Eosinophilic gastritis (EG) is an uncommon disease that may manifest itself with dyspeptic symptoms, nausea, vomiting and epigastric pain. At onset, digestive hemorrhage is atypical. The incidence of EG has increased in the past few years. The infiltration of eosinophils can affect any part of the digestive tract. The presence of at least 15 eosinophils per high-power field (HPF) is essential for diagnosis. Here, we present a patient with recurrent epigastric pain that started with severe upper gastrointestinal bleeding due to EG.
Our patient, a 15-year-old female, had been studied since she was 9 years old due to a recurrent abdominal pain and severe anemia. Prior tests included the results of 6 gastroscopies with biopsies and 1 colonoscopy. They showed chronic gastritis, a nodular pattern in the gastric antrum, and infection by Helicobacter pylori, which was later treated and eradicated. Only one gastric biopsy showed an increase in eosinophils, no specific treatment was carried out. Furthermore, the colonoscopy results presented were normal. Additional studies for coeliac disease were tested and the results came negative (antitransglutaminase antibodies, HLA DQ2 DQ8 and normal duodenal biopsies).
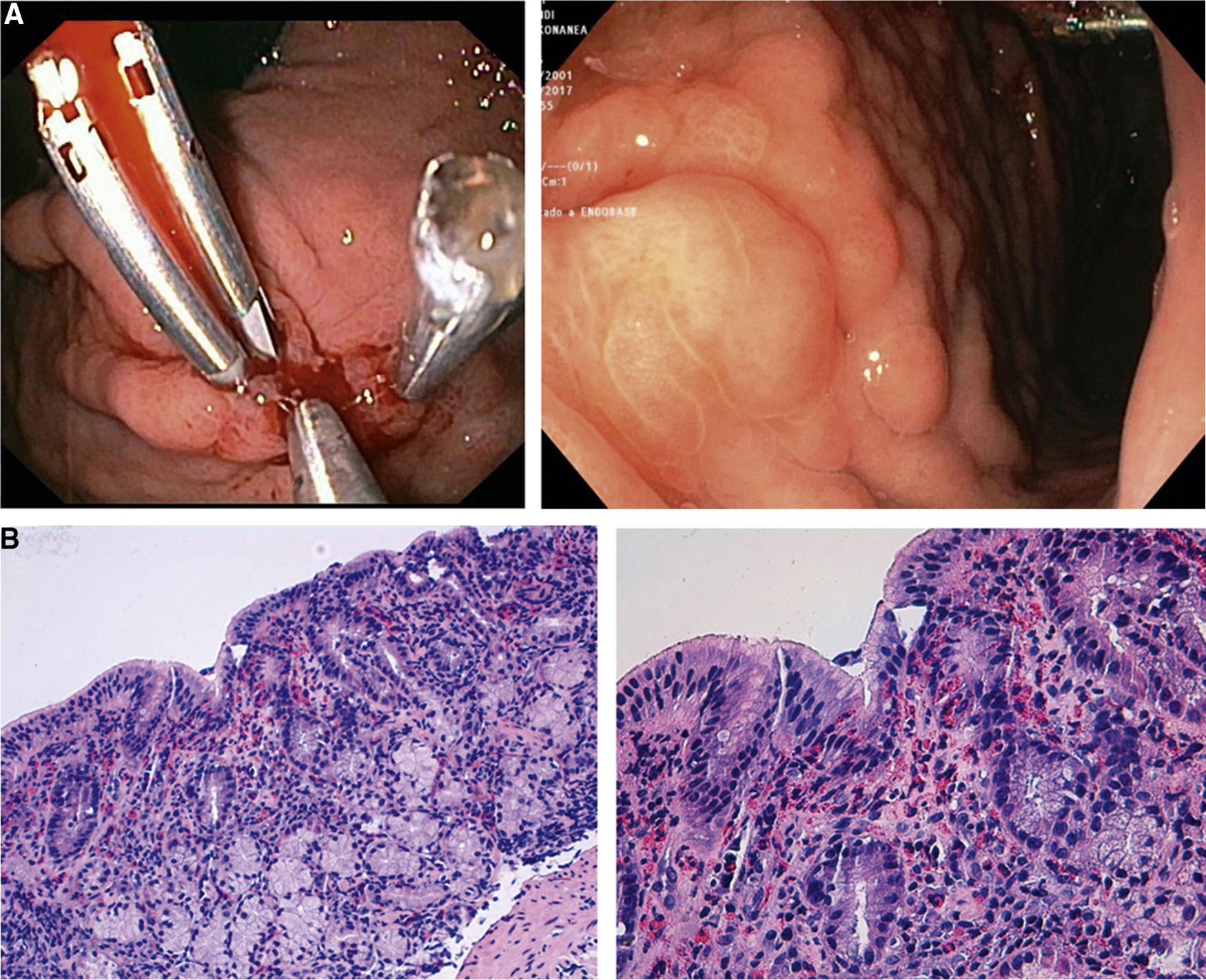
At 14 she was hospitalized due to dizziness and hematemesis. Laboratory tests showed a normocytic-hypochromic anemia (hemoglobin 6.7g/dl and hematocrit 21%). Metabolic profile, lipase, and clotting test were normal. She was treated with proton pump inhibitors (PPIs), intravenous iron and blood transfusions. A gastroscopy was performed and red blood remains were found with an ulcer Forrest IIA in the gastric body. She was then treated with adrenaline, ethoxy-sclerol and hemostatic clips.
After 6 days, another gastroscopy was performed. The results revealed a nodular pattern in the fundus and gastric body (Fig. 1A). Biopsies were taken and a chronic inflammatory infiltrate was observed. No other pathology was seen. The rapid urease test for H. pylori was repeated and came out negative.
Laboratory findings were repeated 3 months later and showed hemoblobin values of 12.8g/dL, a hematocrit of 38.7%, no peripheral blood eosinophilia, pepsinogen of 74ng/ml, gastrin of 68.8pg/ml, Calprotectin of 11mg/kg, negative antinuclear antibodies and stool culture. Studies of food allergies were positive on nuts, skin and blood.
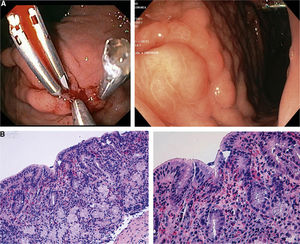
A gastroscopy was repeated one year later. It showed the previously observed nodular pattern. The biopsies of the gastric fundus and body showed an acute marked eosinophilia in the lamina propria and muscularis mucosa. The eosinophile count was of 40 HPF (Fig. 1B).
After the tests, she was treated with ranitidine 300mg/day, ebastine 10mg/day and a diet free of nuts. No abdominal pain, anemia, or recurrence of bleeding were observed in the following 18 months. A control gastroscopy was performed that showed a marked improvement in eosinophile infiltrate (count below 10 eosinophils).
The incidence of EG is estimated as 1–30/100,000. The most common symptom is abdominal pain. Other “severe” signs, such as digestive hemorrhage, is uncommon. Three similar cases have been reported.1,2 It should be noted that our case is the only one that presented an episode of severe bleeding with hemodynamic repercussion. When the gastroscopy was performed, our patient had blood in the stomach and an ulcer. The entire colon was checked, no other lesions were found and a test of eosinophilia in peripheral blood came out negative.
The suspicion of the disease becomes essential in its diagnosis. Our patient required more than 4 years and 10 gastroscopies before diagnosed. Multiple gastric biopsies should be taken and the pathologist should be aware about EG. Apparently EG is not as uncommon as previously thought and missed diagnosis are high.3,4
Although eosinophilia or leukocytosis are usually found,4 they are not essential for the diagnosis of EG. In our case eosinophil count was normal. The most common endoscopic presentation is mucosal edema and hyperemia, followed by mucosal erosion and hemorrhage. Our patient presented erythema, erosions, lymphonodular hyperplasia and granular mucosal changes at the antrum, fundus, and pyloric regions.
The treatment is based on diet control and systemic or enteral administration of corticosteroids. Other therapies as histamine blockers, mast cell stabilizers, or leukotriene inhibitors can also be used. Current therapies include monoclonal antibody against IgE and IL-5. In this case, the treatment with diet, oral antihistamines and anti-H2, the patient became asymptomatic.
In summary, when a patient presents peptic ulcer not related to H. pylori or non-steroidal anti-inflammatory drug use, the presence of EG disease should be considered and biopsies should be performed for the diagnosis.