Stereotactic body radiotherapy has experienced exponential development in recent years, as its ablative capacity has demonstrated a benefit in certain patients including oligometastatic and oligoprogressive patients. We present a case of a 59-year-old woman with a history of infiltrating metastatic ductal breast carcinoma with vertebral bone oligoprogression. After radical surgical treatment and re-irradiation SBRT, a complete response was achieved. After more than two years of follow-up the patient remains with neither local nor distant recurrence. Patients with oligometastatic or oligoprogressive breast cancer are candidates for radical treatment modalities. Stereotactic body radiotherapy has demonstrated promising local control, progression free survival and overall survival in these patients. In this context, there are currently ongoing phase III studies in order to provide stronger evidence.
La radioterapia estereotáctica corporal ha sufrido un desarrollo exponencial en los últimos años. Debido a su capacidad ablativa, esta técnica ha demostrado un beneficio en determinados pacientes incluyendo los pacientes oligometastásicos o con oligoprogresión. Se presenta el caso de una mujer de 59 años con antecedentes de carcinoma ductal de mama infiltrante con oligoprogresión ósea vertebral. Tras tratamiento quirúrgico y reirradiación del lecho con SBRT se obtuvo una respuesta completa a nivel local. Tras más de dos años de seguimiento, la paciente permanece sin recidiva local ni a distancia. Las pacientes con cáncer de mama oligometastásico o con oligoprogresión son candidatas a recibir un tratamiento radical. La radioterapia corporal estereotáctica ha demostrado unas cifras de control local, supervivencia libre de progresión y supervivencia global prometedoras en estas pacientes. En este contexto, se están desarrollando ensayos fase III que aportarán una evidencia más sólida en el tratamiento de estas pacientes.
The clinical state of oligometastases was first described by Hellman and Weichselbaum in the 1990s.1 They suggested that there is an intermediate tumor stage between localized lesions and the widespread metastatic disease and proposed the concept of “oligometastatic disease” (OMD). Some studies have described OMD as a maximum of five treatable lesions. Recently, Guckenberger M, et al. redefined a new OMD classification system.2
Stereotactic body radiotherapy (SBRT) has experienced exponential development in recent years, as its ablative capacity has demonstrated a benefit in certain patients including oligometastatic (OM) and oligoprogressive (OP) patients.3 Oligoprogression is a limited tumor progression in some tumor sites with complete response or stable disease in other sites. SBRT allows the administration of high antitumor biologically effective doses. There are different dose fractionation schemes used depending on the anatomical location, size and tumor histology, among other factors. In general, the most common fractionation used in SBRT is over 6 Gy per fraction delivered 1–5 fractions.
The radical treatment of metastatic lesions includes surgery, radiation therapy and combined therapies.4
Case presentationWe present a case of a 59-year-old woman with a history of infiltrating metastatic ductal carcinoma of the right breast. The subtype of ER negative, PR 50%, HER-2 positive and ki-67 25% was identified at the time of diagnosis in March 2013. CT revealed multiple pulmonary and hepatic metastases. No medical or surgical history of interest. After diagnosis, the patient started systemic treatment with Navelbine given orally and Herceptin.
Following two years with stable disease, on 15 January 2015, CT revealed the progression of a unique bone metastasis of the vertebral column on vertebra T3. The patient had been presenting pain for a period of three weeks. She had no neurological alterations. MRI confirmed the bone metastasis on the T3 right lateral vertebral body with bulging of the medullary canal. Given the oligoprogression of the disease, a radical treatment with SBRT was performed until reaching a dosage of 18 Gy in a single fraction of the T3 vertebral body at Hospital Vithas del Consuelo. The spinal cord received a maximum dose (Dmax, 0.01 cc) of 5.7Gy. Following treatment with SBRT, systemic treatment with Navelbine given orally and Herceptin was resumed.
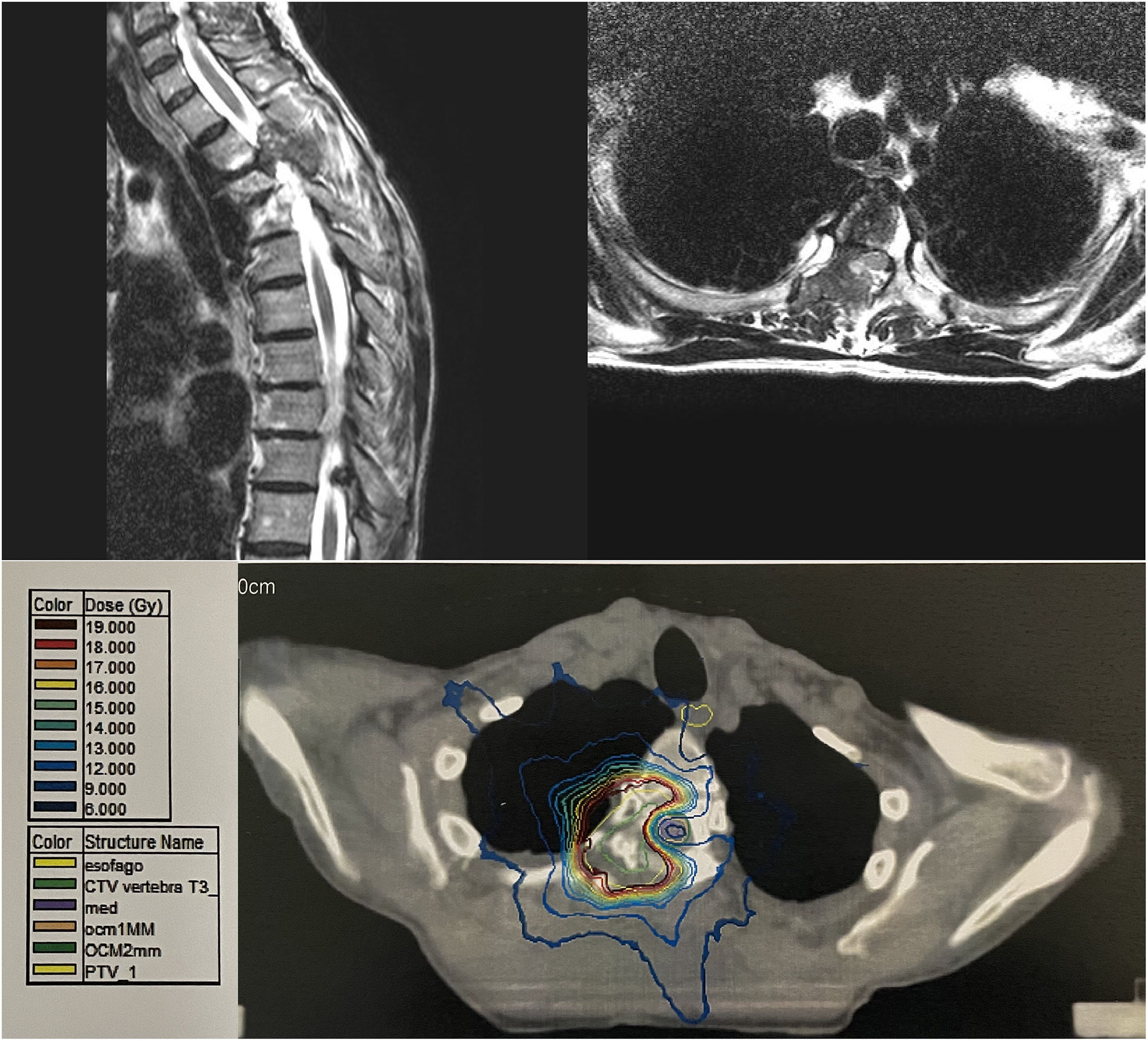
In February 2019, follow up with CT indicated local progression of the previously treated lesion on vertebra T3. The patient was asymptomatic. An MRI was performed showing an osteolytic lesion in T3 affecting the body, pedicle, and right lamina, with an extradural tumor mass occupying the spinal canal in 50% of T3 and medullary compression/deviation from right to left [Fig. 1a, 1b]. Tumor size was 25x28x28 mm and Spinal Instability Neoplastic Score (SINS) was 6. Based on these findings, the tumor in the spinal canal was resected, with subsequent post-operative SBRT on the surgical site.
On 1 March 2019, the extradural intra-spinal tumor mass was resected, decompressing the spinal cord and separating it from the surgical site using two Teflon sheets (the sheets surrounded the thecal sac). Surgical fixation was not performed. There were no complications after the surgical procedure.
After the resection, on 25 March 2019, SBRT was performed on the surgical site of the T3 vertebra. Fixation and immobilization were carried out using a body stereotaxic frame (BodyFix®, Elekta). The simulation was performed by CT and MRI. IMRT was used with stereotaxic coordinates on the tumor bed until reaching a dosage of 18 Gy in a single fraction [Fig. 1c]. The spinal cord received a maximum dose (Dmax, 0.01 cc) of 7.3Gy. Following treatment with SBRT, the patient resumed systemic treatment with Navelbine given orally and Herceptin.
As of the last follow-up on 25 October 2021, the patient remained stable, with no evidence of local or distant progression. No evidence of toxicity secondary to salvage SBRT treatment according to CTCAE v.5 scale.
Discussion and resultsBreast cancer (BC) is the most common cancer in women, with 2,26 million estimated new BC cases worldwide in 2020.5 Bone is the most common site of metastasis for BC.6 Nevertheless, metastasis confined to the bone have a more favorable prognosis than other types of distant metastasis.7
As we previously mentioned, SBRT and its ablative ability offers a greater tumor control compared to conventional palliative radiotherapy (CPR).3
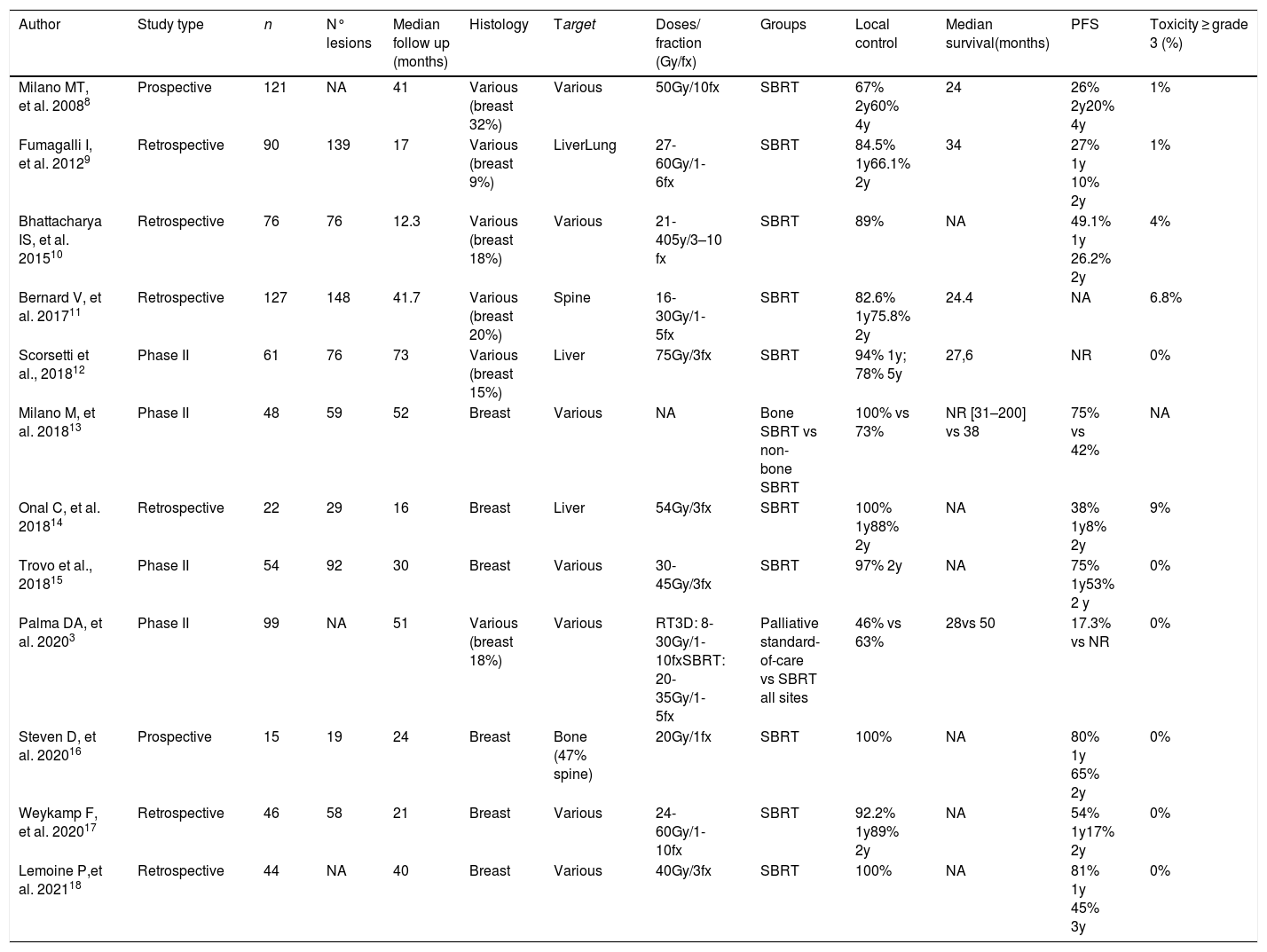
A non-systematic review has been carried out on the topic of SBRT targeting oligometastases in BC. Table 1 summarizes the publications reviewed from PubMed database within the last 10 years.
A review of the different retrospective and prospective trials of SBRT in oligometastases breast cancer.
| Author | Study type | n | N° lesions | Median follow up (months) | Histology | Target | Doses/ fraction (Gy/fx) | Groups | Local control | Median survival(months) | PFS | Toxicity ≥ grade 3 (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Milano MT, et al. 20088 | Prospective | 121 | NA | 41 | Various (breast 32%) | Various | 50Gy/10fx | SBRT | 67% 2y60% 4y | 24 | 26% 2y20% 4y | 1% |
| Fumagalli I, et al. 20129 | Retrospective | 90 | 139 | 17 | Various (breast 9%) | LiverLung | 27-60Gy/1-6fx | SBRT | 84.5% 1y66.1% 2y | 34 | 27% 1y 10% 2y | 1% |
| Bhattacharya IS, et al. 201510 | Retrospective | 76 | 76 | 12.3 | Various (breast 18%) | Various | 21-405y/3–10 fx | SBRT | 89% | NA | 49.1% 1y 26.2% 2y | 4% |
| Bernard V, et al. 201711 | Retrospective | 127 | 148 | 41.7 | Various (breast 20%) | Spine | 16-30Gy/1-5fx | SBRT | 82.6% 1y75.8% 2y | 24.4 | NA | 6.8% |
| Scorsetti et al., 201812 | Phase II | 61 | 76 | 73 | Various (breast 15%) | Liver | 75Gy/3fx | SBRT | 94% 1y; 78% 5y | 27,6 | NR | 0% |
| Milano M, et al. 201813 | Phase II | 48 | 59 | 52 | Breast | Various | NA | Bone SBRT vs non-bone SBRT | 100% vs 73% | NR [31–200] vs 38 | 75% vs 42% | NA |
| Onal C, et al. 201814 | Retrospective | 22 | 29 | 16 | Breast | Liver | 54Gy/3fx | SBRT | 100% 1y88% 2y | NA | 38% 1y8% 2y | 9% |
| Trovo et al., 201815 | Phase II | 54 | 92 | 30 | Breast | Various | 30-45Gy/3fx | SBRT | 97% 2y | NA | 75% 1y53% 2 y | 0% |
| Palma DA, et al. 20203 | Phase II | 99 | NA | 51 | Various (breast 18%) | Various | RT3D: 8-30Gy/1-10fxSBRT: 20-35Gy/1-5fx | Palliative standard-of-care vs SBRT all sites | 46% vs 63% | 28vs 50 | 17.3% vs NR | 0% |
| Steven D, et al. 202016 | Prospective | 15 | 19 | 24 | Breast | Bone (47% spine) | 20Gy/1fx | SBRT | 100% | NA | 80% 1y 65% 2y | 0% |
| Weykamp F, et al. 202017 | Retrospective | 46 | 58 | 21 | Breast | Various | 24-60Gy/1-10fx | SBRT | 92.2% 1y89% 2y | NA | 54% 1y17% 2y | 0% |
| Lemoine P,et al. 202118 | Retrospective | 44 | NA | 40 | Breast | Various | 40Gy/3fx | SBRT | 100% | NA | 81% 1y 45% 3y | 0% |
NA - not available; NR - not reached.
The potential benefit of SBRT in oligometastatic BC has increased the evidence supporting local control (LC), overall survival (OS) and progression free survival (PFS) in these patients.
After this review, 12 articles were included, four of them were randomized clinical trials (RCT),3,12,13,15 2 were prospective studies8,16 and 5 were retrospective studies.9–11,14,17,18
The sample size is remarkably different among studies ranging from 22 to 227 patients. The follow-up is also distinct ranging from 17 to 73 months. Furthermore, 6 out of 12 articles include multiple histologies.3,8–12
LC after SBRT is achieved in 60 to 100% of the cases,8,16 and OS varies from 24 to 50 months.3,8 When focusing on studies including only BC patients13–18 LC varies from 73% to 100%.13,16 OS median ranges from 28 to 50 months and it was not reached in one of the studies.13 PFS varies from 38 to 81%14–18 and 2-year PFS from 17,3 to 65%.3,16
A single study included exclusively bone lesions (47% spine metastases) in BC patients.16 This prospective study reports up to 100% LC rates and a 2-year PFS of 65% of bone metastases treated with radiosurgery (20Gy in 1 fraction).
Milano M et al. demonstrated a better LC (100% vs. 73%), OS (not reached vs 38 months; p = 0.002) and PFS (75% vs 42%) after the treatment of extracranial bone lesions compared to those not involving the skeleton (adrenal gland, liver, lung or lymph nodes).13 Other authors also report differences in terms of LC depending on the target.3
Palma et al. reported an improvement in LC (46% vs 63%; p < 0.05) and OS (28% vs 50%; p < 0.05) after SBRT to all metastatic sites compared to CPR standard-of-care in oligometastatic patients. No increase in toxicity was observed after SBRT.3 In this context, Sprave and colleagues showed no detriment in the quality of life (assessed through QOL-BM22, QLQ FA13 and QSC-R10) following SBRT compared to CPR in vertebral metastatic lesions.19 Grade 3 or higher toxicity reported in the articles reviewed ranges from 0% to 9%.
In patients with spinal instability, cord compression, or neurologic deficits, the standard of care is surgery followed by radiation therapy. Some authors report excellent results with the use of SBRT in patients who have undergone surgical intervention for spine metastases.20,21 Separation surgery, as our case, refers to providing sufficient surgical circumferential decompression of the spinal cord to create at least 1–2 mm of space between the spinal cord and disease to optimize the SBRT dose distribution.
Separation surgery for the treatment of spinal cord compression is especially useful when reirradiation is required since it facilitates a dosimetric advantage, achieving higher doses and presumably a better local control.22,23
SBRT in oligometastatic patients shows favorable results. In our patient, after radical surgical treatment and salvage SBRT, a complete response was achieved. After more than two years of follow-up the patient remains with neither local nor distant recurrence. Not only does SBRT benefit local control but it also delays the initiation of a new systemic treatment.
Finally, we have to consider that the studies reviewed show heterogeneity both in the target location and treatment site (lung, liver, bone…). Owing to the limitations mentioned above, few robust conclusions can be drawn to the date. There are currently several ongoing clinical trials, such as NRG BR002 (NCT02364557), AVATAR (ACTRN12620001212943)24 or STEREO-OS (NCT03143322),25 that will provide more data in relation to the SBRT in oligometastatic BC patients.
ConclusionsPatients with oligometastatic or oligoprogressive breast cancer are candidates for radical treatment modalities. SBRT has demonstrated promising LC, PFS and OS in these patients with an acceptable toxicity. In this context, there are currently ongoing phase III studies in order to provide stronger evidence.
FundingThe authors received no financial support for the research, authorship and publication of this article.
Ethical considerationsThe authors have complied with the ethical relevant standards for publication.
Conflicts of interestThe authors declare no conflict of interest.