To assess if seven demographic variables (age, gender, religion, ethnicity, income, educational level, and political views) are predictive of Covid-19 vaccine hesitancy.
Material and methods327 participants completed a survey asking questions regarding each of the variables.
ResultsAge, gender and political views have no statistically significant correlation with vaccine hesitancy. Ethnicity and religion are predictive of vaccine hesitancy. Income has a weak negative correlation with Covid-19 vaccine hesitancy, and educational level has a moderate negative correlation with Covid-19 vaccine hesitancy.
ConclusionIn order to curb Covid-19 vaccine hesitancy, public health authorities in Venezuela need to focus efforts on marginalized ethnic groups, Protestants, and those with lower levels of education.
Evaluar si 7 variables demográficas (edad, género, religión, origen étnico, ingresos, nivel educativo y opiniones políticas) son predictivas del rechazo a la vacuna del Covid-19.
Material y métodosTrescientos veintisiete participantes completaron una encuesta con preguntas sobre cada una de las variables.
ResultadosLa edad, el género y las opiniones políticas no tienen una correlación estadísticamente significativa con el rechazo a la vacuna. El origen étnico y la religión predicen el rechazo a las vacunas. Los ingresos tienen una correlación negativa débil con el rechazo de la vacuna Covid-19, y el nivel educativo tiene una correlación negativa moderada con el rechazo de la vacuna Covid-19.
ConclusiónPara frenar el rechazo a la vacuna del Covid-19, las autoridades de salud pública en Venezuela deben concentrar sus esfuerzos en los grupos étnicos marginados, los protestantes y aquellos con niveles más bajos de educación.
As a result of what some authors have called a “humanitarian crisis”,1 Venezuela's healthcare system has been on the border of collapse for the past five years. In this context, the nation was ill-prepared to manage the Covid-19 pandemic.
Due to economic sanctions (imposed by the United States and the European Union), Venezuela has encountered additional difficulties in receiving vaccines. A vaccination programme has begun, but it is still slow in achieving its goals.2 As in many other countries, one difficulty in the vaccination campaign has been vaccine hesitancy. Public health officials need to have a good understanding of what sectors of the population are at greater risk in vaccine hesitancy, so as to focus informative campaign efforts on the most hesitant. Consequently, the present study assesses whether seven demographic variables (age, gender, religion, ethnicity, income, education and political views) are predictive of Covid-19 vaccine hesitancy in Venezuela.
Materials and methodsDue to restraints due to Covid-19 lockdowns, this study had to work with non-probabilistic sampling. 327 participants were recruited on the basis of availability and willingness to answer a survey. Recruitment took place in two malls and two public parks in Maracaibo, during the period between February and May 2021.
The survey asked participants their age, gender, religion, ethnicity, household income per capita, years of schooling, whether or not they support the government, and whether or not they have received or intend to receive the Covid-19 vaccine when available.
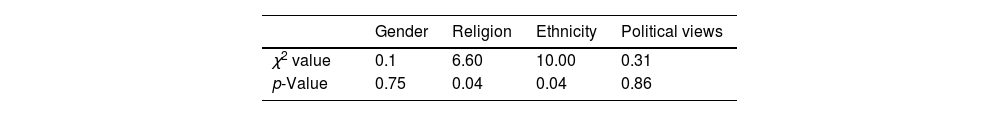
Chi-square coefficients were calculated to determine if vaccine hesitancy has a statistical correlation with the following nominal variables: gender, religion, ethnicity, and opposition/support for the government.
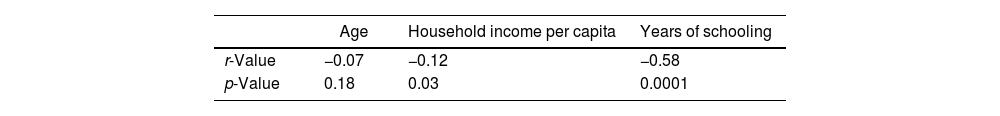
Given that in this study vaccine hesitancy is a dichotomous variable (i.e., only two values are possible), conventional correlation coefficients were not calculated. Instead, point biserial coefficients (used for at least one dichotomous variable) were calculated to determine if there is a correlation between vaccine hesitancy and the following quantitative variables: age, household income per capita, years of schooling.
Statistical significance was placed at p<0.05.
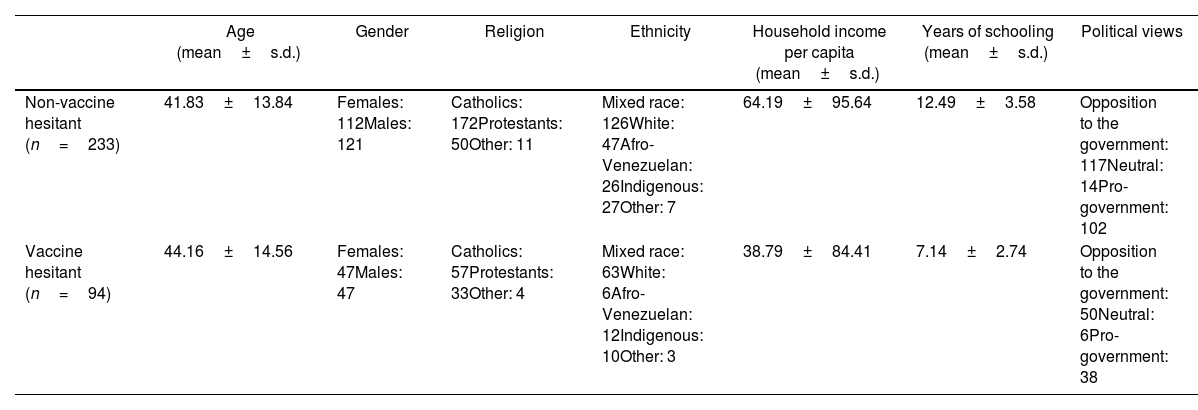
ResultsDescriptive statistics are presented in Table 1. In the present sample, 28.75% are vaccine hesitant.
Descriptive statistics.
| Age (mean±s.d.) | Gender | Religion | Ethnicity | Household income per capita (mean±s.d.) | Years of schooling (mean±s.d.) | Political views | |
|---|---|---|---|---|---|---|---|
| Non-vaccine hesitant (n=233) | 41.83±13.84 | Females: 112Males: 121 | Catholics: 172Protestants: 50Other: 11 | Mixed race: 126White: 47Afro-Venezuelan: 26Indigenous: 27Other: 7 | 64.19±95.64 | 12.49±3.58 | Opposition to the government: 117Neutral: 14Pro-government: 102 |
| Vaccine hesitant (n=94) | 44.16±14.56 | Females: 47Males: 47 | Catholics: 57Protestants: 33Other: 4 | Mixed race: 63White: 6Afro-Venezuelan: 12Indigenous: 10Other: 3 | 38.79±84.41 | 7.14±2.74 | Opposition to the government: 50Neutral: 6Pro-government: 38 |
Chi square analyses are presented in Table 2.
Table 3 presents point biserial correlations.
DiscussionAlthough Venezuela has had intense political polarization over the last 20 years, opposition or support for the government do not correlate with hesitancy to receive the Covid-19 vaccine. At first sight, in a nation with deep political divisions, it may be expected that those disapproving of the government would be more hesitant to receive vaccines (since the government is in charge of distributing them), and those who sympathize with the government would be more receptive. In other contexts, political ideologies do influence vaccine hesitancy.3 Yet, results from this study indicate that such hypothesis must be rejected.
By contrast, ethnicity is a predictive factor of vaccine hesitancy, with whites being the least likely to be vaccine hesitant (11.32%), followed by indigenous (27.02%), other (30%), Afro-Venezuelan (31.57%), and Mixed Race (33.33%). Venezuela still struggles with racism and ethnic discrimination, and historically whites have been the dominant group. Prior research has consistently shown that in various countries, marginalized ethnic minorities are at greater risk for vaccine hesitancy,4 including the Covid-19 vaccine.5 In the present study, that pattern is repeated. One possible cofounding variable is acceptance of conspiracy theories. Given their greater mistrust of the societal system at large because of discrimination, ethnic minorities are more likely to accept conspiracy theories,6 and consequently, have greater levels of vaccine hesitancy.
Religion also comes out as a predictor of vaccine hesitancy, with Protestants having the greatest level of vaccine hesitancy (39.76%), followed by other (26.66%) and Catholic (24.89%). Prior research in other contexts has shown that very conservative religious groups are more prone to be vaccine hesitant.7 In the case of Venezuela, the fact that most Protestant denominations are evangelical is relevant in this regard. Evangelical groups have traditionally manifested greater levels of anti-scientific thinking8 (especially rooted in opposition to the theory of evolution, as it is perceived to run counter to the tenets of Christianity), and consequently, anti-science attitudes might account for greater vaccine hesitancy,9 inasmuch as vaccines are promoted by the scientific establishment.
Results come out showing that age has no correlation with vaccine hesitancy. Household per capita income only has a weak negative correlation with vaccine hesitancy. However, years of schooling does have a moderate negative correlation with vaccine hesitancy. This finding coheres with extensive research that so far has proven that one big factor in vaccine hesitancy is low educational level.10 Naturally, as subjects have greater exposure to education, they are more apt in understanding how vaccines work, and the high risks of not getting vaccines.11
ConclusionsResults from this study suggest that authorities in Venezuela have reason to be concerned about Covid-19 vaccine hesitancy. Those with lesser education, and traditionally marginalized ethnic groups, are at greater risk for vaccine hesitancy. Protestants are also less likely to be receptive of vaccination. Vaccination campaigns in Venezuela need to focus efforts in persuading members of these groups to receive the Covid-19 vaccine. In the longer term, authorities also need to work towards greater inclusion of traditionally marginalized ethnic groups, and expand educational efforts towards the population at large, as the results from the present study suggest that this may reduce vaccine hesitancy. Likewise, public health authorities need to engage Protestant communities in order to promote greater acceptance of scientific thinking, as results from this study also suggest that these policies may also curb vaccine hesitancy.
Conflict of interestThe author declares no conflict of interest.