To review the literature in order to evaluate how health professionals promote and support breastfeeding.
Data sourcesStudies from the following databases were retrieved: Scopus, PubMed, MEDLINE, Lilacs, SciELO, Web of Science and Cumulative Index to Nursing and Allied Health Literature (Cinahl). The descriptors “breastfeeding”, “professional role” and “patient care team” were used in the research. The review was limited to articles in Portuguese, Spanish, and English published between 1997 and 2013.
Data synthesisThe search retrieved 1396 studies, 18 of which were selected for being directly relevant to the main question. The review showed that breastfeeding is a challenge for health professionals, regardless of their specialization, as they have to face a demand that requires skill and sensibility, for which they are not prepared. Health professionals have considered breastfeeding a purely instinctive and biological act. Moreover, it is noticeable that many of them possess theoretical expertise on the subject, but lack the practical skills.
ConclusionsHealth professionals need to be better trained to work on promoting breastfeeding, whether by health and medical schools or by healthcare administrators, in order to consolidate multiprofessional teams committed to maternal-infant health.
Fazer uma revisão da literatura para avaliar a prática de profissionais de saúde na promoção e no apoio à amamentação.
Fontes de dadosForam identificados artigos nas bases de dados Scopus, PubMed, MEDLINE, Lilacs, SciELO, Web of Science e Cumulative Index to Nursing and Allied Health Literature (Cinahl). Para a pesquisa usaram-se os descritores “aleitamento materno” (breast feeding), “papel profissional” (professional role) e “equipe de assistência ao paciente” (patient care team). A busca limitou-se aos artigos em português, espanhol e inglês e compreendeu os anos de publicação entre 1997 e 2013.
Síntese dos dadosA pesquisa encontrou 1.396 estudos, dentre os quais foram selecionados 18 que contemplavam a pergunta norteadora. A pesquisa revelou que a amamentação é um desafio para o profissional de saúde, independentemente da área de atuação, uma vez que ele se depara com uma demanda para a qual não foi preparado e que exige sensibilidade e habilidade em seu trato. Os profissionais de saúde têm considerado a amamentação como um ato puramente instintivo e biológico. Além disso, nota-se que muitos têm domínio teórico do assunto, mas ausência do domínio prático.
ConclusõesOs profissionais de saúde precisam ser mais bem capacitados para trabalhar com a promoção do aleitamento materno, seja por meio das instituições de ensino e formação, seja por gestores da saúde, a fim de consolidar equipes multiprofissionais comprometidas com a saúde materno-infantil.
Regarding children's health, breastfeeding is essential due to its nutritional, emotional, immunological and socioeconomic benefits, and contribution to the child's development, in addition to maternal health benefits. Unfortunately, early weaning by Brazilian nursing mothers is an evident reality, but, in order to promote maternal and child health in recent years, there has been an increase in breastfeeding encouragement by health professionals and services as well as by government agencies.1
In Brazil, it can be observed that although most women start breastfeeding, more than half of the children are no longer receiving exclusive breastfeeding in the first month of life. Despite the increasing trend toward breastfeeding in the country, we are far from meeting the recommendation of the World Health Organization (WHO) on exclusive breastfeeding up to six months of life and continued breastfeeding up to the second year of life or longer.2
Rego3 indicates, as one of the causes of early weaning, the lack of information of the general population and, especially, of the health professionals. The author also affirms that the reason given for the weaning is the health team's recommendation. The percentage of misinformation dissemination is similar to the percentage of mothers who abandon breastfeeding claiming that “milk does not satisfy the baby”, which highlights the importance of the training of health professionals to increase the prevalence of breastfeeding.
Considering the experience of baby-friendly hospitals (Hospitais Amigos da Criança), there are difficulties in supporting the ten steps to successful breastfeeding, which vary from place to place. However, the results obtained with a multidisciplinary effort demonstrate their importance, not only due to the humanization of maternal and child care, but also due to the increase in exclusive breastfeeding rates that have been achieved with this program. Therefore, the Department of Breastfeeding of the Brazilian Society of Pediatrics, consisting of renowned experts in the field, supports and encourages the Baby-Friendly Hospital Initiative program in the country as an effective way to encourage and promote breastfeeding.4
The actions of breastfeeding encouragement, promotion and support should be part of the set of actions by health professionals during the prenatal, pre-delivery, and delivery periods, as well as during scheduled immunizations, newborn screening test and return to the post-partum consultation. It is essential that the health team have the role of welcoming mothers and babies, being available to listen and clarify doubts and distressing questions, encouraging the exchange of experiences and providing, whenever necessary, a unique assessment of each case.5
To obtain accurate and actual information related to the community's health, it is necessary to prioritize the personal, human and interdisciplinary characteristics of training of professionals working in the healthcare field. The appreciation of the professionals through their qualification and knowledge of the profile of each team member becomes essential for an adequate performance, improving services and thus, the user's health.6
Teamwork, individual improvement in multiple skills in the interdisciplinary context and cooperation between professionals are essential for the adequate flow of health services. Currently, the teams are becoming more important in service organizations thanks to the efficient organizational structure and use of human skills. A more global and collective view of the work becomes necessary for a better use of the skills of the professionals in relation to maternal and child health.7
It is necessary to discuss the necessities regarding breastfeeding assistance and whether such actors are performing these practical actions, in addition to verifying if they are capable of supplying this demand. The aim of this study was to identify the peculiarities indicated by literature on the importance and influence of health professionals in promoting breastfeeding.
MethodTo achieve the proposed objective, the integrative review was selected as the research method, defined by the following steps: (1) identification of the problem or issue (creation of guiding question, establishment of descriptors and criteria for inclusion/exclusion of articles); (2) sampling (selection of articles); (3) categorization of studies; (4) definition of information to be extracted from the reviewed studies; (5) analysis and discussion of the technologies used/developed, and (6) synthesis of the knowledge provided by the analyzed articles and presentation of the integrative review.8,9
The following guiding question was established: “What are the peculiarities indicated by literature on the importance of health professionals in the promotion of breastfeeding?” The inclusion criteria for this study were: the publication topic should be on the promotion of breastfeeding by health professionals; publications classified as original articles and literature reviews, published a maximum of 20 years prior to the study, published in English, Spanish, and Portuguese; complete publications with available abstracts and indexed in the Scopus, PubMed, LILACS, MEDLINE, SciELO, Web of Science and CINAHL databases. Editorials were excluded, as well as Letters to the editor, reflective studies and studies that did not cover the topic relevant to the review objective.
The search in the databases was carried out between July and October 2013, using the health terminology identified at the Descriptors of Health Sciences (DECS) and the Medical Subject Headings (Mesh), through which the following descriptors were identified: breastfeeding, professional role, and patient care.
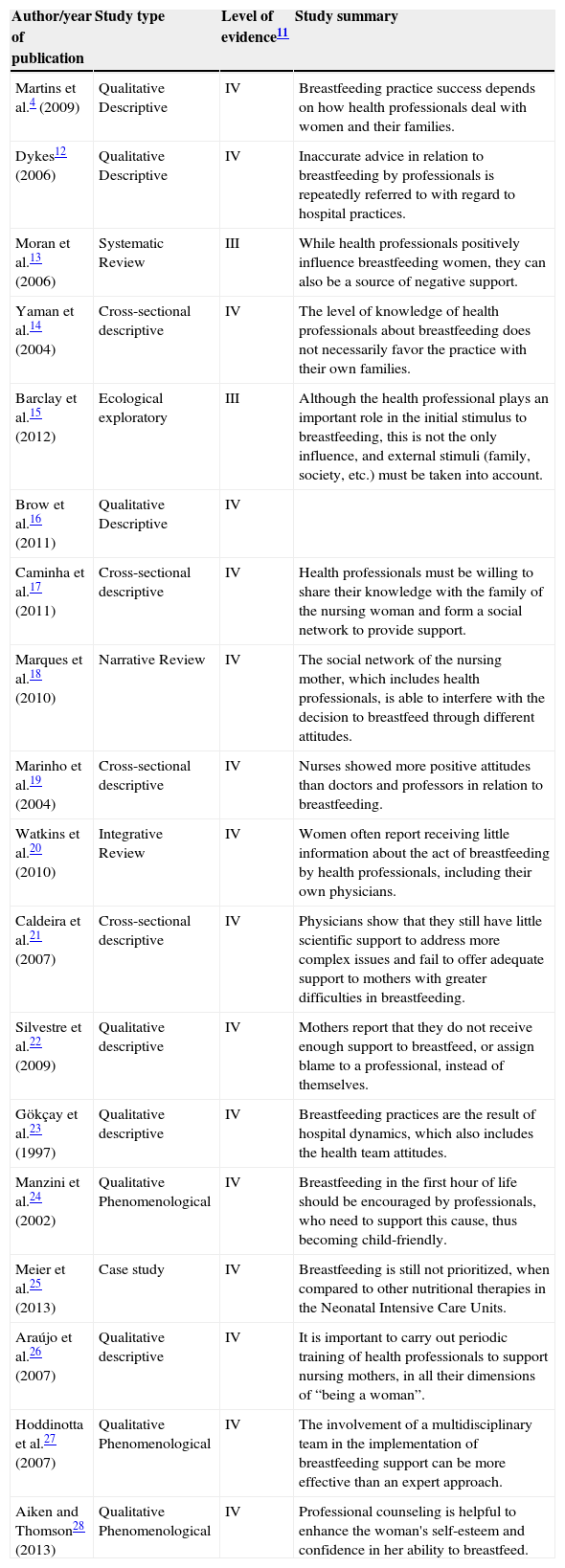
References were assessed using a form adapted from Ursi.10 This allowed the analysis of the following aspects: identification of the study (article title, journal title, authors, country, language, year of publication); journal; and methodological characteristics of the study (type of publication, technology used/developed and their target audience). The articles were arranged by year of publication and classified by levels of evidence (I–VI, with I being the highest level of evidence) according to Stetler et al.11 (Table 1). The article quality analysis was performed by two independent evaluators, who attained an agreement regarding their classification.
Summary of the main results of studies related to the practice of health professionals in breastfeeding support.
| Author/year of publication | Study type | Level of evidence11 | Study summary |
|---|---|---|---|
| Martins et al.4 (2009) | Qualitative Descriptive | IV | Breastfeeding practice success depends on how health professionals deal with women and their families. |
| Dykes12 (2006) | Qualitative Descriptive | IV | Inaccurate advice in relation to breastfeeding by professionals is repeatedly referred to with regard to hospital practices. |
| Moran et al.13 (2006) | Systematic Review | III | While health professionals positively influence breastfeeding women, they can also be a source of negative support. |
| Yaman et al.14 (2004) | Cross-sectional descriptive | IV | The level of knowledge of health professionals about breastfeeding does not necessarily favor the practice with their own families. |
| Barclay et al.15 (2012) | Ecological exploratory | III | Although the health professional plays an important role in the initial stimulus to breastfeeding, this is not the only influence, and external stimuli (family, society, etc.) must be taken into account. |
| Brow et al.16 (2011) | Qualitative Descriptive | IV | |
| Caminha et al.17 (2011) | Cross-sectional descriptive | IV | Health professionals must be willing to share their knowledge with the family of the nursing woman and form a social network to provide support. |
| Marques et al.18 (2010) | Narrative Review | IV | The social network of the nursing mother, which includes health professionals, is able to interfere with the decision to breastfeed through different attitudes. |
| Marinho et al.19 (2004) | Cross-sectional descriptive | IV | Nurses showed more positive attitudes than doctors and professors in relation to breastfeeding. |
| Watkins et al.20 (2010) | Integrative Review | IV | Women often report receiving little information about the act of breastfeeding by health professionals, including their own physicians. |
| Caldeira et al.21 (2007) | Cross-sectional descriptive | IV | Physicians show that they still have little scientific support to address more complex issues and fail to offer adequate support to mothers with greater difficulties in breastfeeding. |
| Silvestre et al.22 (2009) | Qualitative descriptive | IV | Mothers report that they do not receive enough support to breastfeed, or assign blame to a professional, instead of themselves. |
| Gökçay et al.23 (1997) | Qualitative descriptive | IV | Breastfeeding practices are the result of hospital dynamics, which also includes the health team attitudes. |
| Manzini et al.24 (2002) | Qualitative Phenomenological | IV | Breastfeeding in the first hour of life should be encouraged by professionals, who need to support this cause, thus becoming child-friendly. |
| Meier et al.25 (2013) | Case study | IV | Breastfeeding is still not prioritized, when compared to other nutritional therapies in the Neonatal Intensive Care Units. |
| Araújo et al.26 (2007) | Qualitative descriptive | IV | It is important to carry out periodic training of health professionals to support nursing mothers, in all their dimensions of “being a woman”. |
| Hoddinotta et al.27 (2007) | Qualitative Phenomenological | IV | The involvement of a multidisciplinary team in the implementation of breastfeeding support can be more effective than an expert approach. |
| Aiken and Thomson28 (2013) | Qualitative Phenomenological | IV | Professional counseling is helpful to enhance the woman's self-esteem and confidence in her ability to breastfeed. |
Then, the main data were extracted using the abovementioned tool,10 aiming at this stage to concisely organize and summarize the information on breastfeeding support by health professionals, thus creating an easily accessible and manageable database. The information included the study sample, the objectives, methodology used, results, and main findings of each study.
Thus, following the above mentioned methodological approach, the articles that addressed the guiding question of this study were selected, as well as those meeting the previously established criteria, respecting the ethical aspects related to the performance of the scientific research. The analysis of breastfeeding support actions by health professionals was carried out by assessing the methodology of each article, observing the composition of the involved professional team and the observation of the assistance demands in this area and the practice carried out by such actors.
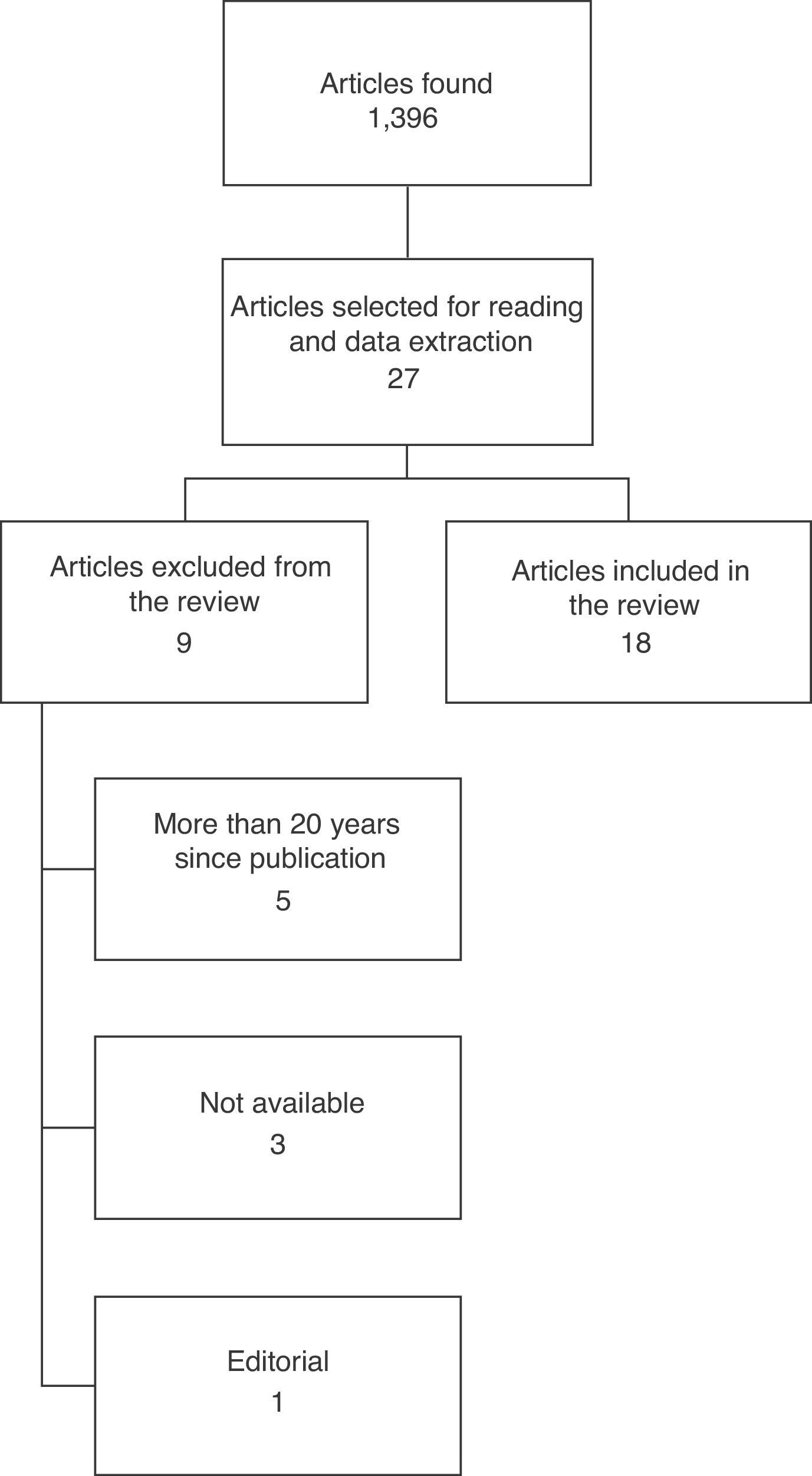
ResultsA total of 1396 studies were identified and so distributed in the databases used. Of this total, 1369 were excluded based on inconsistencies regarding the theme of breastfeeding promotion by health professionals. None of the studies located in the CINAHL and Web of Science databases were used, as they did not mention breastfeeding support by health professionals. Therefore, in this integrative review, 27 studies were potentially relevant to be analyzed, based on the reading and analysis of titles and abstracts, but nine did not meet the inclusion criteria, and were also excluded. Finally, this study included 18 articles (Fig. 1).
Regarding the type of design of the assessed studies, the sample showed a predominance of descriptive qualitative and review articles. As for the language, it seems the English language was the most frequent (60.0%), followed by Portuguese (40%). The articles found were published in the years 1997–2013 and are shown in Table 1. The results of the review are reported below.
According to Dykes,12 while health professionals positively influence breastfeeding women, they can also be a source of negative support by providing inconsistent information and inadequate recommendations to the patients. Conflicting information and, in fact, inaccurate advice are repeatedly reported by patients regarding hospital practices. Moran et al.3 reinforce that health professionals have often been identified as being inadequate to support breastfeeding, for relaying contradictory and even misleading information.
An analysis carried out by Yaman and Akçam,14 on the influence of the level of knowledge and the attitudes promoting breastfeeding within the family context of the professionals, showed that the level of theoretical instruction of these professionals did not translate in favor of breastfeeding within their own families’ scenario.
According to Barclay et al.15 and Brow et al.,16 it is important to considered that although health professionals play an important role in the initial stimulus to breastfeeding, they are not the only influence; family and friends may have a more significant influence. On the other hand, Caminha et al.17 report that it is important for the health professional to consider the mother's “cultural baggage” as an influence on the decision to breastfeed. However, the professionals must be willing to share their knowledge with the family and form a social network to provide support and encouragement for nursing mothers to overcome obstacles.
The members of the nursing mothers’ social network, including the health professionals, are capable of interfering in the decision to breastfeed, by encouraging and supporting the initiative, by transferring knowledge and cultural values, or family traditions combined with growing disinterest and discouragement, due to the pressure on the nursing mother in relation to how to feed the child.18 Considering that, Marques et al.18 infer about the need to implement new health practices regarding how to care for this population group.
A relevant aspect is the way health professionals deal with women and their families, because their doubts and questions are not always spontaneously exposed. Institutions such as the WHO and the UN Children's Fund (UNICEF) recommend that, for this approach to be carried out in an effective manner, it is necessary to use counseling skills, such as listening, understanding and offering help to mothers who are breastfeeding, supporting them to deal with pressures, thus increasing their confidence and self-esteem and preparing them for making decisions.4
Brow et al.16 conclude that mothers are under many different influences regarding the decision to breastfeed, such as lack of knowledge and motivation, easy-to-use formulas, among others, and although the professionals are willing to support the mothers, they face a lack of time and resources to do so. The need to provide consistent support is evident, by increasing the number of professionals involved, optimizing time and providing material resources to facilitate handling. Only then professionals can be trained and thus offer support to breastfeeding.
A study by Marinho and Leal,19 aiming to investigate the health professionals’ attitudes toward breastfeeding, found statistical differences due to the profession, the workplace and nursing specialty. Nurses showed more positive attitudes than physicians and professors. Watkins and Dodgson20 observed that the knowledge attributed to nursing professionals through training has positive implications for the practice, being an important factor when supporting a mother regarding the decision to breastfeed. However, women frequently report receiving little information about the act of breastfeeding by health professionals, including their own physicians.
Caldeira et al.21 reported in their study, based on the analysis of professionals’ performance in specific knowledge tests about breastfeeding through a questionnaire given to 41 college or university-level professionals and 152 technical-level ones, that, in most cases, health professionals have theoretical knowledge on the benefits of breastfeeding. When analyzing data from the questionnaires, we observed a mean of more than 80% for all professional categories considered satisfactory. However, the performance below 50% for physicians about the technique of breastfeeding and management of major lactation problems shows that such professionals still have little scientific support to address more complex issues and fail to offer adequate support to mothers with greater difficulties in nursing.
Using a semi-structured interview with five nursing aids, six resident doctors and two nurses from an Obstetric Center on the knowledge of the “Ten Steps to Successful Breastfeeding - the Baby-Friendly Hospital Initiative”, Silvestre et al.22 found that nearly 50% of the professionals were unable to report at least one step. Considering that this subject should be familiar to hospital professionals, it can be said that the lack of knowledge is considerable. Therefore, in some cases, despite the good intentions transmitted by health professionals, mothers feel they did not receive enough support, or assign blame to a professional, instead of themselves.
Breastfeeding practices, far from being an individual process involving only the mother–child pair, are the result of hospital dynamics, which also includes the attitudes of health professionals. There are obstacles to the “Ten steps to successful breastfeeding” that are resolvable, despite the unfavorable conditions that public hospitals currently offer to their users.23
In a study carried out by Manzini et al.24 in the delivery room of a hospital, it was demonstrated that most involved professionals knew about the “ten steps” and considered breastfeeding in the delivery room an important factor, considering the benefits brought to the mother–child pair, especially the formation of bonding and attachment between them. However, among the difficulties experienced by the professionals, are cesarean deliveries and the lack of training in breastfeeding. Respondents emphasized the need for greater integration among the team and that the guidelines should be relayed during prenatal care. This activity should be a continuing one, and professionals should be encouraged to support this cause, thus becoming “child-friendly professionals”.24
Meier et al.25 emphasize that breastfeeding is still not prioritized, when compared to other nutritional therapies in Neonatal Intensive Care Units (NICU). Members of the NICU staff and patients have inconsistent information, coupled with the lack of information on lactation management to optimize the dose and feeding intervals. Evidence for the use of human milk in the NICU is compelling, but the translation of evidence into best practices, tools, policies, procedures and discussion points is still limited.25
Caminha et al.17 verified that, in the presence of the maternal difficulties faced at the beginning of breastfeeding, health professionals, in addition to theoretical knowledge and clinical expertise in breastfeeding, need communication skills. To acquire these skills, it is important to differentiate between the simple act of advising and counseling. If advising is to say what should be done, counseling is a type of action where the professional listens and understands, and thus, offers help for mothers to plan and make decisions and become stronger to handle pressure, increasing their self-esteem and self-confidence.
Araújo and Almeida26 analyzed breastfeeding as a major challenge for health professionals, as they face a situation for which they were not prepared, which requires sensibility and skills to be performed. It is important to carry out periodic training of health professionals to provide breastfeeding assistance, using an approach that goes beyond the biological factors, understanding the nursing mother in all her dimensions of “being a woman”. It is evident that health professionals base their actions to stimulate breastfeeding on understanding this phenomenon as a natural act, a result of maternal instinct, while recognizing that this process is determined by social objects of the family context.26
Hoddinott et al.,27 in their study, conclude that it is essential to include the topic “Breastfeeding” at the technical and College/University level education as an specific and multidisciplinary issue, establishing national standards for education, with designated funding and participation of experts. It has been hypothesized that, by involving a multidisciplinary team in the implementation of a more effective support to breastfeeding, an intervention involving several professionals may be more effective than a specialist's approach. Relationships between health professionals can be an important factor for the success of positive interventions in breastfeeding promotion. Health professionals may feel more capable if knowledge and experiences are shared within and between teams.
DiscussionThe analyzed studies showed, in most cases, that the health professionals are not trained to promote breastfeeding. Ideally, all health professionals with whom the pregnant and postpartum women come into contact should be committed to the promotion of breastfeeding and able to provide appropriate information, in addition to demonstrating practical skills in breastfeeding management.
However, the identified studies did not show a common evaluation method, which is specific and able to analyze the practical ability of breastfeeding management by a multidisciplinary team, in addition to not proposing solutions, which hinders the discussion of the findings. Perhaps, the fact is justified by the low appraisal and new perspective of the multidisciplinary approach.
In the current scenario of breastfeeding difficulties, advice from health professionals is crucial to help mothers overcome the pre-established difficulties. This should occur at several different times: during prenatal care, in the delivery room, during rooming-in and the postpartum period. This information and guidance should also be extended to the family support network, as a mother who does not easily breastfeed loses confidence in herself and becomes susceptible to pressure from relatives and friends, in addition to imparting this distress to other nursing mothers. Still, even if a certain mother is a healthcare professional, she is also subject to the same family, social and emotional pressures, so it is necessary to intervene in the same way as with the other mothers, as professional advice is aimed at enhancing self-esteem and confidence in her ability to breastfeed.17,28
What is routinely observed in health services is the isolated work of professionals, each one carrying out his or her function in isolation and without interaction with the health team. Very often the lack of a common approach, coordination and cooperation among professionals are persistent problems that hinder women's confidence regarding breastfeeding. The lack of adequate maternal guidance, as a contributing factor to decrease breastfeeding duration, is an aggravating issue, especially for teenagers and new mothers, who want to breastfeed but are less likely to initiate or continue breastfeeding.
All health professionals, including doctors, nurses, nutritionists, physical therapists, occupational therapists, speech therapists, among others, and more specifically gynecologists and obstetricians – as they have greater contact with pregnant women during prenatal care – as well as the pediatrician, need to understand breastfeeding as a biopsychosocial, dynamic, and relational process, as well as its changes over time. People greatly look up to the physician as a source of knowledge and put their trust in their advice, so breastfeeding is a process that should be highly appreciated and included in the consultations.
Mothers seek professional help to solve their problems related to breastfeeding, but the professional usually has many rules and regulations that do not address their reality, and these factors ultimately bring fear and insecurity to the nursing mother. Considering the mother's routine, it is necessary to go beyond what is theorized and contemplate the reality she lives in, as well as to help her reflect on the best course of action in an attempt to improve her worries and promote healthy breastfeeding for her child.
All health professionals, without exception, should have modules included in their training courses that demonstrate the importance of considering interdisciplinary parameters of collaboration regarding breastfeeding. Educational institutions need to contribute to this process.
When health professionals are confident in their own capacities to support breastfeeding women, they become more likely to positively promote breastfeeding and offer support to mothers. Breastfeeding support opens up a multiprofessional universe, in which the performance of these different actors constitutes the object of research.
Final considerationsLiterature does not clearly depict the importance of health professionals regarding the promotion of breastfeeding, and there are few studies demonstrating the role of health professionals that can constitute a breastfeeding support team, including elements of education, problem-solving and adequate support. The lack of health professionals trained to deal with the breastfeeding factor was evident in the analyzed studies, and especially the physician, who should be the protagonist in health protection through breastfeeding.
It can be concluded that health professionals need to be better trained to work with breastfeeding. It is suggested a greater incentive on the part of managers (at municipal, state and federal levels) to create multidisciplinary teams committed to maternal and child health and improvement regarding the approach of theoretical and practical contents in technical, as well as college/university institutions.
Encouragement to the practice of breastfeeding should occur through improvements and changes of all professional teams. Changes must occur, mainly in hospital routines, by implementing the “Ten steps to successful breastfeeding”. These steps guide and reinforce effective breastfeeding support, in addition to being one of the requirements for the implementation of the Baby-Friendly Hospital.
FundingThis study did not receive funding.
Conflicts of interestThe authors declare no conflicts of interest.