With the surge of COVID-19 cases worldwide, vaccines against COVID-19 are also developing across the countries. However, the acceptability of COVID-19 vaccination among general people is questionable. The availability of several vaccines’ options against COVID-19 has perplexed people regarding individual vaccines’ efficacy and safety. Therefore, we aim to determine the acceptance, preferences, impact factors of future COVID-19 vaccines in Malaysia and the factors influencing the COVID-19 vaccination acceptance among vaccine demand and vaccine delay groups.
Material and methodsAn online-based cross-sectional survey was conducted among Malaysian residents 18 years and above of either gender using the snowball sampling technique. A self-administered questionnaire was made available to participants through various social media networks, email, and telegram. The data obtained from the survey were analyzed using SPSS version 25.0. Association between background characteristics and respondents were analyzed using the Chi-square test in the vaccine delay group and vaccine acceptance group.
ResultsTotal of 1282 responses were considered for the study, mainly from male respondents (71%). Among the respondents, 95.9% thought that vaccination would be an effective way to prevent and control COVID-19, and 96% would accept vaccination if the COVID-19 vaccine were successfully developed and approved for listing in the future. Essential factors influencing vaccination decisions were vaccine convenience (95.7%) and doctor's recommendation (97.3%). Bivariate analysis revealed that age less than 24 years, Malay race, living in urban areas, tertiary education, students, single marital status, family income (Malaysian ringgits) RM 4,850 to RM 10,959 and >RM 10,960 were significantly associated with vaccine acceptance of COVID19 vaccination.
ConclusionAll the factors influencing COVID-19 vaccine acceptance rates throughout the country should be studied on a larger scale, and appropriate steps to ensure vaccine acceptance among the public should be meticulously devised by the government and related authorities.
Con el aumento de casos de COVID-19 en todo el mundo, las vacunas contra la COVID-19 también están en desarrollo en todos los países. Sin embargo, la aceptabilidad de la vacuna COVID-19 entre la gente en general es cuestionable. La disponibilidad de varias opciones de vacunas contra COVID-19 ha dejado perpleja a la gente con respecto a la eficacia y seguridad de las vacunas individuales. Por lo tanto, tenemos como objetivo determinar la aceptación, las preferencias y los factores de impacto de las futuras vacunas COVID-19 en Malasia y los factores que influyen en la aceptación de la vacunación COVID-19 entre la demanda de vacunas y los grupos de demora de la vacuna.
Material y métodosSe realizó una encuesta transversal en línea entre residentes de Malasia de 18 años o más de cualquier género utilizando la técnica de muestreo de bola de nieve. Se puso a disposición de los participantes un cuestionario autoadministrado a través de varias redes sociales, correo electrónico y telegrama. Los datos obtenidos de la encuesta se analizaron con el programa SPSS versión 25.0. La asociación entre las características de fondo y los encuestados fueron analizados usando la prueba de χ2 en el grupo de demora de la vacuna y el grupo de aceptación de la vacuna.
ResultadosSe consideró un total de 1.282 respuestas para el estudio, principalmente de hombres encuestados (71%). Entre los encuestados, el 95,9% pensó que la vacunación sería una forma eficaz de prevenir y controlar la COVID-19, y el 96% aceptaría la vacunación si la vacuna COVID-19 se desarrollara con éxito y se aprobara para su inclusión en el futuro. Factores esenciales que influyeron en las decisiones de vacunación fueron la conveniencia de la vacuna (95,7%) y la recomendación del médico (97,3%). El análisis bivariado reveló que la edad < 24 años, la raza malaya, la vida en áreas urbanas, educación terciaria, estudiantes, estado civil soltero, ingresos familiares RM 4,850 a RM 10,959 y > RM 10,960 (en ringgits, moneda malaya), se asociaron significativamente con la aceptación de la vacuna COVID-19.
ConclusiónTodos los factores que influyen en las tasas de aceptación de la vacuna COVID-19 en todo el país deben estudiarse a mayor escala, y el gobierno y las autoridades relacionadas deben diseñar meticulosamente los pasos apropiados para asegurar la aceptación de la vacuna entre el público.
The coronavirus disease (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has wreaked havoc worldwide, especially in Southeast Asia.1–3 Food and Drug Administration (FDA) has approved some drugs to treat severe COVID-19 cases, there is no specific and effective therapy. Therefore, all countries are attempting to halt the disease from spreading by enforcing lockdowns and quarantines, community-wide use of facemasks at all hours, social distancing measures, and travel ban.4,5 Unfortunately, these initiatives have resulted in substantial physical and psychosocial deterioration of individuals,6 as well as a global economic recession.4,7 Therefore, designing and deploying a COVID-19 vaccine is one of the most cost-effective and successful approaches to fighting the pandemic.1,8,9
Various research institutes funded by governments, philanthropists, and pharmaceutical firms actively create and test the most effective COVID-19 vaccine.1 The first COVID-19 vaccine based on mRNA was developed and evaluated by Moderna Inc in the United States, and then CanSino Biologics in China tested a non-replicating vector-based vaccine.10 Other vaccine candidates are being developed, including inactivated,11 sub-unit,12 live attenuated,13 replicating viral vector-based vaccines,13 and DNA-based vaccines.10 Nevertheless, it is not clear how efficacious will these vaccines be. People can assume that the pandemic vaccine is dangerous due to its novelty or alleged lack of research.14 As a result, public understanding of COVID-19 vaccine safety may play a role in vaccine acceptance.15,16 Indonesian study reported, 52% of individuals are willing to get vaccinated against COVID-19; while 48% of the individuals would delay the vaccination until the vaccine's safety was verified.1
COVID-19 is one of the greatest human health crises globally, so community engagement and vaccine coverage are critical factors in overcoming this pandemic.17,18 However, the acceptability level of the Covid-19 vaccine is less well known, and there could be major differences in the rates of acceptance vaccine against COVID-19 concerning different populations.14 According to a global survey, it ranges from 55% (in Russia) to 89% (in China).19 Whereas study conducted in Malaysia showed 93% acceptance.20 Further, the most frequent reasons identified for vaccine refusal were vaccine safety,21 vaccine efficacy22 and vaccine side effects.20,23
With this background, the main aim of this research was to determine the acceptability level of the COVID-19 vaccine in Malaysia. The specific objectives were to determine the acceptance, preferences, impact factors of the future COVID-19 vaccine and determine the influencing factors of COVID-19 vaccination acceptance among the vaccine demand and vaccine delay groups. This research will help formulate the best approaches to implement potential vaccination policies in Malaysia and reduce factors affecting vaccine acceptance and immunization programmes.
Material and methodsStudy design and study settingAn internet-based cross-sectional survey was conducted from October 2020 to January 2021, when the movement restriction due to COVID-19 was active in Malaysia. Snowball sampling, a convenience sampling method, was used for the data collection using research networks of universities, hospitals, friends, and their relatives.
Ethical considerations, study population and study toolThe study received ethical approval from Asia Metropolitan University's Medical Research and Ethics Committee (Reference no. AMU/MREC/FOM/NF/2020/38). Malaysian residents of 18 years old and above and of either gender were selected and enrolled in the study. All the enrolled participants consented to the online survey.
The self-administered questionnaire was designed based on previous studies and frameworks to assess vaccine acceptance for newly emerging infectious diseases such as H1N1 or Ebola.7,8 The contents of the questionnaire included (1) socio-demographic characteristics such as age, gender, place of residence, race, educational level, occupation, number of family members, marital status and family income; (2) acceptance, attitude, vaccination preferences for future COVID-19 vaccination and the importance of identified impact factors on the respondents’ vaccination decision-making, such as vaccine price, convenience and doctor's recommendations. All questions were close-ended, with tick boxes provided for responses. The Cronbach's alpha of 0.812 indicated that the questionnaire has an excellent internal consistency.
Process of data collectionThe structured online questionnaires were conveniently distributed through emails, Facebook, WhatsApp, Telegram, Instagram, and other social media throughout this network in Malaysia. The online link for collecting data was available for about four months. Our study was entirely a voluntary online survey. The survey form was provided with a setting such that the consented participants could respond to questions only once using a single account to prevent more than one response from the same history. Spreadsheets of responses were exported into IBM SPSS version 25 for further analysis.
Data analysisThe data captured in the online google form were examined for any errors, cleaned and then exported into SPSS version 25.0 for further analysis. Descriptive statistics were used to summarize the respondent's socio-demographic. Chi-square test was used to analyze the significance of the association between background characteristics and respondents in the two groups (vaccine delay group vs vaccine acceptance group. A logistic regression model was employed on those variables that appeared to have a p-value of <0.05 in the bivariate analysis to identify determinants of participants’ acceptance of a COVID-19 vaccine. The significance of adjusted Odds Ratio (AOR) in multivariate analyses were assessed at α=0.05.
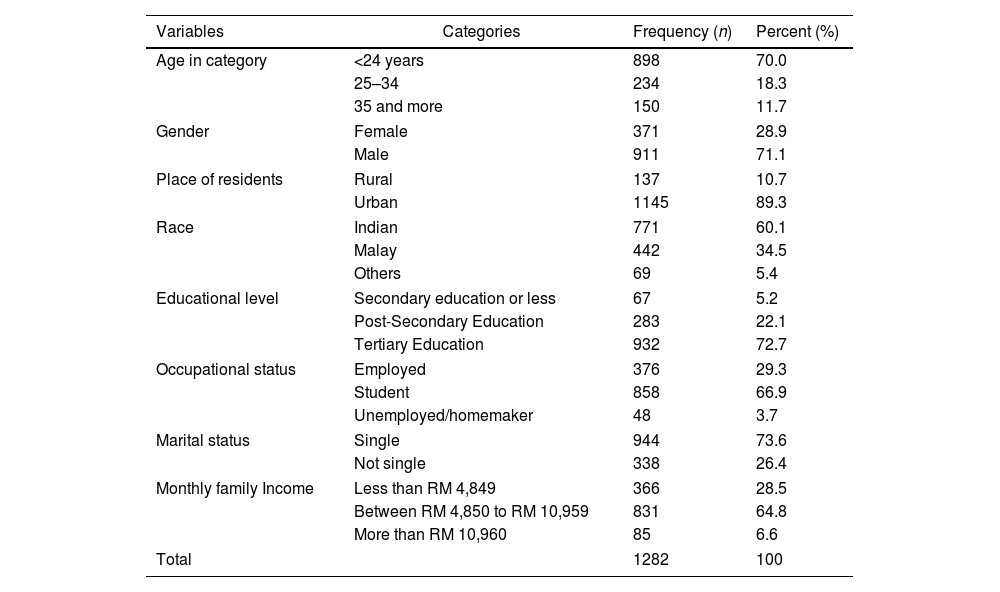
ResultsWe received 1310 responses (Response rate 97.8%) during the survey period; 28 were excluded because of failure in fulfilling the inclusion criteria and incomplete data. Table 1 presents the basic characteristics of respondents. Nearly 70% of the respondents were less than 24 years old, and 71% were male. Most (89%) were residents of the urban area, and around 60% of respondents were from the Indian ethnicity. Almost 73% were tertiary, and two-third of the respondents were students. About 73% of respondents were single, and most of the respondent's monthly incomes were between RM 4,850 to RM 10,959.
Socio-demographic characteristics respondents.
| Variables | Categories | Frequency (n) | Percent (%) |
|---|---|---|---|
| Age in category | <24 years | 898 | 70.0 |
| 25–34 | 234 | 18.3 | |
| 35 and more | 150 | 11.7 | |
| Gender | Female | 371 | 28.9 |
| Male | 911 | 71.1 | |
| Place of residents | Rural | 137 | 10.7 |
| Urban | 1145 | 89.3 | |
| Race | Indian | 771 | 60.1 |
| Malay | 442 | 34.5 | |
| Others | 69 | 5.4 | |
| Educational level | Secondary education or less | 67 | 5.2 |
| Post-Secondary Education | 283 | 22.1 | |
| Tertiary Education | 932 | 72.7 | |
| Occupational status | Employed | 376 | 29.3 |
| Student | 858 | 66.9 | |
| Unemployed/homemaker | 48 | 3.7 | |
| Marital status | Single | 944 | 73.6 |
| Not single | 338 | 26.4 | |
| Monthly family Income | Less than RM 4,849 | 366 | 28.5 |
| Between RM 4,850 to RM 10,959 | 831 | 64.8 | |
| More than RM 10,960 | 85 | 6.6 | |
| Total | 1282 | 100 | |
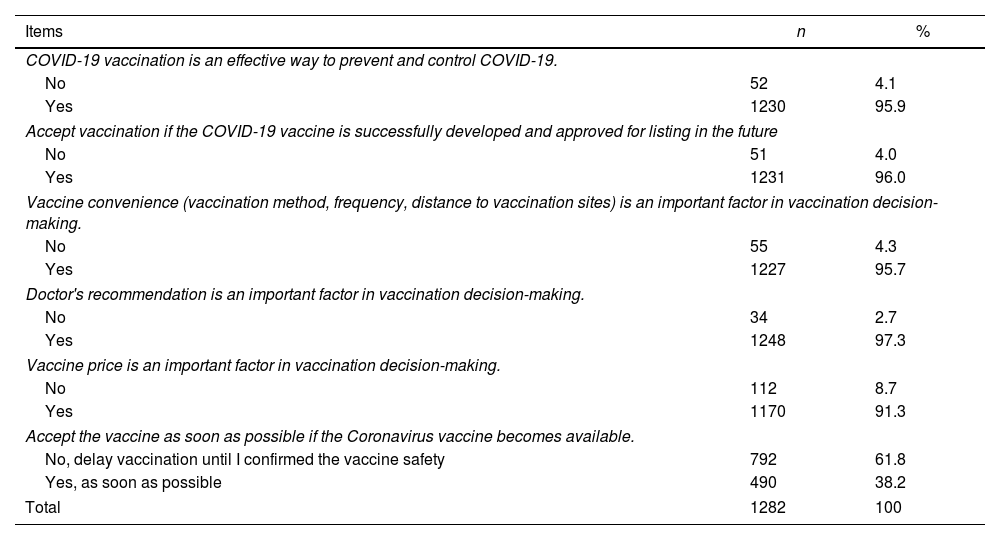
Table 2 shows the acceptance, preferences, and impact factors of the future COVID-19 vaccine. Of the 1282 respondents, 95.9% thought that vaccination would be an effective way to prevent and control COVID-19, and 96% would accept vaccination if the COVID-19 vaccine were successfully developed and approved for listing in the future. Regarding the significance of some vaccination decision-making factors, most considered were vaccine convenience (95.7%) and doctor's recommendation (97.3%), affecting their vaccination plan. Around 91% thought that the vaccine price was important. With the 1282 respondents in the vaccine accept group, only 38.2% wanted to get vaccinated as soon as possible when it becomes available, while 61.8% would hold vaccination until they could verify the safety of vaccine.
Acceptance, preferences, and impact factors of the future COVID-19 vaccine.
| Items | n | % |
|---|---|---|
| COVID-19 vaccination is an effective way to prevent and control COVID-19. | ||
| No | 52 | 4.1 |
| Yes | 1230 | 95.9 |
| Accept vaccination if the COVID-19 vaccine is successfully developed and approved for listing in the future | ||
| No | 51 | 4.0 |
| Yes | 1231 | 96.0 |
| Vaccine convenience (vaccination method, frequency, distance to vaccination sites) is an important factor in vaccination decision-making. | ||
| No | 55 | 4.3 |
| Yes | 1227 | 95.7 |
| Doctor's recommendation is an important factor in vaccination decision-making. | ||
| No | 34 | 2.7 |
| Yes | 1248 | 97.3 |
| Vaccine price is an important factor in vaccination decision-making. | ||
| No | 112 | 8.7 |
| Yes | 1170 | 91.3 |
| Accept the vaccine as soon as possible if the Coronavirus vaccine becomes available. | ||
| No, delay vaccination until I confirmed the vaccine safety | 792 | 61.8 |
| Yes, as soon as possible | 490 | 38.2 |
| Total | 1282 | 100 |
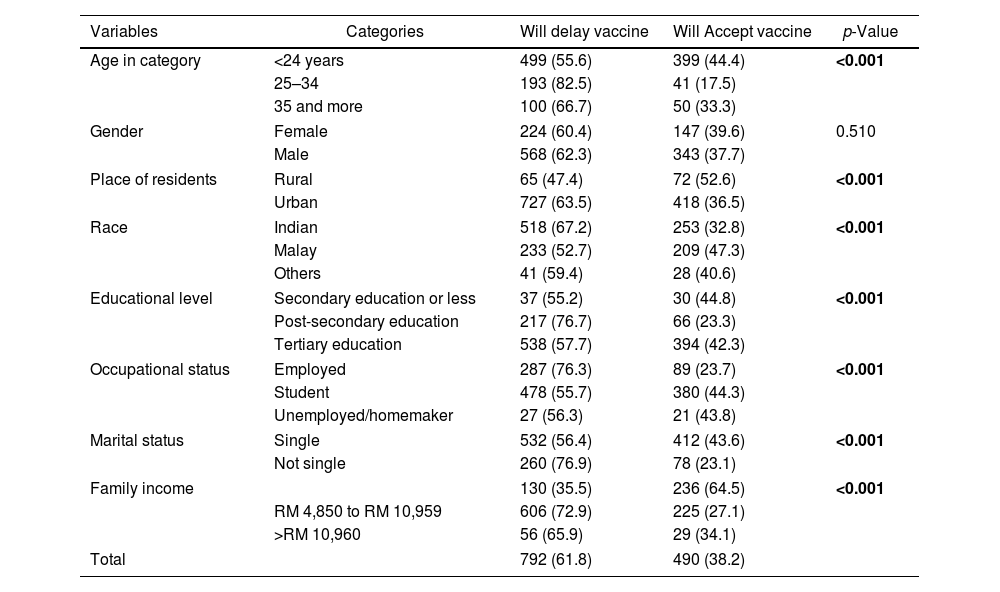
Table 3 exhibits the comparison between delay and acceptance of the future COVID-19 vaccine among 1282 Malaysian residents. Among them, 792 respondents reported they would delay the vaccination, while 490 will accept vaccination and get vaccinated as soon as possible when it becomes available. In bivariate analysis, age of respondents, residents, race, education level, occupational status, marital status, and family income were significantly associated with vaccine acceptance of COVID19 vaccination.
Comparison between delay and acceptance of the future COVID-19.
| Variables | Categories | Will delay vaccine | Will Accept vaccine | p-Value |
|---|---|---|---|---|
| Age in category | <24 years | 499 (55.6) | 399 (44.4) | <0.001 |
| 25–34 | 193 (82.5) | 41 (17.5) | ||
| 35 and more | 100 (66.7) | 50 (33.3) | ||
| Gender | Female | 224 (60.4) | 147 (39.6) | 0.510 |
| Male | 568 (62.3) | 343 (37.7) | ||
| Place of residents | Rural | 65 (47.4) | 72 (52.6) | <0.001 |
| Urban | 727 (63.5) | 418 (36.5) | ||
| Race | Indian | 518 (67.2) | 253 (32.8) | <0.001 |
| Malay | 233 (52.7) | 209 (47.3) | ||
| Others | 41 (59.4) | 28 (40.6) | ||
| Educational level | Secondary education or less | 37 (55.2) | 30 (44.8) | <0.001 |
| Post-secondary education | 217 (76.7) | 66 (23.3) | ||
| Tertiary education | 538 (57.7) | 394 (42.3) | ||
| Occupational status | Employed | 287 (76.3) | 89 (23.7) | <0.001 |
| Student | 478 (55.7) | 380 (44.3) | ||
| Unemployed/homemaker | 27 (56.3) | 21 (43.8) | ||
| Marital status | Single | 532 (56.4) | 412 (43.6) | <0.001 |
| Not single | 260 (76.9) | 78 (23.1) | ||
| Family income | 130 (35.5) | 236 (64.5) | <0.001 | |
| RM 4,850 to RM 10,959 | 606 (72.9) | 225 (27.1) | ||
| >RM 10,960 | 56 (65.9) | 29 (34.1) | ||
| Total | 792 (61.8) | 490 (38.2) | ||
Chi-square test with p-value less than 0.05 is considered significant. All significant values are highlighted in bold.
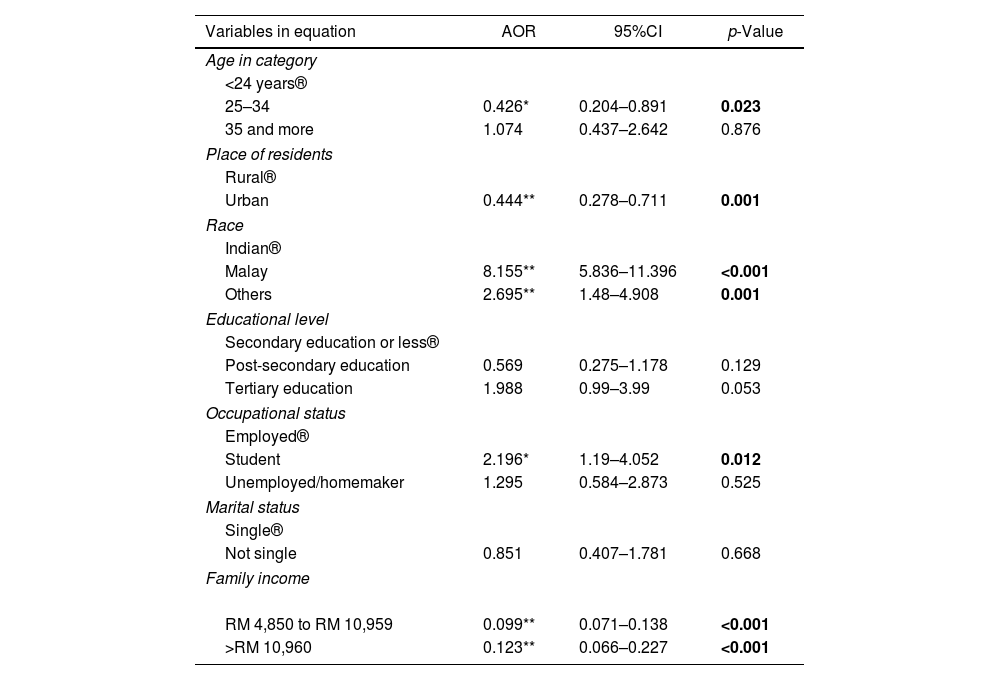
Table 4 exhibits the multivariate logistic regression to identify the determinants of vaccination acceptance. Those aged 25–34 years were less likely to accept the vaccine than those aged less than 24 years, with the AOR: 0.426 (95% CI: 0.204–0.891). Also, residents of urban areas were less likely to accept the vaccine than their counterparts, with the AOR: 0.444 (95%CI: 0.278–0.711). Those who were of the Malay race (AOR: 8.155; 95%CI: 5.836–11.396) and other races (AOR: 2.695; 95%CI: 1.48–4.908) were eight times and twice as likely to accept a COVID-19 vaccine compared to Indian race respondents. Students had twice the odds of vaccine acceptance among occupational categories than employed (AOR: 2.196; 95%CI: 1.19–4.052). Those who were earning between RM 4,850 to RM 10,959 (AOR: 0.09; 95%CI: 0.071–0.138) and more than RM 10,960 other race (AOR: 0.12; 95%CI: 0.066–0.227) were less likely to accept a COVID-19 vaccine compared those with monthly income of less than RM 4,849.
Factors affecting acceptance of the future COVID-19 vaccine.
| Variables in equation | AOR | 95%CI | p-Value |
|---|---|---|---|
| Age in category | |||
| <24 years® | |||
| 25–34 | 0.426* | 0.204–0.891 | 0.023 |
| 35 and more | 1.074 | 0.437–2.642 | 0.876 |
| Place of residents | |||
| Rural® | |||
| Urban | 0.444** | 0.278–0.711 | 0.001 |
| Race | |||
| Indian® | |||
| Malay | 8.155** | 5.836–11.396 | <0.001 |
| Others | 2.695** | 1.48–4.908 | 0.001 |
| Educational level | |||
| Secondary education or less® | |||
| Post-secondary education | 0.569 | 0.275–1.178 | 0.129 |
| Tertiary education | 1.988 | 0.99–3.99 | 0.053 |
| Occupational status | |||
| Employed® | |||
| Student | 2.196* | 1.19–4.052 | 0.012 |
| Unemployed/homemaker | 1.295 | 0.584–2.873 | 0.525 |
| Marital status | |||
| Single® | |||
| Not single | 0.851 | 0.407–1.781 | 0.668 |
| Family income | |||
| RM 4,850 to RM 10,959 | 0.099** | 0.071–0.138 | <0.001 |
| >RM 10,960 | 0.123** | 0.066–0.227 | <0.001 |
® Reference group; AOR, adjusted odds ratio.
**,* Significant at 1% and 5% level of significance, respectively.
Vaccination is a vital component in preventing the spread of COVID-19, and high vaccine acceptance is required in populations for effective vaccination initiatives. However, to achieve this aim, policymakers in Malaysia must first learn about people's perception of COVID-19 vaccines and the causes of vaccine apprehension. Therefore, we conducted this research in Malaysia among 1282 responders to assess the acceptance level, preferences, impact factors of future COVID-19 vaccine, and the factors influencing COVID-19 vaccination acceptance among the vaccine demand and vaccine delay groups. Of these participants, 96% said they would consider vaccination if vaccinations were successfully developed and approved for listing in the future, and 97% said they would follow their doctor's prescription for vaccination. The acceptance rate in our study was similar to the studies reported from China,24 Ecuador25 and United Kingdom26 while higher than the studies conducted in France,27 Israel,28 Italy,29 Portugal,29 Turkey,30 USA,31 South Africa,19 Malta,32 Jordan.33
On the other hand, literature revealed vaccine hesitancy is a common phenomenon across countries, with acceptance levels ranging from 55% in Russia to 89% in China.19 The most frequent reasons for vaccine hesitancy or refusal identified in the literature are perceived risks versus benefits and perceived safety.34–36 A similar research conducted in Indonesia showed 93% of people would be willing to take a vaccine with a 95% efficacy, but this acceptance level decrease sharply as the vaccine's safety declines (67%). We also observed that only 38.2% of respondents in the vaccine accept group wanted to take vaccinated as quickly as possible when it became available, whilst 61.8% wanted to wait before the vaccine's safety was confirmed. Another research conducted by Woon et al. in Malaysia also reported vaccination safety as one of the leading reasons for vaccine refusal.37 Hence, these findings highlight that the majority of Malaysians are in favour of the COVID-19 vaccine. However, these acceptance levels will be affected if vaccines need to be purchased and have a high cost, the government does not adequately subsidize them, and there is a lack of accessibility.1 The findings of the current study support this, i.e. 91.3% and 95.7% of the respondents said vaccine price and vaccine convenience, respectively, are the essential factor in vaccination decision-making.
In this study, most patients of all age ranges said they would postpone vaccines, with people aged 25–34 having the lowest acceptance (AOR: 0.426; 95 percent CI: 0.204–0.891). Similarly, in a survey undertaken in the United States, younger people were less likely than older adults to accept the COVID-19 vaccine (OR=0.69, 95 percent CI: 0.36–1.3).38 The less acceptance among young adults shows the optimistic bias since they are more inclined to underestimate their chance of contracting COVID-19. The literature further indicates that young adults are less likely to adhere to preventive measures like social distancing and handwashing than other age groups.19,39
Compared to rural areas, urban residents had a lower acceptance rate for COVID-19 vaccines (AOR=0.44, 95 percent CI: 0.278–0.711). This may be because city dwellers are more informed and aware about the COVID-19 vaccine than rural dwellers, so they are more worried about side effects and are more likely to avoid vaccination before effectiveness is confirmed.40,41 Another reason for the vaccination delay is that people in urban areas are less afraid of COVID-19 than people in rural areas. Again, this may be attributed to urban areas having more access to information and daily alerts about COVID-19.42
In the present study, it has been found that high-income groups have less acceptance of the vaccine than the low-income population. Cerda et al. lower-income and higher-risk populations can obtain vaccines at no cost, but high-income individuals must pay, so the willingness to pay for vaccines could contribute to vaccine refusal.43 Therefore, the price of vaccination should be affordable for all with promising results.44
People's education level plays a significant role in several measures related to vaccination experiences and behaviours, including evaluating both efficacy and the likelihood of severe side effects.45–48 In this study, people with a higher level of education (tertiary education) were more likely to consider vaccination than those with a lower level of education (post-secondary education and secondary education or less) (AOR: 1.988, 95 percent CI: 0.99–3.99). The global survey results also indicated that people with higher education were more willing to get vaccinated than people having lower education.49 Another study conducted in Indonesia also revealed that acceptance of vaccine was higher in individuals having postgraduate education.1 This highlights that health departments should design education programmes for increasing awareness regarding COVID-19 vaccination among people with lower education, leading to an overall improvement in acceptance and compliance of the general public.44
Another interesting result of our research was that married individuals were less likely to get vaccinated than unmarried individuals (AOR: 0.851, 95% CI: 0.407–1.781). However, a study conducted in Saudi Arabia revealed that married people were more likely to accept vaccination than unmarried ones (AOR: 1.79; 95% CI: 1.28–2.50).50 Hence, our result highlights that married people perceived themselves to be at lower risk of COVID-19 infection. This finding may be attributed to the fact that the proportion of single people in our survey was much higher than married.
Hence, future vaccine awareness strategies should consider subpopulations’ health, science, and general literacy levels, recognize locally trusted knowledge providers, and go beyond merely stating that vaccines are safe and effective. Vaccine awareness and adoption strategies should specifically resolve community-specific concerns or myths, spot-on historical problems that contribute to scepticism, and be sensitive to religious or political views.14,51 Researchers have found successful strategies for increasing vaccine trust and decreasing vaccine apprehension in various settings but converting this research into large-scale vaccination programmes would necessitate a keen understanding of and commitment to current consumer attitudes and needs. It would be crucial to include both formal and informal opinion leaders in these groups.1,34–37,52
Future directionsThis study advances the understanding of how health-related attitudes evolve. Focus on vaccine-related attitudes and intentions is essential because experts and stakeholders agree that having enough people vaccinate against COVID-19 is key to stemming the pandemic. While the focus of this paper is vaccine attitudes, broad dataset offers a unique opportunity to understand attitudes and behaviours over time. Due to the richness of data in this study, its unique nature, and its timeliness, we believe it is essential to make it available to other researchers interested in exploring it and publishing additional findings. Also, this research study has important practical implications for public health policy.
Strength and limitationsThe main strength of this study was a large number of respondents. However, a significant limitation is the representativeness of the sample population; data collection occurred online, which means we may not have reached vulnerable groups, including those with lower socioeconomic backgrounds and those who are illiterate. Since the recruitment of these respondents was done through convenience sampling, the presence of bias may limit its findings. However, the efficiency of data collection, lower cost, and acceptability of online survey recruitment could provide a valuable alternative for the formal regional or national survey.
ConclusionThe government and other relevant authorities should carefully consider all of the factors influencing COVID-19 vaccine acceptance rates across the country and devise measures to make the public aware of vaccine hesitancy's potential benefits and risks.
Authors’ contributionsRRM conceived and designed the study. RRM, AA1, TMK performed validation and reliability of the questionnaire. RRM, TMK, IZA, MS, AA2, SS1, SS2 and APS collected the data. RRM and AA1 conducted the statistical analysis and interpretation of the findings. RRM, APS, KA and wrote the first draft of the manuscript. RRM, APK, AA2 and SS2 provided manuscript editing. All authors read and approved the final version of this manuscript.
Availability of data and materialsAll the data supporting our findings have been presented in the manuscript; the datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
FundingNo funding was received for this study.
Conflict of interestAll authors declare no conflict of interest.