbidity in both groups were expected. The severity of morbidity was predicted by the length of time spent on the battlefield and being wounded, emphasizing the importance of the intensity and duration of the exposure to traumatic experience for the occurrence of physical illness. Employment status was a predictor of morbidity in control group, presumably due to the workplace stress, associated with the adverse working conditions in developing countries (Kortum, Leka, & Cox, 2010).
The high percentage of psychiatric comorbidity with PTSD and the large proportion of patients with Enduring Personality Change After Catastrophic Experience (EPCACE) and anxiety-depressive disorder are findings consistent with previous reports (Ginzburg et al., 2010; Nemčić-Moro, Frančišković, Britvić, Klarić, & Zečević, 2011), however our and other (McTeague et al., 2010) studies underscored the significance of the duration of trauma exposure on the occurrence of psychiatric comorbidities. The reason why veterans with PTSD complicated with various psychiatric comorbidities suffer less frequently from all cardiovascular diseases, except arrhythmia, and also dermatological diseases is unclear, but might be due to the process of psychiatric diagnosis and clinical evaluation of psychiatric comorbidity that may relieve anxiety, which consequently reduces the risk for other diseases. This finding remains unclear and requires further investigations.
The explanation for our findings of the increased morbidity from physical as well as psychiatric disorders may be sought in the current understanding of the neurobiology of response to traumatic experience, and its impact on the occurrence of depression and physical illnesses. The influence of trauma leads to abnormal, excessive activation of the HPA axis and inflammatory pathways. Activation of macrophages due to inflammatory challenges (infection, tissue damage or destruction) may cause the release of proinflammatory cytokines. These cytokines enter several areas of the afferent sensory systems and can lead to increased activity. Once in the brain, cytokines can cause altered metabolism of serotonin (5-HT) and dopamine (DA), activation of corticotrophin-releasing hormone (CRH) leading to increased serum cortisol levels, and disruption of synaptic plasticity through changes in growth factors such as brain-derived neurotrophic factor (BDNF) (Raison et al., 2006). These cellular disturbances might be correlated with disorders in the immune response, which reflects stress at both the psychological and physical levels. In patients with chronic PTSD, low cortisol levels and high HPA sensitivity are usually found (Yehuda, 1997). Unfortunately, these explanations are only speculations because indicators (cortisol, inflammatory cytokines) were not measured.
This study has some limitations: experimental group was studied 15 years after the end of the war. Presumably, because of that reason, about half of the veterans from this group, with PTSD diagnosis, also suffer from Enduring Personality Change After Catastrophic Experience (EPCACE). Due to afore mentioned, it can be supposed that these veterans suffer from more difficult form of PTSD, and as such they are not adequate representatives of the total veteran population from this area. Therefore, this group of veterans consisted of the most severely ill patients who required years of treatment. In addition, the use of hospital and clinic samples, as in the current study, is potentially open to Berkson's bias. Since the group of veterans was not evaluated for possible other kind of traumatic experience besides war induced trauma, we realized that any other trauma during lifetime can also affect the appearance of symptoms. Unfortunately, this has not been studied (Guerra, Cumsille, & Martinez, 2014). On the other hand, although the control group was formed from members of the general population who did not fought in the war; these subjects were also exposed to the stressful experience of living under wartime conditions, although the degree of their traumatization was certainly far lower. Also, it should be considered that most veterans did not work, opposed to the control group, which also may represent an additional stressor factor. Another limitation might be that psychiatrists did not examine each member of the control group, in order to rule out the diagnosis of PTSD. Smoking and body mass index (as well as physical training), pre-war medical history or health behavior were not evaluated, as these factors may also contribute to a higher incidence of physical illness, which is also a shortcoming of the study. Future research should focus on all veterans with PTSD, veterans without PTSD and corresponding control subjects from the general population, using objective laboratory and clinical measures.
In conclusion, 501 veterans with PTSD suffered more often from cardiovascular, dermatological, musculoskeletal, pulmonary and metabolic diseases than 825 corresponding control subjects who were not exposed to combat experience. The predictors of cardiovascular, musculoskeletal and malignant diseases in veterans were age, length of time spent in combat, and having been wounded. A longer period in the combat zone was associated with arrhythmias in veterans with PTSD complicated with other psychiatric comorbidities. PTSD as a result of exposure to war trauma increases the likelihood of developing somatic diseases.
FundingThis research was supported by Project 141-0000000-0068 of the Croatian Ministry of Science, Education and Sports.
Available online 25 December 2014