There is increasing evidence relating the presence of depression in seniors and the risk of hospital admission in medical departments from the Emergency Services.
ObjectiveTo determine the impact of antidepressant treatment (ATD) as a protective factor for emergency hospitalisation in older people.
MethodAll patients aged 65 and over who required urgent attention for medical reasons at the Emergency Department of the Corporació Sanitària i Universitària Parc Taulí (Sabadell, Barcelona, Spain) for the period between January and October 2012 were included in the study. Sociodemographic variables, alcohol and tobacco use, medical history and psychopharmacological treatment were obtained. The necessary sample size was calculated and a simple randomisation was performed. Subsequently, a descriptive statistical analysis and parametric tests were conducted.
ResultsA total of 674 patients (53% women) were evaluated, with a mean age of 78.45 years, and 27.6% of the cases (71% women) were receiving ATD. Among the 333 admitted patients (50%), 83 individuals (24.6%) had previously received ATD; this contrasts with the 103 cases (30.6%) of prior ATD treatment among the patients who were not admitted. After comparative analysis, the relationship between previous use of ATD and being admitted to hospital was not statistically significant in our global sample. This relationship was only statistically significant among the group aged 75 and over (neg. sig. 0.012).
ConclusionsIn our study, ATD was associated with a decreased risk of hospital admission for urgent medical conditions in people aged 75 and over. Treating depression may protect the elderly against admission to the Emergency department and may potentially be a quality criterion in preventing complications in this population.
Existe una creciente evidencia acerca de la interrelación entre presencia de depresión en la tercera edad y riesgo de ingreso hospitalario médico.
ObjetivoDeterminar el impacto del tratamiento antidepresivo (ATD) como factor protector de ingreso hospitalario desde Urgencias en personas mayores.
MétodoSe incluyó a personas de 65 años o mayores que acudieron por cualquier motivo a Urgencias de la Corporació Sanitària i Universitària Parc Taulí de Sabadell (Barcelona) entre enero y octubre del 2012. Se obtuvieron datos sociodemográficos básicos, consumo de alcohol y tabaco, antecedentes y tratamiento actual. Se realizó el cálculo de tamaño muestral y una aleatorización simple. Posteriormente se realizó un análisis estadístico descriptivo y pruebas paramétricas.
ResultadosSe evaluó a 674 pacientes (53% mujeres), con una edad media de 78,45 años. Un 27,6% de los casos (71% mujeres) recibían tratamiento antidepresivo. Del total de 337 pacientes ingresados (50%), 83 individuos (24,6%) utilizaban previamente ATD, mientras que entre los no ingresados, utilizaban ATD el 30,6%. Tras el análisis comparativo, se objetivó una relación significativa negativa entre recibir ATD y riesgo de ingreso solo en aquellos pacientes de 75 años o mayores (sig. 0,012).
ConclusionesEn nuestro estudio, el tratamiento antidepresivo se relaciona con una disminución del riesgo de ingreso hospitalario urgente por enfermedad médica en personas de 75 años o mayores. El tratamiento de la depresión en personas mayores podría tener efecto protector general frente a la severidad de las enfermedades atendidas en Urgencias en nuestra población y puede suponer un criterio de calidad en orden a prevenir complicaciones.
Depression is a highly common disease among the elderly. Up to 60% of the patients admitted to a general hospital have or will have a mental health problem, including dementia, delirium or depression.1
At the same time, medical emergencies are now the first point of contact with the health care system for many patients with medical as well as psychiatric diseases.2 Chronic diseases (especially heart, respiratory or endocrinological diseases such as diabetes) and their high levels of comorbidity, including cognitive deterioration, depression and other disabilities, are significant predictors of visits to the A&E unit for elderly adults.3 Up to 2/3 of the elderly patients admitted to the A&E ward of a general hospital suffer depression or pre-existing cognitive deterioration and, in these cases, the results of their hospitalisation are poorer in terms of their survival, the duration of their admission and destination when discharged.4
To discover the real size of the problem of depression among the elderly in our European population, in 1995 the EURODEP consortium published a European scale multicentre study on the frequency of depressive disorders in older people. At that time 12% of the elderly (65 years old or older) European population were assigned a diagnosis of depression. The corresponding figure in Spain was slightly lower (10.7%).5 Given the methodological complexity that is required to estimate the incidence of depression, few studies attempt this, although it may stand at around 12% per year.6
The appearance of depression in elderly individuals with chronic diseases may lead to an increase in the number of visits to the A&E Unit, although chronic diseases are also in turn a factor that favours the appearance of depression. An increase in the severity of a disease may lead to an increase in the symptoms of depression and, if the latter is not treated correctly, they may exacerbate the physical symptoms. Due to the symptoms of their disease depressed patients are also known to often not adhere to the medical recommendations necessary to control their bodily diseases, displaying less compliance with treatment.4
In 2001 the World Health Organisation identified depression as a major direct cause of disability and underlined the importance of effective treatment and management of the condition in all areas of care.7 However, an intrinsic difficulty was found in identifying depressive disorders in the A&E Unit. This is due to several reasons, including the priority of diagnosing imminent risk and organic disease, methodological and organisational difficulties and the high pressure staff are under.8 The effects of this possible infradiagnosis of depression in the elderly are not well known, and this is even more so of the results of the same in the A&E Unit.9,10
There are in fact few studies which analyse the impact of depression (or its treatment) on the risk of hospital admission due to a medical condition among the elderly. In any case, evaluation of depressive disorder in the elderly should be implemented in all areas, and in fact several fast screening scales are already available. These could be used or validated in Spanish or other languages.11–14
A previous study by our group in the Principality of Asturias was published in 2009 and covered a broad sample of 1016 patients aged 74 years old or more (average age 87.4 years) who required complete geriatric evaluation in general hospital A&E units in our area. Up to 17.4% of cases in this study were diagnosed with depressive disorder, and 79.7% of these patients had to be admitted to hospital.15 After logistic regression analysis adjusted for different confusion factors (age, sex, marital status, institutionalisation, form of coexistence, Barthel index and cognitive deterioration), depression was independently associated with a higher risk of admission (OR: 1.83; IC 95%: 1.0–2.78). It was therefore concluded that those individuals over the age of 74 years old who visit an A&E Unit and have a previous depressive disorder are at greater risk of hospitalisation.15
A subsequent study in 2010 in north New York state care centres covered a sample of 477 patients included in a home help program, evaluating whether or not they suffered depression. The hospitalisation rates of the group of individuals with depression (77 patients) and non-depressed ones (400 patients) were similar (at around 7%). Nevertheless, the average duration of hospitalisation was longer in the group of patients with depression (19.5 vs 8.4), as well as the risk of hospitalisation during the first 2 weeks after entering the program.16
In a way that is complementary to these previous studies, the aim of this work is to determine whether prior treatment of depressive disorders in an elderly person who visits an A&E unit due to a medical cause is a protective factor against hospitalisation. This will make it possible to gain deeper knowledge of the consequences for the healthcare system of correct treatment of depressive disorders in the elderly.
Material and methodDesignAn observational, randomised, retrospective and transversal study.
Population and areaAll of the individuals aged 65 years old or over who visits the A&E Unit of the Corporació Sanitària i Universitària Parc Taulí de Sabadell (Barcelona) from January 2012 to October of the same year requiring care for medical reasons were included. The catchment area of our hospital includes 500,000 inhabitants of the city of Sabadell and the Vallés Occidental region. The population is mainly urban and works in industry and services. The A&E Unit is for general emergencies and has different levels and facilities.
During the period in question our hospital treated a total of 36,176 medical emergencies. A total of 15,791 of these were patients aged 65 years old or more (43.65%) of whom it was necessary to admit 4094 (25.93%). The analysis includes all of the patients who were evaluated and fulfilled the age criterion after excluding those patients who visited the A&E Unit on several occasions (and who may represent a population with different characteristics from the usual patients). The sample necessary to obtain significant data was calculated (95% level of confidence, α=0.05) after which the R program was used to select patients at random for the study: 7 patients who required admission were selected per week, together with 7 patients who were discharged from the A&E Unit to their home or place of residence.
VariablesBasic sociodemographic data were recorded (age and sex), together with any history of cognitive deterioration, medical history, toxic substance (alcohol and tobacco) and pharmaceuticals consumption. The use of psychopharmaceutical drugs was taken into account (antidepressants, tranquilisers, antipsychotics and benzodiazepines), as well as the doses given. The different medical units where admission took place were also recorded.
The main result variable was admission to hospital following a visit to the A&E Unit for any non-psychiatric medical reason (yes/no). The total population included was also divided according to age, to determine whether greater age had any effect. Those patients aged 75 years old or more were distinguished from the younger ones aged 65–74.
Data gatheringData were obtained from the computerised clinical histories available in the A&E Unit itself, including the data of patients treated in the Emergency Department and in different specialised departments, including the mental health centre of the Corporació. To cover the patients who had only been treated by General Practitioners the search was broadened to include the computerised clinical histories of Primary Care. Finally, all data were made anonymous before being entered and analysed.
An Excel database was created to enter the variables, after which the SPSS 21.0 program was used to analyse them statistically.
Statistical analysisThe study variables were analysed descriptively in terms of frequency, percentage, average and standard deviation. P<.05 was considered to be statistically significant. After this either the Chi-squared or Student t-test was used to interrelate the different variables and check their statistical relationship.
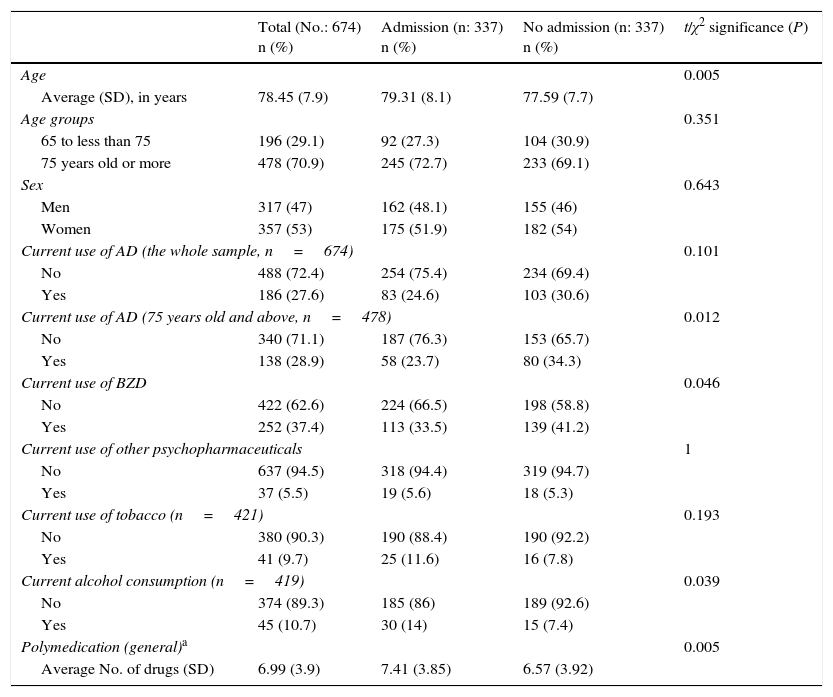
Results674 patients were selected after randomisation during the period from January to October 2012. They were then divided into 2 groups according to whether or not they had been admitted to hospital or not after visiting the A&E Unit. Their average age was 78.45 years old (SD 7.93) and 53% of the sample were women. The characteristics of both samples are described in Table 1. Of the total number of patients who were hospitalised (337 patients), 83 individuals (24.6%) had previously taken antidepressant treatment, while 30.6% (103 cases) of those who were not admitted (337 patients) had taken this type of drug.
Characteristics of the population and results.
| Total (No.: 674) n (%) | Admission (n: 337) n (%) | No admission (n: 337) n (%) | t/χ2 significance (P) | |
|---|---|---|---|---|
| Age | 0.005 | |||
| Average (SD), in years | 78.45 (7.9) | 79.31 (8.1) | 77.59 (7.7) | |
| Age groups | 0.351 | |||
| 65 to less than 75 | 196 (29.1) | 92 (27.3) | 104 (30.9) | |
| 75 years old or more | 478 (70.9) | 245 (72.7) | 233 (69.1) | |
| Sex | 0.643 | |||
| Men | 317 (47) | 162 (48.1) | 155 (46) | |
| Women | 357 (53) | 175 (51.9) | 182 (54) | |
| Current use of AD (the whole sample, n=674) | 0.101 | |||
| No | 488 (72.4) | 254 (75.4) | 234 (69.4) | |
| Yes | 186 (27.6) | 83 (24.6) | 103 (30.6) | |
| Current use of AD (75 years old and above, n=478) | 0.012 | |||
| No | 340 (71.1) | 187 (76.3) | 153 (65.7) | |
| Yes | 138 (28.9) | 58 (23.7) | 80 (34.3) | |
| Current use of BZD | 0.046 | |||
| No | 422 (62.6) | 224 (66.5) | 198 (58.8) | |
| Yes | 252 (37.4) | 113 (33.5) | 139 (41.2) | |
| Current use of other psychopharmaceuticals | 1 | |||
| No | 637 (94.5) | 318 (94.4) | 319 (94.7) | |
| Yes | 37 (5.5) | 19 (5.6) | 18 (5.3) | |
| Current use of tobacco (n=421) | 0.193 | |||
| No | 380 (90.3) | 190 (88.4) | 190 (92.2) | |
| Yes | 41 (9.7) | 25 (11.6) | 16 (7.8) | |
| Current alcohol consumption (n=419) | 0.039 | |||
| No | 374 (89.3) | 185 (86) | 189 (92.6) | |
| Yes | 45 (10.7) | 30 (14) | 15 (7.4) | |
| Polymedication (general)a | 0.005 | |||
| Average No. of drugs (SD) | 6.99 (3.9) | 7.41 (3.85) | 6.57 (3.92) | |
AD: antidepressants; BZD: benzodiazepines; SD: standard deviation.
Both of the groups studied (admitted vs not admitted) are comparable in terms of sex but not for age, as the patients who were admitted were significantly older than those who were not (79.31 years old vs 77.59 years old).
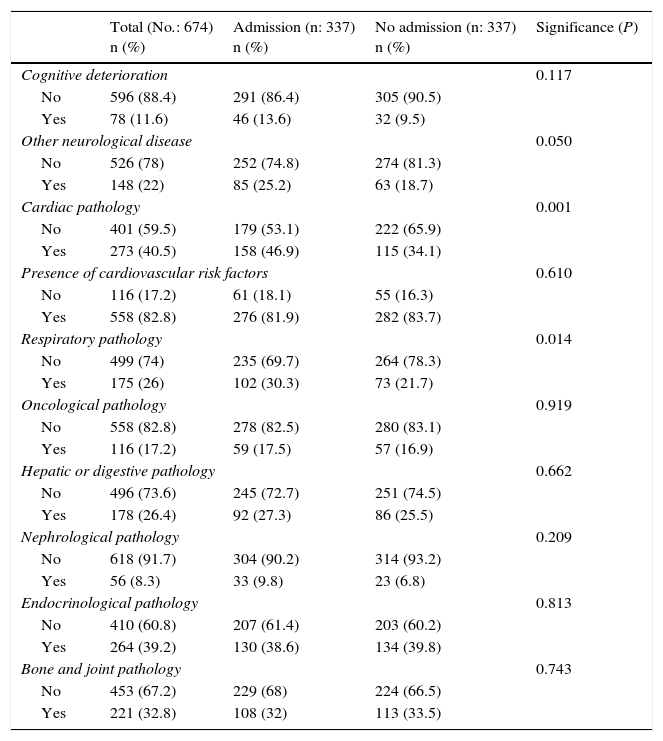
The most frequent causes of visits to the A&E Unit were respiratory (23.4%), followed by heart disease (15.7%) and hepatodigestive disease (12.3%) (Table 2). The clinical histories of 11.6% of patients had recorded cognitive deterioration. A history of cardiovascular, respiratory or neurological disease was associated with a significant risk of admission (Table 2). Likewise, the patients who were hospitalised had a significantly higher consumption of multiple medication and alcohol (Table 1).
Somatic pathologies.
| Total (No.: 674) n (%) | Admission (n: 337) n (%) | No admission (n: 337) n (%) | Significance (P) | |
|---|---|---|---|---|
| Cognitive deterioration | 0.117 | |||
| No | 596 (88.4) | 291 (86.4) | 305 (90.5) | |
| Yes | 78 (11.6) | 46 (13.6) | 32 (9.5) | |
| Other neurological disease | 0.050 | |||
| No | 526 (78) | 252 (74.8) | 274 (81.3) | |
| Yes | 148 (22) | 85 (25.2) | 63 (18.7) | |
| Cardiac pathology | 0.001 | |||
| No | 401 (59.5) | 179 (53.1) | 222 (65.9) | |
| Yes | 273 (40.5) | 158 (46.9) | 115 (34.1) | |
| Presence of cardiovascular risk factors | 0.610 | |||
| No | 116 (17.2) | 61 (18.1) | 55 (16.3) | |
| Yes | 558 (82.8) | 276 (81.9) | 282 (83.7) | |
| Respiratory pathology | 0.014 | |||
| No | 499 (74) | 235 (69.7) | 264 (78.3) | |
| Yes | 175 (26) | 102 (30.3) | 73 (21.7) | |
| Oncological pathology | 0.919 | |||
| No | 558 (82.8) | 278 (82.5) | 280 (83.1) | |
| Yes | 116 (17.2) | 59 (17.5) | 57 (16.9) | |
| Hepatic or digestive pathology | 0.662 | |||
| No | 496 (73.6) | 245 (72.7) | 251 (74.5) | |
| Yes | 178 (26.4) | 92 (27.3) | 86 (25.5) | |
| Nephrological pathology | 0.209 | |||
| No | 618 (91.7) | 304 (90.2) | 314 (93.2) | |
| Yes | 56 (8.3) | 33 (9.8) | 23 (6.8) | |
| Endocrinological pathology | 0.813 | |||
| No | 410 (60.8) | 207 (61.4) | 203 (60.2) | |
| Yes | 264 (39.2) | 130 (38.6) | 134 (39.8) | |
| Bone and joint pathology | 0.743 | |||
| No | 453 (67.2) | 229 (68) | 224 (66.5) | |
| Yes | 221 (32.8) | 108 (32) | 113 (33.5) | |
In our total sample (aged 65 years old and older) there was no significant relationship between receiving antidepressant treatment and emergency admission (P=.101). Nevertheless, when the population is divided into age groups the relationship is significant (and negative) in the group of patients aged 75 years old or more (χ2=6.610; gl=1; sig. 0.012) (Table 1). There is therefore an effect on admission for older populations, and this is interesting. Sex has no effect (as women are admitted the same as men) independently of antidepressant treatment. A history of heart, respiratory, oncological, neurological (other than cognitive deterioration) or nephrological disease, together with the presence of cardiovascular or traumatological risk factors, do not in themselves influence the effect of antidepressant treatment on the risk of hospitalisation. This is also the case for tobacco or alcohol consumption.
The patients previously affected by cognitive deterioration who take an antidepressant treatment are at less risk of emergency admission to hospital (χ2=9.89; gl=1; sig. 0.003). This is also the case for those previously affected by hepatodigestive disease (χ2=4.26; gl=1; sig. 0.042) and endocrinological disease (χ2=5.68; gl=1; sig. 0.023).
Within the group of those aged over 75 years old the hospitalised patients were also older (average age 83.13 years old; SD 5.8) than those who were not admitted (average age 81.52 years old, SD 5.7; sig. 0.002). Sex was not found to affect admission (χ2=0.199; gl=1; sig. 0.362). On the other hand, sex did influence the effect of antidepressant treatment. The women receiving this treatment were admitted to hospital significantly less than those who were not taking it (χ2=4.991; gl=1; sig. 0.032), while this effect was not detected in the men (χ2=1.506; gl=1; sig. 0.285).
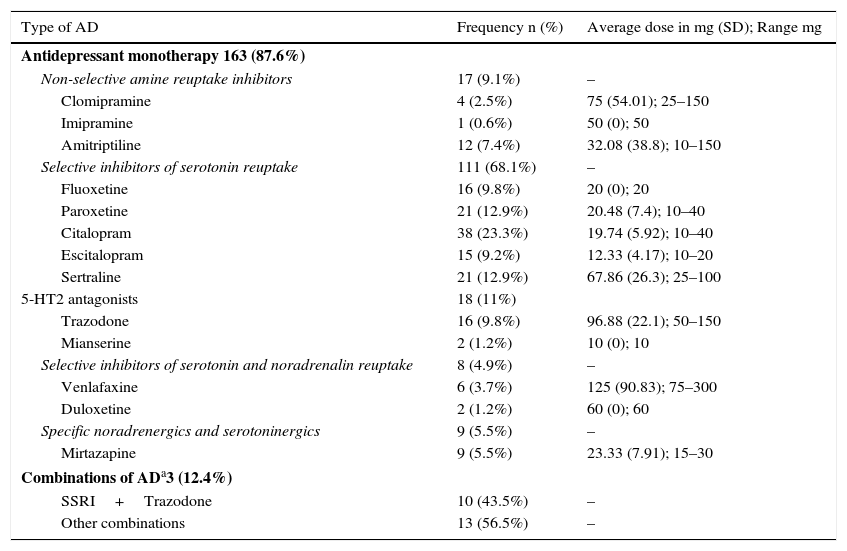
In the total sample, of the 186 patients who received antidepressant treatment, it is outstanding that 111 (68.1%) patients in the sample used selective serotonin reuptake inhibitors as a monotherapy. Citalopram is the antidepressant drug used the most widely in our sample (38 patients, 23.3%, with an average dose of 19.74mg/d; SD 5.92). Regarding frequency of use in our sample, Paroxetine and Sertraline are used 21 patients (12.9%) and Trazodone is used by 16 patients (9.8%). Table 3 shows the frequencies, average doses and ranges of the different types of antidepressant treatment used in our sample. There are no significant differences between the different groups of antidepressants in terms of whether or not patients were admitted. All of the patients in our sample were treated correctly using drugs within their therapeutic range, while considering the precautions that have to be taken with patients over the age of 65 years old.
Antidepressants used.
| Type of AD | Frequency n (%) | Average dose in mg (SD); Range mg |
|---|---|---|
| Antidepressant monotherapy 163 (87.6%) | ||
| Non-selective amine reuptake inhibitors | 17 (9.1%) | – |
| Clomipramine | 4 (2.5%) | 75 (54.01); 25–150 |
| Imipramine | 1 (0.6%) | 50 (0); 50 |
| Amitriptiline | 12 (7.4%) | 32.08 (38.8); 10–150 |
| Selective inhibitors of serotonin reuptake | 111 (68.1%) | – |
| Fluoxetine | 16 (9.8%) | 20 (0); 20 |
| Paroxetine | 21 (12.9%) | 20.48 (7.4); 10–40 |
| Citalopram | 38 (23.3%) | 19.74 (5.92); 10–40 |
| Escitalopram | 15 (9.2%) | 12.33 (4.17); 10–20 |
| Sertraline | 21 (12.9%) | 67.86 (26.3); 25–100 |
| 5-HT2 antagonists | 18 (11%) | |
| Trazodone | 16 (9.8%) | 96.88 (22.1); 50–150 |
| Mianserine | 2 (1.2%) | 10 (0); 10 |
| Selective inhibitors of serotonin and noradrenalin reuptake | 8 (4.9%) | – |
| Venlafaxine | 6 (3.7%) | 125 (90.83); 75–300 |
| Duloxetine | 2 (1.2%) | 60 (0); 60 |
| Specific noradrenergics and serotoninergics | 9 (5.5%) | – |
| Mirtazapine | 9 (5.5%) | 23.33 (7.91); 15–30 |
| Combinations of ADa3 (12.4%) | ||
| SSRI+Trazodone | 10 (43.5%) | – |
| Other combinations | 13 (56.5%) | – |
AD: antidepressant; SSRI: selective serotonin reuptake inhibitors.
The great majority of the patients are treated by their GP in their Primary Care Centre, as only 11 cases (5.91%) are treated by their Psychiatric specialist in a mental health centre.
Regarding treatment with benzodiazepines, of the 252 patients who take them, 107 patients (42.5%) are treated using Lorazepam at an average dose of 1.41mg/d (SD 1.06). In terms of frequency of Benzodiazepine use, Lormetazepam is used in 50 patients (19.8%) while Alprazolam is used in 45 patients (17.9%). There is a strong association between the use of benzodiazepines and antidepressants (χ2=44.504; gl=1; sig. 0.001).
DiscussionAlthough the consequences of the underdiagnosis of depression in the elderly for their quality of life and that of their family are known, the direct effects of depression on the healthcare system (in the consumption of healthcare resources,17,18 as well as being a risk factor for suicide)19 are not well-known for the elderly, and less still for those elderly patients who visit the A&E Unit.1,15
As was pointed out above, different studies have shown that a history of depressive disorder or the actual presence of depression are associated with an increase in the risk of hospitalisation among those aged over 74 years old who visit the A&E Unit due to a medical condition.15 In general, geriatric patients aged 65 years old or more with severe mental disorders have higher rates of visits to the A&E Unit, longer periods of hospitalisation and a high frequency of falls, alcoholism and the abuse of other substances.20 In all cases this is a population at risk that requires a holistic approach and special monitoring.
A range of risk factors for readmission in geriatric patients was found in a systematic revision in 2011. While sociodemographic factors are only able to explain risk in a few models, previous admission and the duration of hospitalisation were the factors that are relevant the most often, as were somatic morbidity and functional disability. Other factors detected in the said revision but mentioned in fewer studies include neuropsychological (or psychopathological) ones such as depression or delirium.21 We believe that psychological disorders in the elderly are under-diagnosed and under-treated, so that these aspects should be covered systematically by future revisions and studies in this area.
In 2004 an interesting prospecting and longitudinal study was conducted of predictive factors for rehospitalisation among patients aged over 60 years old who had previously been independent for their everyday activities. 194 consecutive admissions in a rehabilitation hospital were studied. The patients with depression in the base evaluation using the Geriatric Depression Scale (GDS) were at greater risk of rehospitalisation during the following 3–6 months (OR=3.549).22
Elderly patients make worse progress and have poorer general health after hospitalisation. As was shown by a broad study in 1997, the symptoms of depression may intervene in some of these negative results following discharge. In a sample of 572 hospitalised patients older than 70 years old depression symptoms, state of health and the severity of disease were measured. The main prospective evaluation measurement (discharge, 30 and 90 days) was dependency for everyday activities. The average number of depressive symptoms in the sample was 4, although patients with 6 or more symptoms of depression at admission (n=196) had a higher risk of dependency after performing the analysis and monitoring different variables, including sociodemographic ones and disease severity.23 A later study of 2006 with 380 patients older than 65 years old confirmed these findings.24 On the other hand, other studies exist which contradict these results. A study in 1999 with a sample of 165 patients older than 65 years old found that depression (scores of 9 or more in the GDS), led to a very high risk of functional deterioration in hospitalised patients (OR=3.1), although this effect disappeared in the final logistic regression model leaving the sole predictors of sex (OR=3.3), days of hospitalisation (OR=2.3), Barthel index on admission (OR=6.1) and the Cognitive Mini-Test (OR=2.7).25
One interesting datum in our analysis was the lack of a relationship between antidepressant treatment and hospital admission when the whole sample over the age of 65 years old is considered. The results of the study by Suárez et al. (2009)15 refer to a population aged 74 or more years old, so they would be comparable to those of our sample of patients aged 75 years old or more, where this association between antidepressant treatment and a reduced risk of admission is found. These data indicate a possible differential effect of depression (and its treatment) with increasing age. This effect may also be associated with a more chronic stage of both diseases (somatic and depressive).
As several previous studies have shown, an improvement arising from the treatment of depression not only improves the direct negative results of the same in geriatric patients, but also reduces the number of adverse medical events.16 The initial study by Prina et al. (2012)26 analysed a broad Dutch cohort of 8282 individuals aged 55–85 years old, taken from the “Longitudinal Aging Study Amsterdam” (LASA). After 12 months of follow-up, 14% of the individuals with depression were hospitalised for medical reasons as opposed to 10% of those who were not depressed. Depression led to a doubling of the risk of death during admission (0.8 vs 0.4%), and it was also an independent risk factor for a longer duration of hospitalisation.26
Subsequently, Prina et al. (2013) analysed a different cohort of 5411 men aged 69 years old and over who lived in Western Australia. In the multivariate analysis the presence of depression symptoms (scores of 7 or more in the GDS) was found to be an independent factor for admission to hospital for non-psychiatric reasons (44.8% vs 22.9%). It was associated with a higher number of admissions as well as longer duration of the same.27
A study in 2001 showed that the presence of depression as well as anxiety disorders was a predictive factor for readmission to hospital. This study followed up a sample of 1654 patients for one year after discharge. They were evaluated for anxiety disorders and depression using DSM-IV criteria and the Hospital Anxiety and Depression Scale (HADS). The latter is a scale that gives a very good measurement of the symptoms of anxiety and depression without being affected by the somatic symptoms of medical diseases28 which strongly affect other scales.
In our sample benzodiazepines were found to have a relevant effect. Although tranquilisers are not a suitable treatment for the symptoms of depression, (except for associated anxiety and insomnia), in our sample they were found to be protective factors, although at a lower degree of significance (Table 1). However, this effect may be simply due to the frequent association of the use of benzodiazepines with antidepressants.
Multimedication in general (the total number of drugs taken by patients for any reason, whether medical or psychiatric) is widely prevalent in our sample. It is also significantly associated with a higher rate of hospitalisation, as other authors have underlined in previous studies.29 However, we believe that this may be a result of the greater complexity or severity of the processes involved.
All of the patients in our sample were correctly treated with antidepressant drugs within their therapeutic range, and the majority (94.09%) were treated by their GP in their primary healthcare centre. This shows a considerable effort to optimise and ensure the quality of antidepressant treatments in our area.
Several previous studies in this area detected other factors that are relevant in terms of the presence of psychiatric symptoms in older patients. Specifically, Olivera et al.30 found that among other factors, the severity of physical diseases, isolation, living in a home with assistance or female sex were associated with higher prevalence of psychiatric disease. 46.1% of elderly patients had at least one psychiatric symptom, and of these 16.4% had cognitive deterioration, 15.7% anxiety, 14.3% depression, 6.1% psychotic symptoms (hallucination and delirium), 7.2% hypochondriac ideas and 4.4% obsessive symptoms. Depression was associated with the severity of physical diseases. Due to the methodology of our study we are unable to include an accumulative severity index for the medical disease of our patients, such as the Accumulative Disease Index.31 This is therefore, as we point out below, one of the limitations of the study.
To summarise, several studies have already shown the said implications and evaluated different risk factors associated with depression in the elderly. This work confirms the need to identify elderly depressive patients at an early stage, given that once they have been identified there is a high probability that they will be treated correctly at any level of the healthcare system. This may also lead to an improvement in the evolution of their somatic diseases.
Weaknesses and strengths of this studyThe fact that this study is randomised but not controlled may be considered to be its main limitation. It is not possible to determine the exact reasons or the severity of the process that led to a specific patient being prescribed an antidepressant treatment by a doctor in the past. However, logically in the majority of cases this will be due to symptoms of depression-anxiety, and less often because of other conditions such as chronic pain, where antidepressants are also occasionally used. Likewise, the heterogeneous nature of the treatments makes it impossible to clearly differentiate between pharmacological types. Nor is it possible to know the degree to which patients were depressed when they visited the A&E Unit. Some patients may have started antidepressant treatment while still suffering the symptoms of depression. In the same way, 9.8% of the patients take Trazodone, and although this is a classic antidepressant treatment, in this age group it is used above all as a hypnotic, so that this may be a confusion factor. It is also impossible to detect degree of compliance with the treatment or the relationship in time between its commencement and possible protective effect against emergency hospitalisation.
In general, other limitations of this study include the lack of standardised diagnoses, comorbidity, the functional status or severity of the patients or the fact that their level of depression was not evaluated at the moment of admission. These last two factors were taken into account in our previous study of a different sample.15
Moreover, as the study design is transversal with bivariate analysis, it is possible to establish associations but not causalities. It is impossible to establish a single independent effect of the antidepressant treatment, and nor is it possible to eliminate confusion factors associated with taking antidepressants. To be able to do so we would need a prospective, randomised and double blind design, with emergency admission to hospital as the main measure of results, while considering the standardised diagnosis of depression as the chief inclusion criterion.
The main strengths of this study are the size of its sample, the randomisation of groups and its ecological nature, given that patients arrived naturally at a public hospital department with a broad catchment area and were not selected.
ConclusionsDepression is a very common disorder among the elderly, and it has been found to have a complex and negative effect on the evolution of chronic or acute medical diseases which may occur simultaneously. Several previous studies detected an independent association between suffering depression and the risk of geriatric hospital admission due to a medical cause.
In our study antidepressant treatment is associated with a reduction in the risk of emergency hospitalisation due to a medical disease in individuals aged 75 years old or more. The correct treatment of depression in elderly individuals may therefore have a general protective effect against the severity of diseases treated in the Emergency department of our population, and it may be a quality criterion in order to prevent future complications.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments with human beings or animals were conducted for this research.
Confidentiality of dataThe authors declare that they followed the protocols of their centre of work regarding the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ortuño N, Cobo J, González E, García I, Ferrer M-D, Campos C, et al. Tratamiento antidepresivo y asociación con el ingreso urgente en unidades médicas en pacientes de 65 años o mayores. Rev Psiquiatr Salud Ment (Barc.). 2016;9:210–218.