Male breast cancer is rare. It accounts for less than 1% of all cancers in men and less than 1% of all breast cancers. We present the case of a 73-years-old male patient with the coexistence of ipsilateral gynecomastia and two synchronous unilateral primary malignant tumors: invasive papillary carcinoma and invasive ductal carcinoma. Our case emphasizes the rare incidence of ipsilateral synchronous unilateral primary malignant tumors and gynecomastia in male breast. Since the triple radiological assessment (clinical, mammography or ultrasonography, and core biopsy) represents a mainstay of the clinical management, radiologists should be aware of the typical findings on clinical examination, mammography and ultrasound.
El cáncer de mama masculino es infrecuente, y representa menos del 1% de todos los cánceres en varones, y menos del 1% de todos los cánceres de mama. Presentamos el caso de un paciente de 73 años de edad, con coexistencia de ginecomastia ipsilateral y 2 tumores malignos primarios unilaterales sincrónicos: carcinoma papilar invasivo y carcinoma ductal invasivo. Nuestro caso resalta la rara incidencia de los tumores malignos primarios unilaterales sincrónicos e ipsilaterales y ginecomastia en la mama masculina. Como la triple evaluación radiológica (clínica, mamografía o ecografía y biopsia central) es la base del tratamiento clínico, los radiólogos deben tener en cuenta los hallazgos típicos en el examen clínico, la mamografía y la ecografía.
Male breast cancer is a rare condition accounting for less than 1% of all cancers in men and less than 1% of all breast cancers.1 Risk factors include advanced age, hormonal imbalance, obesity, a family history of breast cancer, BRCA1 and BRCA2 mutation, Klinefelter syndrome, testicular disease (such as undescended testis, orchitis, orchectomy) and history of chest irradiation.1,2 Male breast cancer has a peak incidence at 67 years, which is older than the mean age for women.3 The most common presentation in these patients is a painless palpable mass.3 Skin thickening and nipple retraction may be present.3 Approximately 50% of men have axillary nodal metastasis at initial evaluation.4 Diagnostic work-up includes clinical examination, bilateral mammography and US, and the final diagnosis is made with biopsy. Because of its rarity, the clinical management is widely influenced by female-population based studies.5 With this report we present a case of coexistence of ipsilateral gynecomastia and two synchronous unilateral primary malignant tumors: invasive papillary carcinoma and invasive ductal carcinoma with no familial history of breast malignancy.
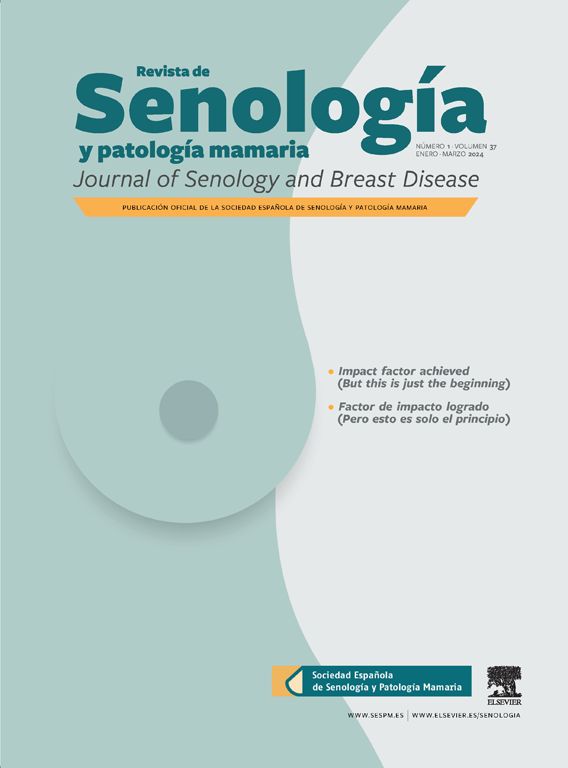
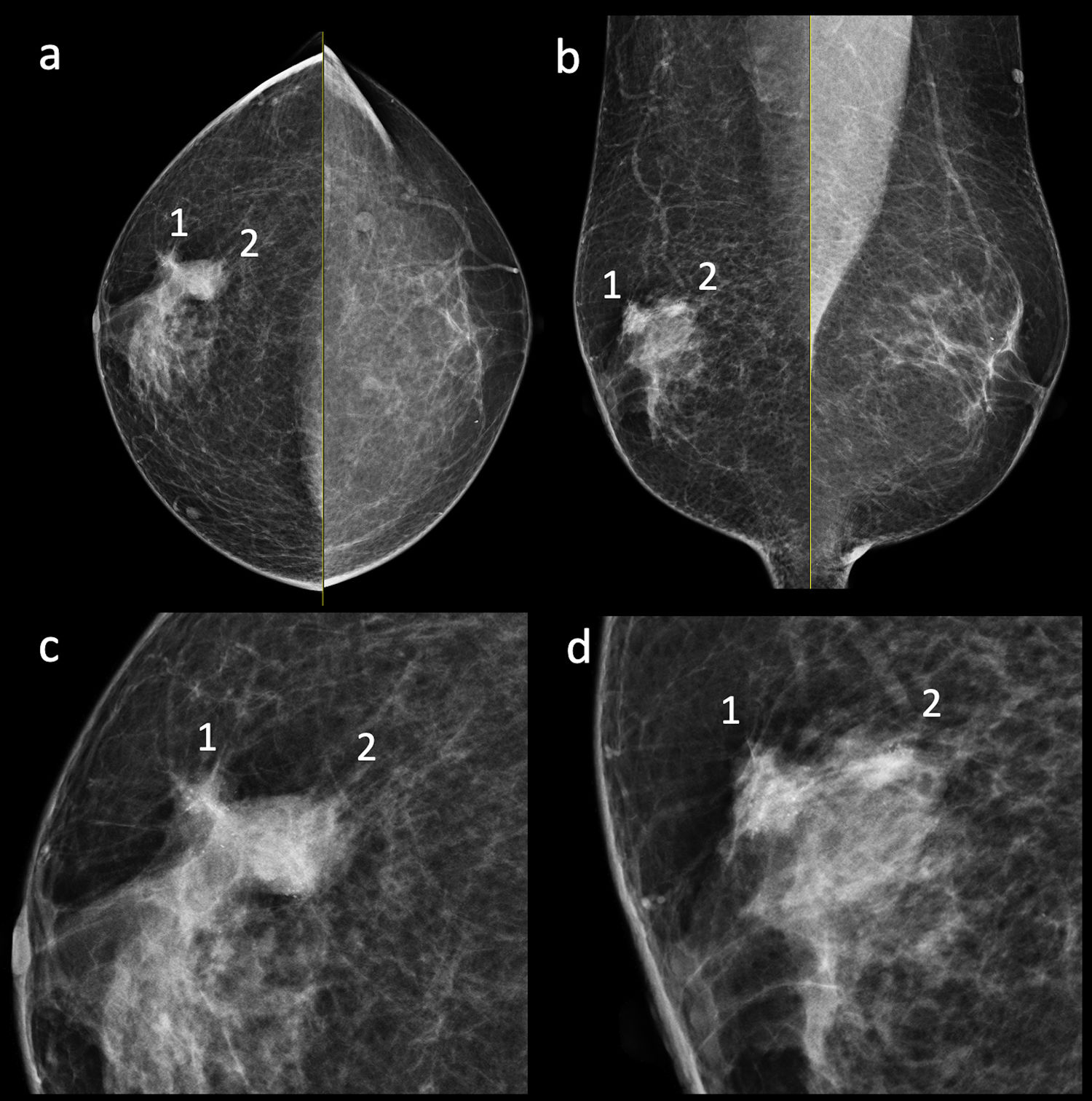
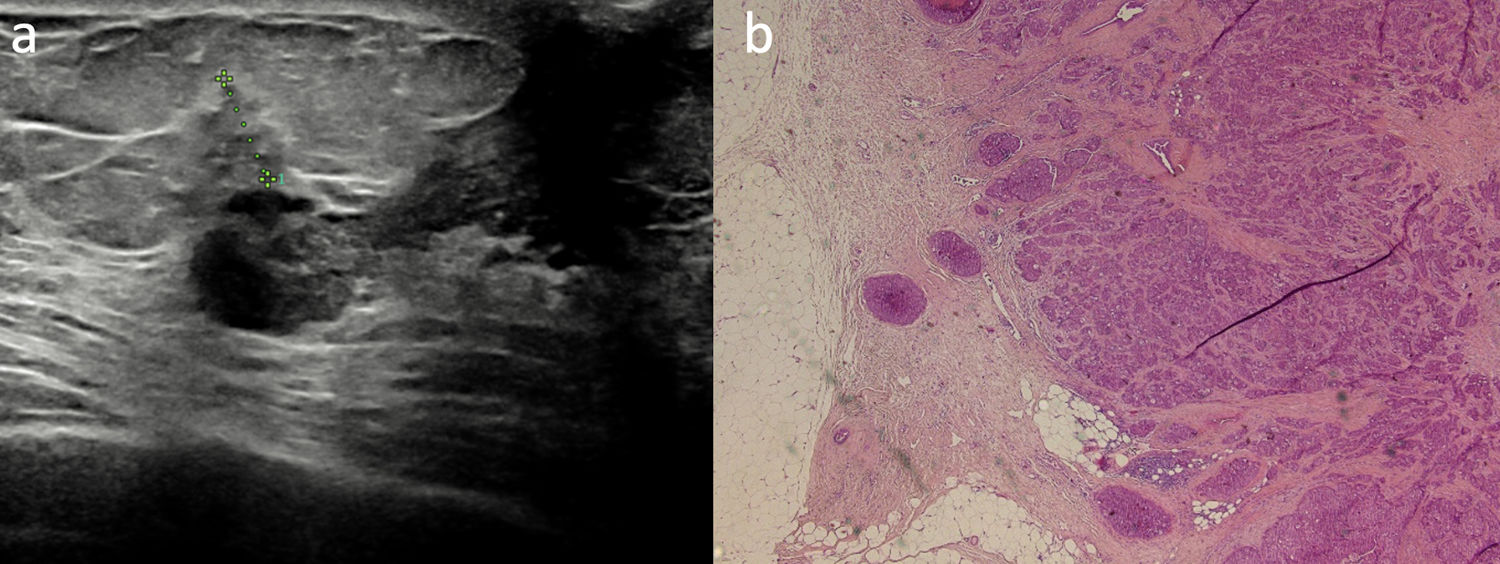
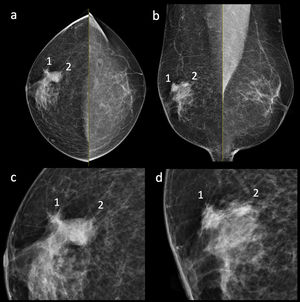
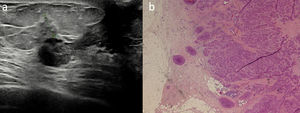
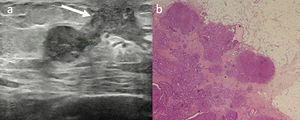
Clinical caseA 73-year-old-man with a medical history of benign prostatic hyperplasia and left nephrectomy (benign pathology) was referred to our Institution with a painless palpable mass in the right breast. There was no family history of breast diseases/malignancy. Two years earlier, in another hospital, he underwent an ultrasound examination for breast size increase which showed a unilateral gynecomastia. Two years later, the patient underwent a second clinical examination for a painless palpable mass in right upper outer quadrant, near the nipple. No nipple discharge or retraction were observed. Mammography demonstrated right retroareolar gynecomastia and, in the same side, at the site of the palpable mass, two suspicious contiguous irregular high-density masses with pleomorphic microcalcifications (Fig. 1a, b). Breast ultrasonography showed a 7mm, irregular shape, hypoechogenic nodule, which was surrounded by desmoplastic reaction (Fig. 2). Moreover, a second 18mm hypoechoic lobulated nodule was found (Figs. 2 and 3). Breast Imaging Reporting and Data System (BI-RADS) category of both lesions was 4C (highly suggestive of malignancy), and tru-cut biopsy of the two nodules was performed. The histopathological examination, later confirmed after surgery, revealed two synchronous independent primary malignant tumors: the smallest tumor was an invasive ductal carcinoma (histologic grade G2) and the other nodule was an invasive papillary carcinoma (histologic grade G1). Right mastectomy and sentinel lymph node biopsy were performed. Surgical specimen demonstrated free of disease breast surgical margins and no pathological nodes were identified. The final pathologic stage was IA (pT1c, pN0, pM0). Furthermore, immunohistochemical staining of both the tumors was positive for estrogen and progesterone receptor (100%) and HER-2 negative (i.e. molecular subtype LUMINAL-A).
Craniocaudal (a) and mediolateral oblique (b) views with respective enlargements (c, d) of the right breast showing flame shaped ipsilateral densities radiating from the nipple, suggestive for gynecomastia. Two suspicious contiguous high-density masses with pleomorphic microcalcifications were shown in the superior outer quadrant. The smallest lesion (1) has irregular margins while the largest lesion (2) has partly lobulated and ill-defined margins.
Ultrasonography (a) showing subareolar and central hypoechoic tissue which radiates posteriorly in the surrounding adipose tissue, suggestive for gynecomastia (white arrow). A 18mm hypoecoic lobulated nodule corresponding to the largest lesion on mammography (Fig. 1) was also detected. Breast biopsy was performed and breast invasive papillary carcinoma, with papillary and solid patter, was diagnosed (b).
Male breast cancer is a rare disease (less than 1% of all cancers in men; 1% of all cases are bilateral); the presence of two synchronous primary breast cancers on the same side is even more rare.1,6 Moreover, since the left breast is usually more frequently involved, our case (right breast) is uncommon.6 Two were the main reasons explaining the low incidence rate in men: the first is the relatively low amount of breast tissue and the second is the difference in hormonal status.6 The most common histological subtype of male breast cancer is invasive ductal carcinoma (approximately 85% of breast cancer cases in men), followed by papillary carcinoma.7 Invasive papillary breast carcinoma is a subtype of breast cancer that is more frequent in males than in females (5% and 1–2% respectively).7 According to Nofal MN and Yousef AJ, our report underlines the importance of a triple assessment approach: in fact, in our center the diagnostic work-up include the clinical assessment, radiologic assessment (mammography and ultrasound examination), and tissue biopsy (fine-needle aspiration cytology or core biopsy).8 Invasive ductal carcinoma usually appears as dense mass with irregular borders and spiculations on mammography corresponding to a solid, hypoechoic, ill-defined mass on ultrasound.7,9 On the other hand, papillary carcinoma usually appears as a well-circumscribed mass with occasional microcalcifications.6 Ill-defined borders point out infiltrative component.9 Though in our case it had a solid appearance, the typical sonographic presentation of papillary carcinoma includes a solid well-circumscribed mass or a complex cystic mass with thick walls containing both solid and cystic components.7 In our case, the different ultrasonographic presentation of the two nodules was highly suspicious of two different histological tumor types so biopsy was carried out from both the nodules. The larger nodule, which had a well-circumscribed aspect on ultrasound, was proved to be a papillary carcinoma, while the smaller irregular shape nodule with was an invasive ductal carcinoma. To the best of our knowledge, only one case of two synchronous unilateral primary malignant tumors in male was described in literature.10 Moreover, ours is the first case describing the coexistence of two synchronous unilateral primary malignant tumors and ipsilateral gynecomastia. Gynecomastia is the most common disease of male breast and it is caused by benign proliferation of ductal and stromal tissue elements.4 In this context, the differentiation between benign and malignant masses is crucial. Compared to breast cancer, at clinical examination patients with gynecomastia usually show a painful breast enlargement. A soft palpable and mobile subareolar mass, which can be unilateral, bilateral symmetric or bilateral asymmetric, is usually observed.1,3 Moreover, while gynecomastia is mostly bilateral, the unilateral involvement is usually expected in malignancy.7,9 The relationship of the mass with the nipple-areolar complex should be carefully assessed. In fact, an eccentric location is highly suspicious for cancer.11 Male breast cancer is typically located in the subareolar tissue and it is eccentric to the nipple. On the other hand, central involvement is typical of gynecomastia.9 The relationship between gynecomastia and male cancer is widely debated in literature.6,12–14 For instance, Brinton A. et al. showed a statistically significant association between male breast cancer and gynecomastia. In this regard, it was postulated that it might affect the risk for cancer by providing increased tissue at risk but it is also possible that increased surveillance and recall biases could be involved.12 On the other hand, Fentiman et al. concluded that there was no convincing evidence to link gynecomastia with male breast cancer.13 In fact, the incidence of gynecomastia in mastectomy specimens from male breast cancer cases was 21%, which is less than the incidence of 40–55% reported at autopsy of unselected cases.14
ConclusionThis report described an exceeding rare case of a 73-year-old male with gynecomastia and two synchronous unilateral primary breast cancers: invasive ductal carcinoma and invasive papillary breast carcinoma, the latter with an unusual ultrasonographic presentation. Since the triple radiological assessment represent a mainstay of the clinical management, radiologists should be aware of the typical imaging findings on clinical examination, mammography and ultrasound.
Ethical approvalProcedure performed in this report involving human participant was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interestsThe authors declare that they have no conflict of interest.