This study aimed to propose criteria for negative symptoms remission (NSR) in schizophrenia using the Brief Negative Symptom Scale (BNSS).
Material and methods274 participants were assessed on the Positive and Negative Syndrome Scale (PANSS), BNSS and Social and Occupational Functioning Assessment Scale (SOFAS). Two criteria for NSR on the BNSS were proposed – NSR based on the BNSS domains scores (NSRBNSS_DOMAINS) and NSR based on 5 key items of the BNSS (NSRBNSS_5ITEMS). A SOFAS score of 61 and above was considered as functional remission (FR). Logistic regressions were run to examine the association between FR and NSR. Receiver operating characteristic (ROC) curve analysis was performed for the NSR criteria on FR. Kappa agreement statistic was used to evaluate the agreement between the two NSR criteria.
ResultsEighty-nine (32.5%) participants fulfilled NSRBNSS_DOMAINS criterion whereas 70 (25.6%) participants fulfilled NSRBNSS_5ITEMS criterion. The two NSR criteria had substantial agreement (Kappa statistic=0.797) with each other. Sixty-one (25.3%) participants were in FR. FR was significantly associated with NSR, irrespective of the criterion used. To predict FR, the Area Under the Curve for NSRBNSS_DOMAINS and NSRBNSS_5ITEMS were 0.761 (CI: 0.696–0.826, p<0.001) and 0.723 (CI: 0.656–0.790, p<0.001), respectively. Hence, both NSR criteria demonstrated a fair ability to discriminate between functional remitters and non-remitters.
ConclusionsDepending on the setting and needs, clinicians and researchers might employ either the full BNSS or an abbreviated 5-item BNSS scale to identify NSR in schizophrenia. More research is needed to further examine the validity of these criteria in schizophrenia.
El objetivo de este estudio fue proponer criterios para la remisión de síntomas negativos (NSR) en la esquizofrenia utilizando la Escala Breve de Síntomas Negativos (BNSS).
Material y métodos274 participantes fueron evaluados con la Escala de Síndrome Positivo y Negativo (PANSS), BNSS y la Escala de Evaluación del Funcionamiento Social y Ocupacional (SOFAS). Se propusieron dos criterios para NSR en el BNSS: NSR basado en las puntuaciones de los dominios BNSS (NSRBNSS_DOMAINS) y NSR basado en 5 elementos clave del BNSS (NSRBNSS_5ITEMS). Una puntuación SOFAS de 61 y superior se consideró como remisión funcional (FR). Se realizaron regresiones logísticas para examinar la asociación entre FR y NSR. El análisis de la curva de características operativas del receptor (ROC) se realizó para los criterios NSR en FR. Se utilizó la estadística de concordancia Kappa para evaluar la concordancia entre los dos criterios de NSR.
ResultadosOchenta y nueve (32,5%) participantes cumplieron el criterio NSRBNSS_DOMAINS mientras que 70 (25,6%) participantes cumplieron el criterio NSRBNSS_5ITEMS. Los dos criterios de NSR tuvieron un acuerdo sustancial (estadística Kappa = 0,797) entre sí. Sesenta y un (25,3%) participantes estaban en FR. La FR se asoció significativamente con la NSR, independientemente del criterio utilizado. Para predecir la FR, el área bajo la curva para NSRBNSS_DOMAINS y NSRBNSS_5ITEMS fueron 0,761 (IC: 0,696-0,826, p <0,001) y 0,723 (IC: 0,656-0,790, p <0,001), respectivamente. Por lo tanto, ambos criterios NSR demostraron una capacidad adecuada para discriminar entre remitentes funcionales y no remitentes.
ConclusionesDependiendo del entorno y las necesidades, los médicos e investigadores pueden emplear la BNSS completa o una escala BNSS abreviada de 5 ítems para identificar la NSR en la esquizofrenia. Se necesita más investigación para examinar a fondo la validez de estos criterios en la esquizofrenia.
Schizophrenia is a heterogeneous disorder and its long-term course can vary from individual to individual. It is important to define outcomes in schizophrenia to make informed clinical decisions, as well as to guide policy decision making. Often, outcomes in schizophrenia were defined as response and remission. Response in schizophrenia refers to a clinically meaningful improvement in symptoms from a start point to an endpoint, regardless of how symptomatic the individual is at the endpoint.1,2 No standard criterion of response in schizophrenia were established for clinical use; various cut-offs based on schizophrenia symptom rating scales such as the Positive and Negative Syndrome Scale (PANSS),3 Brief Psychiatry Rating Scale4 and Clinical Global impression scale5 were suggested to define response.2 On the other hand, symptomatic remission was defined as a state characterised by an absence of significant symptoms, or that the remaining symptoms were of low or mild intensity and did not affect the behaviour of an individual.1,2,6 The Remission in Schizophrenia Working Group (RSWG) proposed standard criteria to evaluate remission in schizophrenia.6 A score of mild or below was suggested as the cut-off for symptom severity needed to achieve remission; this severity of illness had to be maintained for a minimum of 6 months’ duration.
The RSWG criteria for remission in schizophrenia were based on positive, negative as well as disorganised symptoms. Remission on negative symptoms (NSR) was defined using the Scale for the Assessment of Negative Symptoms (SANS)7 or the PANSS negative subscale. However, these scales have limitations when used to assess negative symptoms (NS); both the SANS and the PANSS assess NS based only on behaviours and include few items that do not belong to the NS construct of schizophrenia.8 The SANS assesses the 5 domains of NS (anhedonia, asociality, avolition, blunted affect and alogia)9 but combines asociality and anhedonia into one domain. The PANSS does not have items to assess anhedonia10–13; only 3 items of the PANSS are used to determine NS remission (NSR),6 which do not reflect all domains of NS.
The Brief Negative Symptom Scale (BNSS) was developed to overcome the limitations of the older NS rating scales.14 The BNSS assesses NS based on both behaviours and internal experiences unlike the SANS and the PANSS. It also assesses anticipatory anhedonia. The original English version of the BNSS has been reported to have good reliability and validity.14–18 In addition, many translated versions of the BNSS have been validated: Brazilian,19 Danish,20 Dutch,21 German,22 Italian,17 Japanese,23 Korean,24 Polish,25 Spanish,26 and Turkish,27 However, criteria for NSR have not been established on the BNSS.
NS pose a substantial burden on individuals with schizophrenia, their families and carers. The prevalence of NS in schizophrenia is considerable; at least 1 NS is present in more than half (57.6%) of individuals with chronic schizophrenia.28 They are associated with poor functioning29–31 and lower quality of life in schizophrenia.32 Additionally, they respond minimally to current available treatments for schizophrenia33,34 and remain an important unmet clinical need.8 Importantly, NSR is associated with a higher likelihood of functional remission (FR) in schizophrenia.35
The aim of this study was to propose criteria for NSR in schizophrenia using the BNSS. We assessed the validity of the proposed BNSS NSR criteria by investigating their association with FR and their performance in prediction of FR.
Material and methodsSetting and study participantsStudy participants were recruited from the outpatient clinics at the Institute of Mental Health (IMH), Singapore, from August 2014 to December 2017 via a convenience sampling approach. English speaking individuals with a diagnosis of schizophrenia, between the ages of 21 to 65 years, were invited to participate in the study. Potential participants were approached by their own treating physicians/healthcare providers to participate in this study when they came for their regular clinic visits. Also, patients with schizophrenia who had agreed to be re-contacted during previous research studies in our department were contacted by phone call and invited to take part in the study. Those with mental retardation (IQ<70), a history of head injury or any neurological disorder were excluded from the study. Among psychiatric comorbidities, only current alcohol or substance use disorder was an exclusion criterion. The Structured Clinical Interview for DSM-IV-TR Axis I Disorder-Patient Edition (SCID-I/P)36 was administered to ascertain the diagnosis of schizophrenia. A total of 277 participants were recruited, 3 participants withdrew and did not complete the clinical assessments; therefore, the sample reported herein was 274. Ethics approval for this study was provided by the National Healthcare Group's Domain Specific Review Board. All participants provided written informed consent prior to the study assessments.
AssessmentsSocio-demographic and illness-related information was collected. The PANSS was used to assess severity of symptoms of schizophrenia. It has 7 items to assess positive and NS each, and 14 items to assess general psychopathology symptoms. Each item was rated on a Likert scale from 1 (absent) to 7 (extreme). A 5-factor structure of the PANSS was validated in Singapore; the factors were: positive, negative, excitement, depression and cognitive.37
The BNSS was used to evaluate the presence and severity of NS in schizophrenia. It has 13 items rated on a 7-point scale, from 0 (normal) to 6 (extremely severe). The items are divided into 6 subscales: anhedonia, distress, asociality, avolition, blunted affect and alogia. The ratings are based on a semi-structured interview. The 5-factor structure of the BNSS has been validated for use locally,16 as well as at other international sites.15,38 The 5 factors or domains of the BNSS overlap with the BNSS subscales, except the distress subscale. The time frame for ratings on the PANSS and BNSS was 1 week.
Functioning was rated on the Social and Occupational Functioning Assessment Scale (SOFAS).39 The SOFAS score ranges from 0 (grossly impaired functioning) to 100 (excellent functioning), and is based exclusively on the individual's level of social, occupational or role functioning, with no regard to symptoms. Participants with SOFAS score of 61 and above were considered to be in FR.40–42
The original English version of all the rating scales were used. The assessments were done by 3 raters; 1 research clinician, 1 master level research psychologist and 1 bachelor level research psychologist. The raters had at least 2 years’ experience in rating schizophrenia symptoms. All raters were trained in the administration and scoring of the rating scales used in the study. The raters obtained an intra-class correlation coefficient (ICC) of above 0.80 for ratings on the PANSS and BNSS. Regular case discussions and raters’ meetings were conducted to ensure adequate agreement in rating.
Definition of NSRNSR was defined based on symptom severity; the time criterion could not be applied because the study was cross-sectional and not designed to follow changes in outcome over time. Following up patients longitudinally is resource intensive; additionally, it has been suggested that the addition of duration criteria to the symptom severity criteria when ascertaining remission did not provide additional significant information.43 Therefore, ascertaining remission without duration criteria has been an acceptable approach in related literature.35,43 The proposed NSR criteria based on the BNSS criteria and their rationale are as follows:
- 1.
NSR based on the BNSS domains scores (NSRBNSS_DOMAINS): The NSRBNSS_DOMAINS criterion was based on the remission of NS across all the 5 NS domains in the BNSS. For each of the BNSS domain, the sum of item scores was divided by the number of items in that domain to compute an average domain score for each participant, as previously proposed.38 An average score of 2 (corresponding to mild severity of symptoms) or less on each of the BNSS domains was needed to be considered as remitted on NS, based on the assumption that mild symptoms would not interfere with daily functioning.6
- 2.
NSR based on key BNSS items (NSRBNSS_5ITEMS): The NSRBNSS_DOMAINS criterion required administration and rating on the full BNSS (except distress), followed by computation of an average score for each of the 5 domains of NS. Administering the full BNSS takes around 15min,14 and another 5–10min might be needed to score the items. This could limit its application in clinical practice; therefore, we proposed a NSR criteria based on key BNSS items. Instead of taking all the BNSS items to ascertain NSR, employing 1 representative item from each domain can be done much faster and yet offer adequate robustness to the NSR criterion in a busy clinical practice. The selected 5 BNSS items and the rationale for their selection are shown below. Consistent with the NSRBNSS_DOMAINS criterion, a score of 2 or below on all 5 items was required to be considered as NSR.
- i.
BNSS Item 3, Intensity of expected pleasure from future activities – In schizophrenia, anticipatory anhedonia is primarily impaired; Individuals with schizophrenia reported less pleasure than healthy controls when anticipating future activities, and reported normal levels of pleasure when engaged in any enjoyable activity (consummatory pleasure).44 Anticipatory but not consummatory anhedonia ratings were found to correlate with ratings of clinical anhedonia and family and social functioning in schizophrenia.44 The BNSS item 3 from the anhedonia subscale assesses anticipatory anhedonia and was therefore selected.
- ii.
BNSS Item 6, Asociality: Internal experience – This item assesses internal experiences related to social activities which are more stable and primary. The only other BNSS asociality item (item 7) assesses behaviours related to social activities and behaviours may be secondary to other factors, example, lack of opportunities. Moreover, behaviours are rated based on reports of functioning; therefore, the behaviour item could actually be evaluating functioning rather than NS.45 Hence, the internal experience item 6 was selected from the Asociality subscale.
- iii.
BNSS Item 8, Avolition: Internal experience – This item assesses internal experiences related to Avolition and was selected from the Avolition subscale based on a similar rationale as Asociality item 6.
- iv.
BNSS Item 9, Facial expressions – Facial expressions are most commonly used to assess blunted affect in research and clinical settings. Ratings on blunted affect in commonly used rating scales, e.g., the Positive and Negative Syndrome Scale (PANSS), take mainly facial expressions into consideration, followed by expressive gestures and speech variability.3 Hence, item 9 was selected from the Blunted Affect subscale of the BNSS.
- v.
BNSS Item 12, Quantity of speech – Decreased quantity of speech is most commonly used to assess alogia in schizophrenia. In fact, another newer NS rating scale, the Clinical Assessment Interview for Negative Symptoms (CAINS), only relies on quantity of speech to assess alogia.45–47 Hence, item 12 was selected from the Alogia subscale.
- i.
Correlations of the selected BNSS items 3, 6, 8, 9 and 12 with the other items in their respective domains were strong, suggesting that they were a part of the respective conceptual domain. Item 3 was strongly correlated to the remaining anhedonia items 1 (rs=0.761, p<0.001) and 2 (rs=0.726, p<0.001). Similarly, item 6 was strongly correlated to asociality item 5 (rs=0.694, p<0.001) and item 8 was strongly correlated to avolition item 7 (rs=0.768, p<0.001). The selected blunted affect item 9 was also strongly correlated to items 10 (rs=0.662, p<0.001) and 11 (rs=0.700, p<0.001). Item 12 was very strongly correlated to alogia item 13 (rs=0.916, p<0.001).
Statistical analysesMean (standard deviations) or median (Interquartile range) were presented for continuous variables and frequencies (percentages) for categorical variables. To compare NS remitters vs. non-remitters, Chi-squared test was used for categorical variables whereas t-Test or Mann–Whitney's U was used for continuous variables. Spearman's correlations were used to assess correlations among BNSS items.
Logistic regressions were run separately for each of the 5 NS domain scores to examine its association with FR; and each of the NSR criteria to examine the association between FR and NSR. For each NSR criterion, unadjusted regressions were first conducted followed by adjustment of the model for covariates – age, gender, highest education level and PANSS positive, excitement, depression and cognition scores.
A receiver operating characteristic (ROC) curve analysis was performed to examine the ability of NSRBNSS_DOMAINS and NSRBNSS_5ITEMS to differentiate between those in FR and those not in FR. Area Under the Curve (AUC), Positive predictive value (PPV), negative predictive value (NPV), sensitivity and specificity of each of the NSR criterion to predict FR were computed. Z-test was used to compare AUC among the NSRBNSS_DOMAINS and NSRBNSS_5ITEMS criteria. Kappa agreement statistic was used to evaluate the agreement between the NSRBNSS_DOMAINS and NSRBNSS_5ITEMS criteria. Statistical significance was established at p<0.05. All statistical tests were performed on SPSS 25.0, except ROC analyses and Z-test that were done using Medcalc 19.6.4.
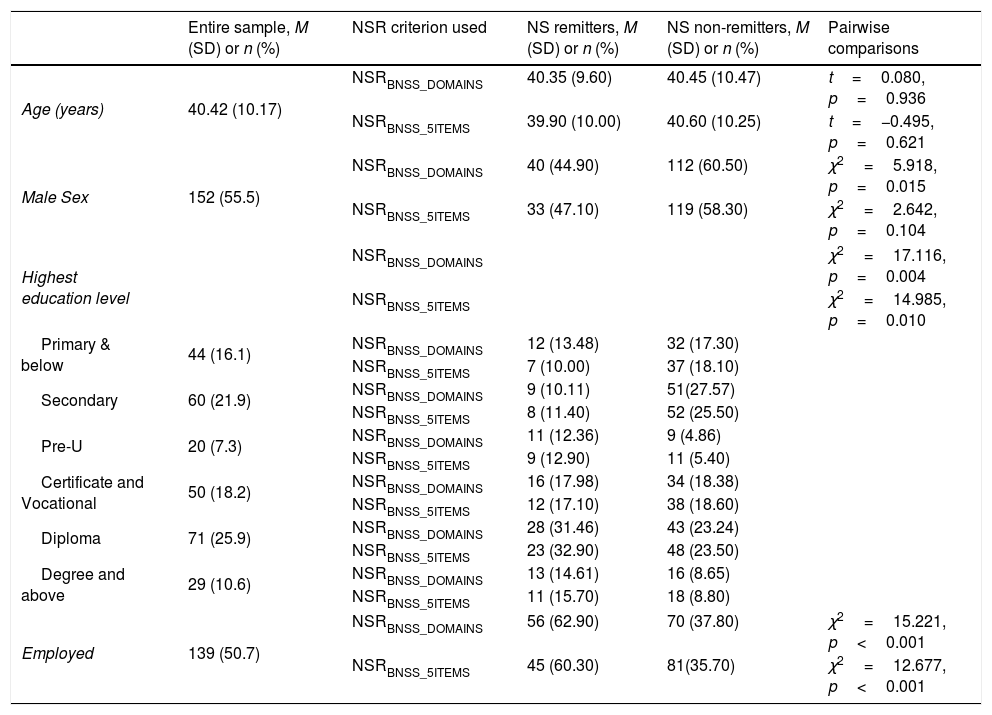
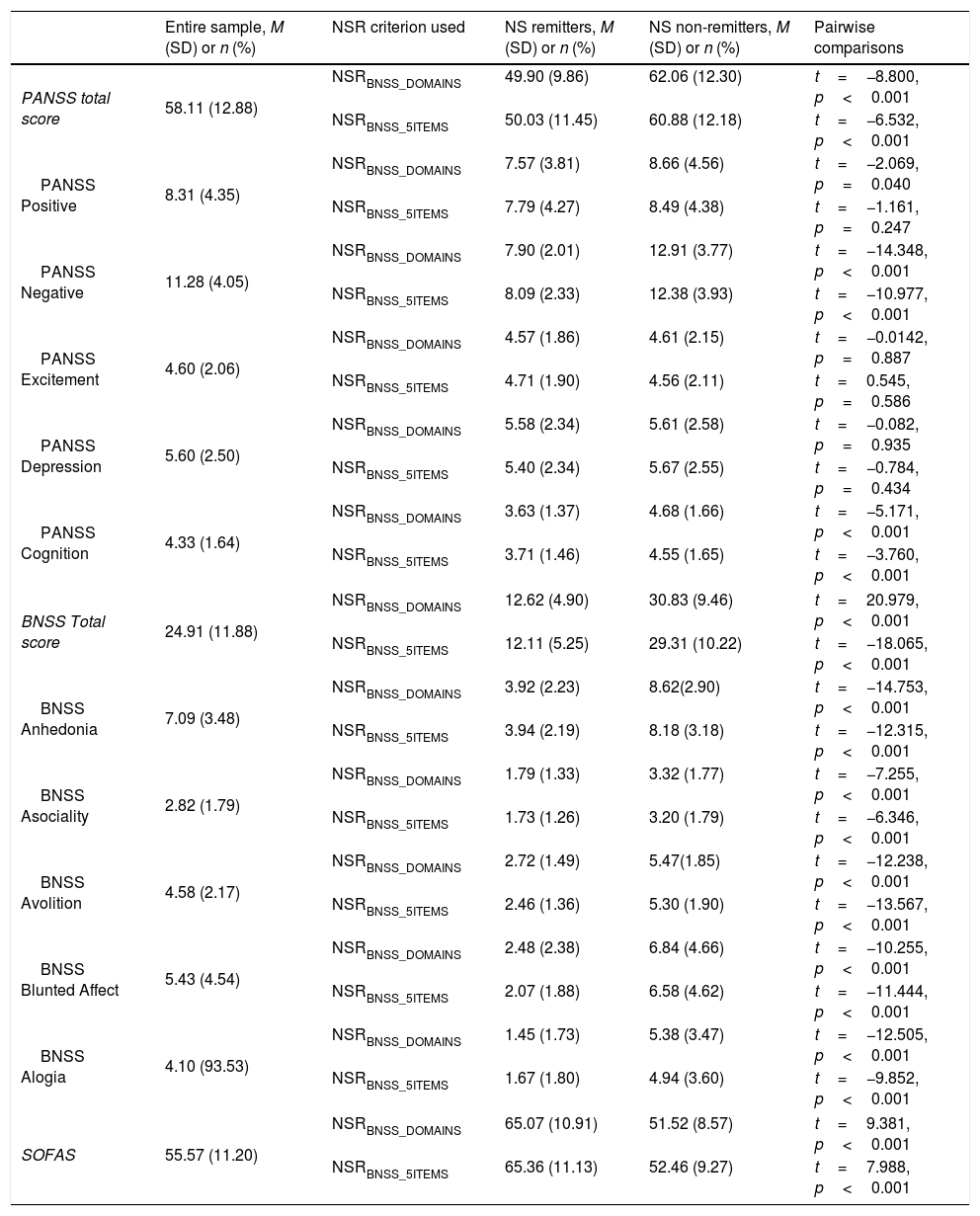
ResultsSocio-demographic and clinical characteristics of the sampleMost of the participants were of Chinese ethnicity (n=231, 84.3%). 174 (62.0%) of them were educated above secondary level, and almost half (n=126, 46.0%) of the study participants were employed (Table 1). The mean PANSS total score was 58.11 (SD=12.88) which suggested mild-moderate severity of schizophrenia.48 The SOFAS score ranged from 35 to 90, with a mean of 55.57 (SD=11.20), which suggested moderate difficulty in social, occupational or school functioning (Table 2).
Socio-demographic characteristics of study participants.
| Entire sample, M (SD) or n (%) | NSR criterion used | NS remitters, M (SD) or n (%) | NS non-remitters, M (SD) or n (%) | Pairwise comparisons | |
|---|---|---|---|---|---|
| Age (years) | 40.42 (10.17) | NSRBNSS_DOMAINS | 40.35 (9.60) | 40.45 (10.47) | t=0.080, p=0.936 |
| NSRBNSS_5ITEMS | 39.90 (10.00) | 40.60 (10.25) | t=−0.495, p=0.621 | ||
| Male Sex | 152 (55.5) | NSRBNSS_DOMAINS | 40 (44.90) | 112 (60.50) | χ2=5.918, p=0.015 |
| NSRBNSS_5ITEMS | 33 (47.10) | 119 (58.30) | χ2=2.642, p=0.104 | ||
| Highest education level | NSRBNSS_DOMAINS | χ2=17.116, p=0.004 | |||
| NSRBNSS_5ITEMS | χ2=14.985, p=0.010 | ||||
| Primary & below | 44 (16.1) | NSRBNSS_DOMAINS | 12 (13.48) | 32 (17.30) | |
| NSRBNSS_5ITEMS | 7 (10.00) | 37 (18.10) | |||
| Secondary | 60 (21.9) | NSRBNSS_DOMAINS | 9 (10.11) | 51(27.57) | |
| NSRBNSS_5ITEMS | 8 (11.40) | 52 (25.50) | |||
| Pre-U | 20 (7.3) | NSRBNSS_DOMAINS | 11 (12.36) | 9 (4.86) | |
| NSRBNSS_5ITEMS | 9 (12.90) | 11 (5.40) | |||
| Certificate and Vocational | 50 (18.2) | NSRBNSS_DOMAINS | 16 (17.98) | 34 (18.38) | |
| NSRBNSS_5ITEMS | 12 (17.10) | 38 (18.60) | |||
| Diploma | 71 (25.9) | NSRBNSS_DOMAINS | 28 (31.46) | 43 (23.24) | |
| NSRBNSS_5ITEMS | 23 (32.90) | 48 (23.50) | |||
| Degree and above | 29 (10.6) | NSRBNSS_DOMAINS | 13 (14.61) | 16 (8.65) | |
| NSRBNSS_5ITEMS | 11 (15.70) | 18 (8.80) | |||
| Employed | 139 (50.7) | NSRBNSS_DOMAINS | 56 (62.90) | 70 (37.80) | χ2=15.221, p<0.001 |
| NSRBNSS_5ITEMS | 45 (60.30) | 81(35.70) | χ2=12.677, p<0.001 | ||
NSRBNSS_DOMAINS, Negative symptom remission (NSR) based on Brief Negative Symptom Scale (BNSS) domains; NSRBNSS_5ITEMS, NSR based on BNSS 5 items.
Clinical characteristics of study participants.
| Entire sample, M (SD) or n (%) | NSR criterion used | NS remitters, M (SD) or n (%) | NS non-remitters, M (SD) or n (%) | Pairwise comparisons | |
|---|---|---|---|---|---|
| PANSS total score | 58.11 (12.88) | NSRBNSS_DOMAINS | 49.90 (9.86) | 62.06 (12.30) | t=−8.800, p<0.001 |
| NSRBNSS_5ITEMS | 50.03 (11.45) | 60.88 (12.18) | t=−6.532, p<0.001 | ||
| PANSS Positive | 8.31 (4.35) | NSRBNSS_DOMAINS | 7.57 (3.81) | 8.66 (4.56) | t=−2.069, p=0.040 |
| NSRBNSS_5ITEMS | 7.79 (4.27) | 8.49 (4.38) | t=−1.161, p=0.247 | ||
| PANSS Negative | 11.28 (4.05) | NSRBNSS_DOMAINS | 7.90 (2.01) | 12.91 (3.77) | t=−14.348, p<0.001 |
| NSRBNSS_5ITEMS | 8.09 (2.33) | 12.38 (3.93) | t=−10.977, p<0.001 | ||
| PANSS Excitement | 4.60 (2.06) | NSRBNSS_DOMAINS | 4.57 (1.86) | 4.61 (2.15) | t=−0.0142, p=0.887 |
| NSRBNSS_5ITEMS | 4.71 (1.90) | 4.56 (2.11) | t=0.545, p=0.586 | ||
| PANSS Depression | 5.60 (2.50) | NSRBNSS_DOMAINS | 5.58 (2.34) | 5.61 (2.58) | t=−0.082, p=0.935 |
| NSRBNSS_5ITEMS | 5.40 (2.34) | 5.67 (2.55) | t=−0.784, p=0.434 | ||
| PANSS Cognition | 4.33 (1.64) | NSRBNSS_DOMAINS | 3.63 (1.37) | 4.68 (1.66) | t=−5.171, p<0.001 |
| NSRBNSS_5ITEMS | 3.71 (1.46) | 4.55 (1.65) | t=−3.760, p<0.001 | ||
| BNSS Total score | 24.91 (11.88) | NSRBNSS_DOMAINS | 12.62 (4.90) | 30.83 (9.46) | t=20.979, p<0.001 |
| NSRBNSS_5ITEMS | 12.11 (5.25) | 29.31 (10.22) | t=−18.065, p<0.001 | ||
| BNSS Anhedonia | 7.09 (3.48) | NSRBNSS_DOMAINS | 3.92 (2.23) | 8.62(2.90) | t=−14.753, p<0.001 |
| NSRBNSS_5ITEMS | 3.94 (2.19) | 8.18 (3.18) | t=−12.315, p<0.001 | ||
| BNSS Asociality | 2.82 (1.79) | NSRBNSS_DOMAINS | 1.79 (1.33) | 3.32 (1.77) | t=−7.255, p<0.001 |
| NSRBNSS_5ITEMS | 1.73 (1.26) | 3.20 (1.79) | t=−6.346, p<0.001 | ||
| BNSS Avolition | 4.58 (2.17) | NSRBNSS_DOMAINS | 2.72 (1.49) | 5.47(1.85) | t=−12.238, p<0.001 |
| NSRBNSS_5ITEMS | 2.46 (1.36) | 5.30 (1.90) | t=−13.567, p<0.001 | ||
| BNSS Blunted Affect | 5.43 (4.54) | NSRBNSS_DOMAINS | 2.48 (2.38) | 6.84 (4.66) | t=−10.255, p<0.001 |
| NSRBNSS_5ITEMS | 2.07 (1.88) | 6.58 (4.62) | t=−11.444, p<0.001 | ||
| BNSS Alogia | 4.10 (93.53) | NSRBNSS_DOMAINS | 1.45 (1.73) | 5.38 (3.47) | t=−12.505, p<0.001 |
| NSRBNSS_5ITEMS | 1.67 (1.80) | 4.94 (3.60) | t=−9.852, p<0.001 | ||
| SOFAS | 55.57 (11.20) | NSRBNSS_DOMAINS | 65.07 (10.91) | 51.52 (8.57) | t=9.381, p<0.001 |
| NSRBNSS_5ITEMS | 65.36 (11.13) | 52.46 (9.27) | t=7.988, p<0.001 | ||
NSRBNSS_DOMAINS, Negative symptom remission (NSR) based on Brief Negative Symptom Scale (BNSS) domains; NSRBNSS_5ITEMS, NSR based on BNSS 5 items; PANSS, Positive and Negative Syndrome Scale; SOFAS, Social and Occupational Functioning Assessment Scale.
Around one-third (n=89, 32.5%) of the participants fulfilled NSRBNSS_DOMAINS criterion. Seventy (25.6%) participants fulfilled NSRBNSS_5ITEMS criterion.
Prevalence of FR and its association with NS scores and NSRData on SOFAS was missing for 33 participants. Of the remaining 241 participants, 61 (25.3%) were in FR. Univariate logistic regressions showed that the likelihood of FR was highest with lower scores on Avolition (OR=0.395, 95% CI=0.306–0.510, p<0.001), followed by Asociality (OR=0.345, 95% CI=0.253–0.469, p<0.001), Anhedonia (OR=0.655, 95% CI=0.579–0.740, p<0.001), Alogia (OR=0.838, 95% CI=0.763–0.921, p<0.001) and Blunted Affect (OR=0.863, 95% CI=0.799–0.933, p<0.001).
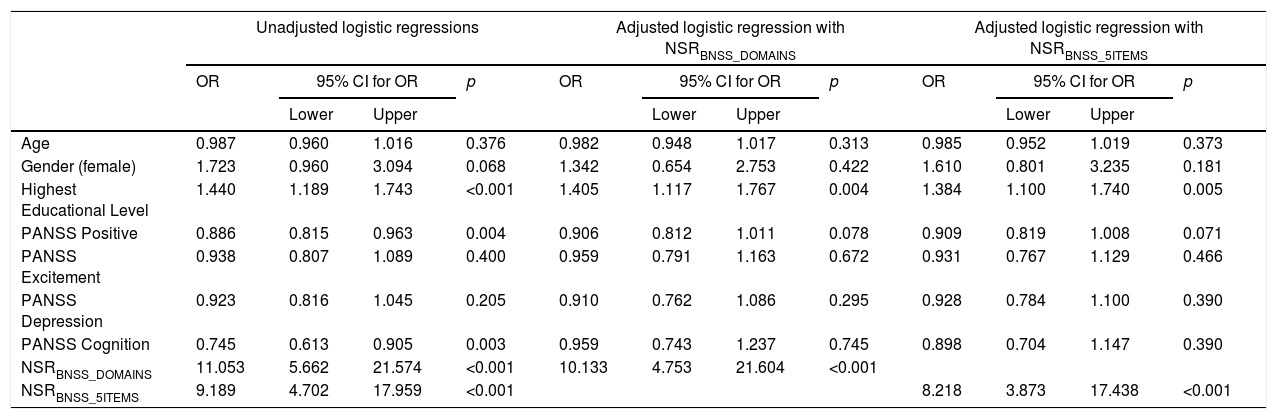
In univariate logistic regression analyses, FR was significantly associated with NSRBNSS_DOMAINS (Unadjusted OR=11.053, 95% CI=5.662–21.574, p<0.001) and NSRBNSS_5ITEMS (Unadjusted OR=9.189, 95% CI=4.702–17.959, p<0.001). The association between FR and NSRBNSS_DOMAINS remained significant (Adjusted OR=10.133, 95% CI=4.753–21.604, p<0.001) when the model was adjusted for covariates. FR was also associated with highest educational level of the participants (Adjusted OR=1.405, 95% CI=1.117–1.767, p=0.004). Similarly, in the model using NSRBNSS_5ITEMS, after adjusting for covariates, FR was significantly associated with NSRBNSS_5ITEMS (Adjusted OR=8.218, 95% CI=3.873–17.438, p<0.001) and highest education level (Adjusted OR=1.384, 95% CI=1.100–1.740, p=0.005) (see Table 3).
Logistic regressions to examine the association between functional remission and negative symptom remission.
| Unadjusted logistic regressions | Adjusted logistic regression with NSRBNSS_DOMAINS | Adjusted logistic regression with NSRBNSS_5ITEMS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI for OR | p | OR | 95% CI for OR | p | OR | 95% CI for OR | p | ||||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| Age | 0.987 | 0.960 | 1.016 | 0.376 | 0.982 | 0.948 | 1.017 | 0.313 | 0.985 | 0.952 | 1.019 | 0.373 |
| Gender (female) | 1.723 | 0.960 | 3.094 | 0.068 | 1.342 | 0.654 | 2.753 | 0.422 | 1.610 | 0.801 | 3.235 | 0.181 |
| Highest Educational Level | 1.440 | 1.189 | 1.743 | <0.001 | 1.405 | 1.117 | 1.767 | 0.004 | 1.384 | 1.100 | 1.740 | 0.005 |
| PANSS Positive | 0.886 | 0.815 | 0.963 | 0.004 | 0.906 | 0.812 | 1.011 | 0.078 | 0.909 | 0.819 | 1.008 | 0.071 |
| PANSS Excitement | 0.938 | 0.807 | 1.089 | 0.400 | 0.959 | 0.791 | 1.163 | 0.672 | 0.931 | 0.767 | 1.129 | 0.466 |
| PANSS Depression | 0.923 | 0.816 | 1.045 | 0.205 | 0.910 | 0.762 | 1.086 | 0.295 | 0.928 | 0.784 | 1.100 | 0.390 |
| PANSS Cognition | 0.745 | 0.613 | 0.905 | 0.003 | 0.959 | 0.743 | 1.237 | 0.745 | 0.898 | 0.704 | 1.147 | 0.390 |
| NSRBNSS_DOMAINS | 11.053 | 5.662 | 21.574 | <0.001 | 10.133 | 4.753 | 21.604 | <0.001 | ||||
| NSRBNSS_5ITEMS | 9.189 | 4.702 | 17.959 | <0.001 | 8.218 | 3.873 | 17.438 | <0.001 | ||||
NSRBNSS_DOMAINS, Negative symptom remission (NSR) based on Brief Negative Symptom Scale (BNSS) domains; NSRBNSS_5ITEMS, NSR based on BNSS 5 items; PANSS, Positive and Negative Syndrome Scale.
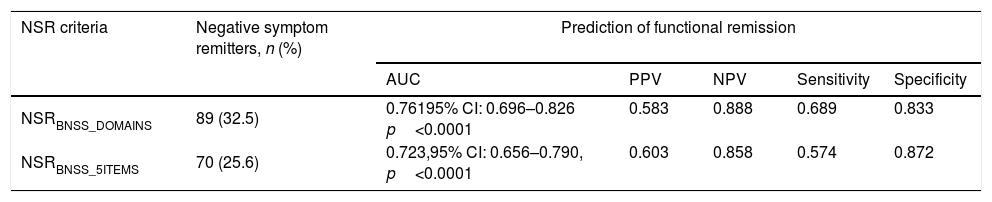
The AUC, PPV, NPV, sensitivity and specificity of the two NSR criteria to predict FR were adequate (Table 4). To predict FR, the AUC for NSRBNSS_DOMAINS and NSRBNSS_5ITEMS were 0.761 (CI: 0.696–0.826, p<0.001) and 0.723 (CI: 0.656–0.790, p<0.001), respectively. Pair-wise comparisons showed that there were no significant differences between the AUCs for NSRBNSS_DOMAINS vs. NSRBNSS_5ITEMS (z=1.685, p=0.0919). Both NSR criteria demonstrated a fair ability to discriminate between functional remitters and non-remitters.49–51 The two NSR criteria had substantial agreement with each other (Kappa statistic=0.797).52
Prediction of functional remission by negative symptom remission.
| NSR criteria | Negative symptom remitters, n (%) | Prediction of functional remission | ||||
|---|---|---|---|---|---|---|
| AUC | PPV | NPV | Sensitivity | Specificity | ||
| NSRBNSS_DOMAINS | 89 (32.5) | 0.76195% CI: 0.696–0.826 p<0.0001 | 0.583 | 0.888 | 0.689 | 0.833 |
| NSRBNSS_5ITEMS | 70 (25.6) | 0.723,95% CI: 0.656–0.790, p<0.0001 | 0.603 | 0.858 | 0.574 | 0.872 |
NSR, Negative Symptom Remission; NSRBNSS_DOMAINS, NSR based on BNSS domains; NSRBNSS_5ITEMS, NSR on based BNSS 5 items; AUC, Area under the curve; PPV, Positive predictive value; NPV, Negative predictive value.
Comparisons on socio-demographic and clinical variables between NS remitters and non-remitters are shown in Tables 1 and 2, respectively. When NSRBNSS_DOMAINS criterion was used, as compared to non-remitters, NS remitters were less likely to be males (χ2=5.918, p=0.015) and more likely to be employed (χ2=15.221, p<0.001). In comparison to non-remitters, NSR remitters had significantly lower scores on PANSS positive (t=−2.069, p=0.040), PANSS negative (t=−14.348, p<0.001) and PANSS cognition (t=−5.171, p<0.001) and significantly higher scores on SOFAS (t=9.381, p<0.001). Similar results were observed when NSRBNSS_5ITEMS was used to define NSR, except that the proportion of males (χ2=2.642, p=0.104) and PANSS positive scores (t=−1.161, p=0.247) were not significantly different between remitters and non-remitters.
DiscussionThe present study proposed 2 criteria for NSR in schizophrenia using the BNSS – NSRBNSS_DOMAINS and NSRBNSS_5ITEMS. Both criteria had substantial agreement with each other and were significantly associated with FR. Additionally, both NSR criteria showed a fair ability to discriminate between functional remitters vs. non-remitters. We discuss and compare the strengths and weaknesses of the two NSR criteria.
The proposed NSRBNSS_DOMAINS criterion took into account the severity of all items across the 5 domains of NS. Though the approach to average the item scores might dilute the impact of high-scoring items within the relevant domain, conceptually, the NSRBNSS_DOMAINS seemed to be a rigorous criterion for remission as all concepts of NS were captured. An individual had to be well in all 5 domains of NS to fulfil criteria for NSR. Another advantage of the NSRBNSS_DOMAINS was that unlike the SANS or PANSS NSR criteria,6 it took into consideration internal motivation for asociality and avolition, and anticipatory anhedonia,44,53 all of which were suggested to be important symptoms by the National Institute of Mental Health (NIMH).8 Additionally, NSRBNSS_DOMAINS showed a fair ability to predict FR.
However, time might be a limitation in the application of this criterion in clinical practice. Clinicians might not be able to spare the required time of 20–25min to ascertain this criterion for an individual patient in a busy practice. Therefore, we suggest that the NSRBNSS_DOMAINS would be more useful in research or clinical trial settings where the outcome entails a robust evaluation of NSR and time is less of a limiting factor.
Next, we proposed the NSRBNSS_5ITEMS criterion to overcome the limitation of the NSRBNSS_DOMAINS criterion, i.e., long duration of its assessment which is not feasible in clinical practice. The NSRBNSS_5ITEMS had an important representative item from each domain of the BNSS. Hence, similar to the NSRBNSS_DOMAINS, it took into consideration all the domains of NS, but it could be done in much less time, leading to ease of its application in clinical settings. Its substantial agreement with NSRBNSS_DOMAINS suggested that it may be similarly rigorous to predict NSR. Moreover, similar to NSRBNSS_DOMAINS, the NSRBNSS_5ITEMS also showed a fair ability to predict FR. We suggest that this criterion can be used in routine clinical care when a quick assessment of NSR is required.
NSR based on any of the two NSR criterion was found to be significantly associated with FR, providing support to the validity of these criteria.35,42 NS have significant association with impairments in functioning in all areas in individuals with schizophrenia; therefore, improvement in NS should lead to an improvement in functioning or a higher likelihood to achieve FR.29–31,54 This is supported by evidence that therapies like cognitive-behavioural social skills training which target NS also lead to an improvement in functioning in individuals with schizophrenia.55 This study also found that the likelihood of FR was highest with lower severity of Avolition, followed by Asociality domains of NS assessed on the BNSS. Previous literature suggested that Avolition and Asociality were the key domains associated with functional outcome in schizophrenia16,56,57; therefore, less severe Avolition and Asociality may be associated with better functioning or higher likelihood of FR.
Comparison of NS remitters vs. non-remitters showed that when NSRBNSS_DOMAINS was used, rates of NSR were significantly higher among females when compared to males. This is consistent with previous research; females were reported to have lower severity of NS and better prognosis when compared to males with schizophrenia.58–60 This relationship between gender and NSR was not significant when NSRBNSS_5ITEMS criterion was used, nonetheless, proportion of females was higher in the remitted group. Further, NSR remitters based on either of the NSR criterion were more likely to have a higher level of education than non-remitters. This is in line with previous reports in schizophrenia that individuals with higher educational attainment had lower levels of NS.61 NSR non-remitters were also found to have significantly lower rates of employment when compared to NS remitters. NS were reported to have a negative effect on both supported and non-supported employment in schizophrenia62 which explains this finding. NS remitters also had significantly lower scores on positive and cognitive symptoms when compared to non-remitters based on NSRBNSS_DOMAINS criterion. Although not significant, the PANSS positive scores were lower for NS remitters when compared to non-remitters based on the NSRBNSS_5ITEMS criterion. Previous literature suggested that NS were correlated with positive63,64 and cognitive symptoms65,66 in schizophrenia. This is consistent with the findings in this study that NS remitters also had lower scores on positive and cognitive symptoms when compared to non-remitters.
To our knowledge, this is the first study examining the applicability of the BNSS to define NSR. Though NS are closely related to functioning and independent living in schizophrenia, they may be neglected in presence of positive symptoms which are more obvious and may require more urgent management.67,68 However, last few decades have witnessed a surge in research on NS, especially on NS rating scales and management of NS.11,69 An NSR outcome measure could provide useful insights for clinicians regarding management of schizophrenia. Moreover, NSR criteria would be a useful outcome measure in clinical trials to investigate the efficacy of new treatments or interventions for negative symptoms in schizophrenia.
The main limitation of our study was that due to its cross-sectional nature, participants were not followed-up to determine the duration or stability of NSR. In other words, we were not able to capture if there were changes in severity of negative symptoms over time, which may change the status of a NS remitter to non-remitter and vice versa. This may affect the validity of the study results. Another drawback of the cross-sectional design of the study was that investigation of the predictors of NSR was not possible. Secondly, the study recruited only outpatients who had mild-moderate severity of NS; thus, further research is needed to explore if the NSR criteria proposed in this study can be applied to patients with more severe NS. Additionally, the approaches to derive the NSR criteria would need to be validated in other samples before they can be further implemented. Lastly, in this study, the validity of the proposed BNSS NSR criteria was investigated by examining their association with FR. A limitation of this method is that the association between functioning and NS was suggested to be somewhat tautological; items assessing behaviours related to NS (especially apathy) in NS rating scales had content which overlapped significantly with measures of functioning or functional decline.45,70 Nonetheless, with the inclusion of items related to internal experience and motivation in the BNSS, it can be argued that NS assessed on the BNSS and functioning would have less overlap or correlation.
In conclusion, our study results suggest that both the NSRBNSS_DOMAINS and NSRBNSS_5ITEMS criteria are capable to define NSR in schizophrenia. Depending on the setting and needs, clinicians and researchers might employ either the full BNSS or an abbreviated 5-item BNSS scale to identify NSR. More research is needed to further examine the validity of these criteria in schizophrenia.
Funding sourceThis study was supported by the Singapore Ministry of Health's National Medical Research Council under the Centre Grant Programme (Grant No.: NMRC/CG/004/2013). Dr. Lee is supported by the Ministry of Health National Medical Research Council Clinician Scientist Award (MOH-000013).
Authors contributionsGR and JL designed the original study and wrote the protocol. GR and MSA conducted data collection. GR conducted literature review, data analyses, and wrote the first draft of the manuscript. MSA, CYH, EF-E, BK and JL gave substantial comments and edited the manuscript. All authors contributed to the manuscript and approved the final manuscript.
Conflict of interestsDr. Kirkpatrick receives licensing royalties from ProPhase LLC for use of the Brief Negative Symptom Scale (BNSS) by for-profit groups; these fees are donated to the Brain and Behaviour Research Foundation. He has also received honoraria and travel support from ProPhase LLC for training pharmaceutical company raters on the BNSS; consulting fees and/or travel support from Lundbeck, Acadia, ProPhase LLC, Otsuka, and Minerva Neurosciences; and fees from anonymized investors through Guideposts and Decision Resources Group. He is part owner of Quantic Innovations, which provides services related to digital phenotyping. Dr. Lee has received honoraria from Otsuka and Janssen. The remaining authors have no conflict of interest to declare.