The increase in telemedicine in the mental health field has led to psychometric instruments changing from paper-and-pencil administration to an electronic format. A study is performed to determine if both formats are equivalent for well-known questionnaires such as GHQ-12, WHO-5, and PHQ-9.
Material and methodsForty-seven volunteers completed GHQ-12, WHO-5 and PHQ-9 questionnaires in paper-and-pencil format, and in the following 24h they completed their electronic versions via the web site www.memind.net. An electronic-Likert format was used by 24 participants, and 23 used an electronic-slider format. Internal consistency was measured by α-Cronbach index and omega coefficient, and test–retest was measured by the intraclass correlation coefficient (ICC). Agreement between individual items was compared using weighted Kappa coefficients, and dimensional structure between formats using the Comparative Fit Index (CFI).
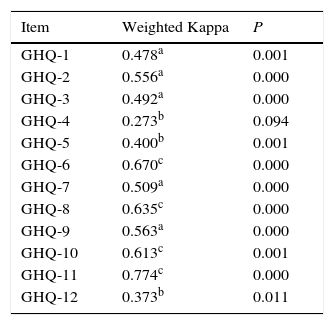
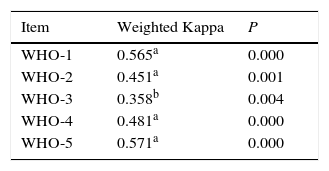
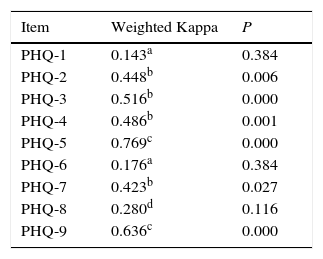
ResultsInternal consistency was higher than 0.8 for GHQ-12 and WHO-5. The ICC ranged between 0.655 for PHQ-9 paper-and-pencil/electronic-slider and 0.901 for GHQ-12 paper-and-pencil/electronic-slider. Agreement for individual items in paper-and-pencil and electronic-Likert versions was variable, ranging from low agreement in PHQ-1 (weighted κ=0.143; P=.384) to high agreement in PHQ-5 (weighted κ=0.769; P=.000). The CFI results showed an adequate equivalence between formats.
ConclusionsExcept for the PHQ-9 electronic-Likert, questionnaires keep their structure in electronic formats. Discrepancies were found in items agreement. This study supports previous works indicating that the change from paper-and-pencil to electronic formats is not an immediate process, and needs a proper adaptation.
El auge de la telemedicina en el campo de la salud mental está haciendo que el uso de instrumentos psicométricos, tradicionalmente basados en un soporte de «lápiz-y-papel», se adapte al formato electrónico. El objetivo de este trabajo es verificar si los 2 formatos de conocidos instrumentos como las escalas GHQ-12, WHO-5 y PHQ-9 son intercambiables.
Material y métodosCuarenta y siete voluntarios completaron los cuestionarios GHQ-12, WHO-5 y PHQ-9 en papel y en las siguientes 24h en su versión electrónica a través de la web www.memind.net (24 en formato electrónico-Likert y 23 en formato electrónico-slider). Se midió la consistencia interna mediante el índice α-Cronbach y el coeficiente omega, la fiabilidad test-retest mediante el coeficiente de correlación intraclase (CCI), el grado de acuerdo de los ítems mediante el coeficiente kappa ponderado y comparamos la estructura dimensional de los 2 formatos con el índice de ajuste comparativo (IAC).
ResultadosLa consistencia interna de los instrumentos fue mayor de 0,8 para todos los instrumentos a excepción del PHQ-9. Los CCI oscilaron entre 0,655 para PHQ-9 lápiz-y-papel/electrónico-slider y 0,901 para GHQ-12 lápiz-y-papel/electrónico-slider. El acuerdo entre los ítems en las versiones en lápiz-y-papel y electrónica-Likert fue variable, desde acuerdos muy bajos en el del ítem PHQ-1 (κ ponderada=0,143; p=0,384) hasta acuerdos altos en el ítem PHQ-5 (κ ponderada=0,769; p=0,000). La equivalencia arrojada con el IAC fue adecuada.
ConclusionesCon la excepción del PHQ-9 electrónico-Likert, los cuestionarios mantienen su estructura en la versión electrónica. Encontramos discrepancias en el acuerdo entre los ítems, lo que apoya la idea de que el paso de un instrumento diseñado en papel al medio digital no es un proceso automático, sino que requiere un proceso de adaptación y de verificación sobre el tipo de diseño en formato electrónico.
In recent years telecommunications and computer technologies have entered the field of healthcare, giving rise to a new discipline that has been called “telemedicine”.1 Telemedicine has also reached mental health and is now a growth area.2 A field of special interest is the evaluation of symptoms using electronic tools such as computers, smartphones or wearables,3 so that what was classically studied in the psychometric field using “pencil-and-paper” now uses an electronic format. Different studies have found that participants feel more comfortable with electronic questionnaires, answering the questions more easily and losing fewer data than occurs with paper questionnaires.4–7
When psychometric instruments are used in populations with characteristics different from the ones they were created for, a validation and adaptation process is necessary.8 Likewise, in the migration from pencil-and-paper format to an electronic one, some initiatives attempt to show that both formats are equivalent instead of directly assuming that they are so.9
At the current time the literature supports the idea that pencil-and-paper questionnaires and electronic ones will supply equivalent data in patient-reported measurements of the results in clinical trials4,10 as well as when they are used as psychometric instruments. Thus three reviews study the comparative reliability of the pencil-and-paper and electronic versions of approximately 50 psychometric instruments — fundamentally for anxiety and depression — finding good reliability in general, although with discrepancies in some questionnaires.11–13
When psychometric questionnaires measure degree of agreement with a phrase, the answers are often shown in a Likert-type scale, with a certain number of options from greater to lesser degree of agreement. Analogue visual scales are an alternative to these questionnaires, as described by Hayes and Patterson in 1921.14 In these the interviewee expresses his degree of agreement with the question on a lineal graph. The characteristics of the electronic format facilitate using an analogue visual format like a line, along which the interviewee can select the point that best represents his answer by sliding the mouse (the “slider”). Analogue visual or slider-type scales have been shown to be a good alternative in electronic/online questionnaires15,16 and they make them simpler and faster to administer as well as easier to understand.17
A specific area of psychometrics consists of using self-administered questionnaires to screen for mental disorders. In the age of telemedicine having reliable electronic versions of instruments of this type would make it easier for a population increasingly familiar with technology to access them. This is especially important if we take the population of digital natives into account.18 They are starting to use health services, while the majority of the professionals who deal with them are digital immigrants.18
Our aim here is to analyse whether the screening questionnaires in the General Health Questionnaire (GHQ-12), the Well-Being Index of the World Health Organisation (WHO-5) and the Patient Health Questionnaire (PHQ-9) have the same psychometric properties as the pencil-and-paper version in their electronic-Likert and electronic-slider forms. Our hypothesis is that the pencil-and-paper and electronic versions of each one of these scales will be interchangeable.
Material and methodsParticipants and procedureThe sample consisted of 47 non-clinical volunteers aged from 18 to 24 years old. The majority of them were women (35 in all), and they were divided into 2 groups of 24 and 23 participants. All of them were Nursing Degree students in the Universidad Autónoma, Madrid.
In May 2016 the participants answered a self-administered interview that included the paper version of the following screening instruments: GHQ-12, WHO-5 and PHQ-9, in their corresponding classrooms after the last class in the morning. All of the students consented to take part. The questionnaires were completed anonymously, and no reward of any type was given. After the students had returned the questionnaires to the researcher, they were given access keys to the multi-platform tool www.memind.net, where they filled out the electronic versions of the same questionnaires in the following 24h. 24 filled out an electronic-Likert version and 23 filled out an electronic-slider version.
This study was approved by the clinical research ethics committee of the Hospital Universitario Fundación Jiménez Díaz. After being informed of the nature of the study, all of the participants gave their informed consent in writing prior to taking part. The results have been presented following the transparency declaration proposed by Catalá-López et al.19,20
InstrumentsThe questionnaires used were the 12-item version of the GHQ-12,21 the WHO-522 and the PHQ-9 depression screening questionnaire.23
The participants first filled out the original versions in pencil-and-paper and then subsequently completed the electronic versions–developed by us–in electronic-Likert and electronic-slider formats.
The General Health Questionnaire (GHQ-12)This is a self-administered questionnaire, designed for use in clinical circles to detect individuals with possible psychiatric disorders. It is composed of 12 items, 6 formulated positively and 6 negatively, which are answered on a Likert-type 4 point scale. The replies, which score from 0 to 3, are: “more than usual”, “the same as usual” and “much less than usual” for the positive questions, and “no, not at all”, “no more than usual” “somewhat more than usual” and “much more than usual” for the negative items. Higher scores indicate worse health. Different models have been developed for scoring: the standard method (GHQ-0011), corrected scoring (GHQ-0111) and Likert scoring (GHQ-0123).
The standard method is considered to be the most suitable for case identification; this gives a score of from 0 to 12, with the cut-off point located between 2 and 324; this was the method used in the comparison between the pencil-and-paper and electronic-Likert formats. The GHQ-0123 score was used for the group of participants which compared the pencil-and-paper version and the electronic-slider one.
The GHQ-12 has been validated in 15 countries and it achieves good reliability, with Cronbach's alphas from 0.82 to 0.86.25 In the Spanish population, different studies have found good reliability in the general population, with Cronbach's alphas from 0.7626 to 0.86.25
The WHO well-being index (WHO-5)This self-administered scale with 5 items is used to measure the feeling of well-being. The 5 phrases it contains have the particularity that they are all expressed positively. They are: (1) “I feel happy and in a good mood”, (2) “I feel peaceful and relaxed”, (3) “I have felt active and energetic”, (4) “I woke up fresh and rested”, and (5) “My everyday life has been full of things which interest me”. It is available gratis in several languages at http://www.who-5.org/. For each one of the items, the degree of well-being is scored for the 2 previous weeks on a Likert-type scale from 0 (never) to 5 (all of the time); the total score varies from 0 to 25, so that the highest scores are associated with a stronger feeling of well-being, while scores below 13 have been linked to depression.27
The WHO-5 is a scale used around the world and not only in the field of mental health, but also in general healthcare. It has been proven to be suitably valid as a screening tool for depression and as a means of measuring evolution in several clinical trials.27 Specifically, in a study of an active adult European population which included Spanish population, its internal consistency amounted to 0.82 (Cronbach's alpha),28 while in a Spanish population over the age of 65 years old its internal consistency was 0.86.29 In the last available European quality of life survey, in 2012, the average score in Spain was 65.4.30
The Patient-9 Health Questionnaire (PHQ-9)This is a self-administered questionnaire that is used for depression screening. It is composed of 9 items formulated based on the diagnostic criteria for depression of the DSM-IV; each item scores from 0 to 3 (0=no day; 1=several days; 2=more than half of the days, and 3=almost every day). Although there are other ways of scoring, when it is used as a depression screening tool the total score of the PHQ-9 is calculated by adding up the score for each item, and it varies from 0 to 27; scores above 10 indicate moderate to high levels of depression.23
The usefulness of the PHQ-9 as a depression screening tool has been shown to be equal to or even greater than those of other measures of depression, and it obtained a good level of validity in different studies.31 More specifically, Kroenke et al.23 reported an internal consistency for the PHQ-9 of from 0.86 to 0.89. In Spain, Diez-Quevedo et al. validated the PHQ-9 in 1003 hospitalised patients, showing good agreement between the diagnoses using the PHQ-9 and clinical diagnoses (kappa=0.74; total precision, 88%; sensitivity, 87%; specificity, 88%).32 in the Spanish-speaking population the validation study in the Mexican population stands out; in 55,000 women in the Mexican Teachers’ Cohort the questionnaire was found to have a high level of internal consistency, with a Cronbach's alpha of 0.89.33
MEmind Wellness TrackerThe MEmind Wellness Tracker tool was used for the electronic administration of the scales. It was developed in the Psychiatry Department of the Hospital Universitario Fundación Jiménez Díaz. This web application is available at www.memind.net, and it works with all types of internet-access devices (computers, tablets and smartphones) using any operating system. The website has 2 interfaces, one for the researcher and the other for the user. Once they had given the researcher the printed questionnaire, the students were registered in the website and given access keys (users and password), after which the researcher randomly assigned them one of the 2 types of electronic questionnaire programmed to be completed in the following 24h.
After accessing the platform and filling out the questionnaires, the data were stored in a secure server and encrypted using Secure Socket Layer/Transport Layer Security (SSL/TLS). Only the head researcher (EBG) has access to the server. MEmind uses encrypted keys with 256 bit codes based on the AES-256 algorithm. An external auditor guarantees that these levels of security comply with the maximum requisites of the data protection law.
Statistical analysisStatistical analysis was performed using version 23.0 of the SPSS package.34 Firstly, given the small size of the sample and the absence of normality, the scores were compared in each one of the scales in the pencil-and-paper and electronic versions using Wilcoxon's signed range test. Then the reliability was calculated using consistency and agreement indexes. Cronbach's alpha was used to measure the internal consistency of the questionnaires in both formats. Additionally, and given the limitations of the alpha coefficient pointed out by several authors, the omega coefficient was also calculated.35 The intraclass correlation coefficient (ICC) was used to estimate test–retest reliability; ICC values under 0.4 indicate low reliability, at from 0.4 to 0.75 they indicate from mediocre to good reliability, and above 0.75 they indicate excellent reliability.33 The degree of agreement between the different items in the pencil-and-paper and electronic-Likert versions of the questionnaires was measured using weighted kappa coefficients, and to interpret them the criteria proposed by Landis and Koch were used, according to which values lower than 0 indicate a poor level of agreement, values from 0.01 to 0.20 indicate slight agreement, from 0.21 to 0.40 a reasonable level of agreement, a moderate agreement from 0.41 to 0.60, from 0.61 to 0.80 a strong agreement and from 0.81 to 1.00 an almost perfect agreement.36 Lastly, to compare the pencil-and-paper and electronic models, and thereby compare their dimensional structure, we calculate the comparative fit index (CFI) for the 3 scales evaluated.
ResultsThe switch from a pencil-and-paper format to an electronic-Likert oneThere were no differences between the pencil-and-paper and electronic versions in any of the scales: GHQ-12 (Z=−1.709; P=.087); WHO-5 (Z=−1.067; P=.286) and PHQ-9 (Z=−0.199; P=.842), with the following average scores for each one of them: 1.96±2.66 in pencil-and-paper vs 1.50±2.55 in electronic format for the GHQ-12; 13.63±2.66 in pencil-and-paper vs 14.42±4.03 in electronic format for the WHO-5, and 4.87±2.80 in pencil-and-paper vs 4.83±2.85 in electronic format for the PHQ-9.
Internal consistencyCronbach's alpha coefficients for the GHQ-12, WHO-5 and PHQ-9 in pencil-and-paper were 0.872, 0.774 and 0.586, respectively, and for the electronic GHQ-12, WHO-5 and PHQ-9 they were 0.835, 0.835 and 0.654. Additionally, the omega coefficients for the GHQ-12, WHO-5 and PHQ-9 in pencil-and-paper were 0.900, 0.900 and 0.720, respectively, and for the electronic versions of the GHQ-12, WHO-5 and PHQ-9 they were 0.890, 0.900 and 0.730.
Test–retest reliabilityThe ICC between the pencil-and-paper and electronic versions of the different scales were 0.802 (P<.001) for the GHQ-12, 0.726 (P<.001) for the WHO-5 and 0.682 (P<.001) for the PHQ-9.
Agreement between individual itemsIn the GHQ-12 questionnaire the agreement between the items was reasonable at the least and even high for several of them (Table 1). For the WHO-5, except for item 3 that was reasonable, the agreement between the items was moderate (Table 2). Finally, for the PHQ-9, except for items PHQ-1 and PHQ-6, in which the level of agreement was low, the level of agreement was at least reasonable and even high for items PHQ-5 and PHQ-9 (Table 3).
Agreement between the items for the GHQ-12 questionnaire.
There were no statistically significant differences between both versions when the WHO-5 and PHQ-9 scales were compared: WHO-5 (Z=−0.974; P=.330) and PHQ-9 (Z=−1,601; P=.109). Statistically significant differences were found between both versions of the GHQ-12 (Z=−2.294; P=.022).
Internal consistencyThe Cronbach's alpha coefficients for the GHQ-12, WHO-5 and PHQ-9 scales in pencil-and-paper were 0.768, 0.881 and 0.655, respectively, and for the electronic versions of the GHQ-12, WHO-5 and PHQ-9 scales they were 0.901, 0.872 and 0.836.
Test–retest reliabilityThe ICC between the pencil-and-paper and electronic versions of the different scales was 0.616 (P=.002) for the GHQ-12, 0.594 (P=.001) for the WHO-5 and 0.584 (P=.011) for the PHQ-9.
Equivalence between the pencil-and-paper and electronic formatsTo compare the pencil-and-paper and electronic models we calculate the CFI and the corresponding mean squared error of approximation (MSEA).
For the pencil-and-paper GHQ-12 the CFI was 0.420 and the MSEA was 0.252, and for the electronic GHQ-12 the CFI was 0.420 and the MSEA was 0.257. For the pencil-and-paper WHO-5 the CFI was 0.888 and the MSEA was 0.216, and for the electronic WHO-5 the CFI was 0.888 and the MSEA was 0.213. For the pencil-and-paper PHQ-9 the CFI was 0.708 and the MSEA was 0.150, and for the electronic PHQ-9 the CFI was 0.708 and the MSEA was 0.150.
DiscussionExcept for the pencil-and-paper and electronic-Likert PHQ-9, all of the instruments presented sufficient internal consistency to ensure the reliability of the scales. Respecting test–retest reliability, although this was good for both formats it was greater in the electronic-Likert format than it was in the switch to the electronic-slider format. In the switch from the pencil-and-paper format to electronic-Likert, only 2 items in the GHQ-12 and one in the PHQ-9 achieved a high level of agreement while the level of agreement was low for the other items. The equivalence between the pencil-and-paper and electronic formats was sufficient.
Our results support the views of other authors in previous works, who found that although the level of equivalence between pencil-and-paper and electronic questionnaires is acceptable in general, this migration is neither completely equivalent nor immediate,11–13 and it must take place using certain agreed norms.9
Comparing the reliability of our results with the previous validated versions in Spanish populations or Spanish speaking ones — all of the versions to be completed using pencil-and-paper — we can state that the internal consistency of the GHQ-12 questionnaire is similar to that of the validations in the general Spanish population (Cronbach's alpha at 0.762 and 0.862); in our case all of the formats have good internal consistency, while the electronic-slider one is especially good in this respect (Cronbach's alpha=0.901). Similarly, the internal consistency of the different formats of the WHO-5 questionnaire used in our study was good (Cronbach's alpha higher than 0.80 in all cases) and it was at the same level as the previous studies, with a European study of active population with part of the Spanish sample (Cronbach's alpha=0.82)28 or a study in a Spanish population over the age of 65 years old (Cronbach's alpha=0.86).29 In the case of the PHQ-9 we are unable to compare the internal consistency with that corresponding to the Spanish validation, but it is of interest to point out that it is lower than in both of the other questionnaires; Cronbach's alpha is only higher than 0.80 for the electronic-slider format, while for the others it stands at a value of around 0.60, which is clearly lower than the internal consistency found in Spanish-speaking populations, with a Cronbach's of 0.89 in Mexican women31 or 0.835 in primary care patients in Chile.37
Respecting the scores in the questionnaires of our sample in pencil-and-paper as well as electronic formats, the participants are classified as “healthy”. Nevertheless, it is striking that (except for the slider format GHQ-12–the different formats of the GHQ-12 and WHO-5 approach the cut-off point to be considered cases: strictly more than 2 for the GHQ (GHQ-0011) and less than 13 for the WHO. However, in the PHQ-9 they do not reach the cut-off point for depression in any of the formats. Although it is outside our field of interest for this study, these indicative scores should lead us to reflect on the self-perception of health and well-being felt by health sciences students: some studies link academic overload with stress, anxiety and depression,38 and these questionnaires were administered in the month of May, which is traditionally exam time.
In spite of the increasingly widespread use of electronic forms, few studies have research their equivalence as we do here. More specifically, of the 3 questionnaires that we used, only for the PHQ-9 has one group studied its electronic version; we found no similar studies for the WHO-5 or the GHQ-12, although we did for the GHQ-28. Respecting the PHQ-9, in 2013 Bush et al.39 compared the psychometric properties of different health measurements in 45 serving soldiers in a United States military installation. These included the PHQ-9 questionnaire, and they were completed in paper, computer and smartphone. As in our case, the average scores obtained in each format were similar, and they were also in a similar range (around a score of 5). Nevertheless, the internal consistency that they found is greater than our figures: 0.79 for paper, 0.85 for computers and 0.87 for smartphones in their study. This compares with our figures of 0.58 for paper (compared with electronic-Likert), 0.65 for paper (compared with the electronic-slider), 0.65 for the electronic-Likert and 0.84 for the electronic-slider. It is only for the latter format that our scores reach the same level as theirs, while our reliability is low for the others. Thus in this study they found a higher level of test–retest reliability than we did, with an ICC=0.94 for paper-computer and 0.92 for paper-smartphone, which are clearly higher than our figures (0.68 for paper-Likert and 0.58 for paper-slider). Respecting the GHQ-12, although we found no study of the validity of its electronic format, in a sample of 185 psychology students in Madrid Vallejo et al.40 studied the validity of the electronic format of the GHQ-28, and they found both formats are interchangeable. They report a Cronbach's alpha of 0.90 for both formats and good test–retest reliability (r=0.69). Our Cronbach's alphas are high too, and the electronic-slider format (0.901) is the one that is closest to theirs. Our test–retest reliability is even higher than theirs, with an ICC=0.802.
We would like to underline the novelty of our work as one of its strong points, as although paper is disappearing few groups have considered studying the validity of the electronic versions of the most widely used psychometric questionnaires. Moreover, we found no works that studied the questionnaires we used in analogue visual format, which is the most suitable for electronic questionnaires.15,16 In spite of these strong points, our work also has limitations. Some of these are its small sample size and the non-representative nature of the same, as it was conveniently recruited in a Spanish university. These results can therefore not be extrapolated to the general population. Nor did we take socio-economic status into account, or whether the students had psychiatric diagnoses or other health problems, or whether they consumed substances; nor do we know the support that they used (web, telephone or tablet, etc.) to fill out the electronic versions. Further studies are therefore required in the future with larger and more varied samples.
ConclusionsOur findings show that we are able to assume the equivalence of the electronic formats of the GHQ-12 and WHO-5 questionnaires, although in the case of the PHQ-9 prudence is required. Moreover, slider formats were found to be a valid alternative to Likert-style questionnaires in the electronic environment. The switch from an instrument designed on paper to using it in an electronic medium is not an automatic process that requires no adaptation, so that every instrument which migrates to another support and method of administration must be validated before it is used, more so if it is expected to be used clinically.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were conducted in human beings or animals for this research.
Confidentiality of dataThe authors declare that no patient or participant data appear in this paper.
Right to privacy and informed consentThe authors declare that no patient or participant data appear in this paper.
FinancingThe financial support for this work was supplied in part by subsidies from the ISCIII PI13/02200 FIS projects, the National Drugs Plan 2015I073 and the PapiitIN108216 grant. The financing agreement guarantees the independence of the authors in the study design, the interpretation of data and the writing and publication of the report.
Conflict of interestsThe authors have no conflict of interests to declare.
The Nursing School of the Fundación Jiménez Díaz. Universidad Autónoma de Madrid.
Psychiatry Department, IIS-Fundación Jiménez Díaz, Madrid, Spain. Universidad Autónoma de Madrid, Spain: Irene Caro-Cañizares, Mónica Jiménez-Giménez, Juncal Sevilla-Vicente, Olga Bautista, Sara María Bañón-González, María Luz Palacios, María Natalia Silva, Jaime Chamorro-Delmo, Marta González- Granado, Sergio Sánchez-Alonso, Ernesto José Verdura-Vizcaíno, Miren Iza, Lucía Villoria-Borrego, Sonia Carollo-Vivian, Rocío Navarro-Jiménez, Laura Mata-Iturralde, Javier Fernández-Aurrecoechea, Santiago Ovejero, Laura Muñoz-Lorenzo, Alba Rodriguez-Jover, Jorge Hernán Hoyos Marín, Carolina Vigil-López, Ana Rico-Romano, Rodrigo Carmona, Susana Amodeo-Escribano, Ana López-Gómez, Margarita Pérez-Fominaya, Covadonga Bonal-Giménez, Rosa Ana Bello-Sousa, Ruth Polo-del Rio, Pedro Gutiérrez-Recacha, Iratxe Tapia-Jara, Marta Migoya-Borja, Elsa Arrua, Antonio Vian-Lains, Elena Hernando-Merino, Nora Palomar-Ciria, Leticia Serrano-Marugán, Alba Sedano-Capdevila, Marisa Herraiz, María Constanza Vera-Varela, Silvia Vallejo-Oñate.
Psychiatry Department, Hospital Universitario Infanta Elena, Valdemoro, Madrid, Spain: Rosana Codesal-Julián, Luis Sánchez-Pastor, Edurne Crespo-Llanos, Ainara Frade Ciudad, Marisa Martin-Calvo.
Psychiatry Department, Hospital Universitario Rey Juan Carlos, Móstoles, Madrid, Spain: Laura de Andrés-Pastor, Pablo Puras-Rico, Miriam Agudo-Urbanos, Diego Laguna-Ortega, Sara Clariana-Martín, Eduardo Reguera-Nieto, Teresa Legido-Gil, María Guadalupe García-Jiménez, Raquel Álvarez-García, Pablo Portillo-de Antonio, Eva María Romero-Gómez Sara González-Granado.
Psychiatry Department, Hospital General de Villalba, Collado Villalba, Madrid, Spain: Ana Alcón-Durán, Juan Manuel García-Vega, Yago Cebolla-Meliá, Ezequiel Di Stasio, Pedro Martín-Calvo, Ana José Ortega.
Hospital 12 de Octubre, Madrid, Spain: Luis Agüera-Ortiz, Javier Rodríguez-Torresano, Javier Sanz-Fuentenebro, Miguel Ángel Jiménez-Arriero.
AGC Salud Mental, Área Sanitaria 3, Avilés, Asturias, Spain: Natalia Bretón-Díez, Juan José Martínez-Jambrina, Emilia García-Castro, María Fernández-Rodríguez, Mónica Álvarez-Villechenous.
MEmind Study Group collaborators are provided in Annex.
Please cite this article as: Barrigón ML, Rico-Romano AM, Ruiz-Gomez M, Delgado-Gomez D, Barahona I, Aroca F, et al. Estudio comparativo de los formatos en lápiz y papel y electrónicos de los cuestionarios GHQ-12, WHO-5 y PHQ-9. Rev Psiquiatr Salud Ment (Barc). 2017;10:160–167.