The present case report describes placement of tooth implants in a patient with history of smoking, exhibiting severe, chronic periodontitis and maxillary atrophy with horizontal bone volume deficiency. Simultaneously to implant placement, the technique of divided crest, ridge expansion and bovine bone graft placement was used. After six months, bone integration of all implants was observed and a hybrid, implant-supported prosthesis was manufactured (full bone anchorage). Finally the case was followed for 18 months without observing any complications, and with satisfactory functional and esthetic results for the patient.
Este reporte de caso describe la colocación de implantes dentales en un paciente con antecedente del hábito de fumar y que presenta periodontitis crónica severa y atrofia maxilar con deficiencia de volumen óseo en sentido horizontal. Simultáneamente a la colocación de implantes se utilizó la técnica de cresta dividida, expansión del reborde y colocación de injerto óseo bovino. Después de seis meses, se observó la oseointegración de todos los implantes y se procedió a la confección de la prótesis implantosoportada de tipo híbrida (anclaje óseo completo). Finalmente, se realizó el seguimiento del caso durante un periodo de 18 meses sin observar complicaciones y con un resultado funcional y estético satisfactorio para el paciente.
One of the main criteria to select a patient for candidacy to tooth implant placement is availability of bone volume.1,2 Literature reports that minimum bone dimension required to place an implant should be 5mm wide (bucca-palatal/lingual) and between 7 and 10mm high.3,4 Nevertheless, in practice, there is a great number of patients requiring dental implants who lack ideal bone circumstances. Among these circumstances, the most frequent is insufficient bone volume, which can be due to the following: alveolar ridge atrophy due to tooth absence, periodontal disease or as sequel of some trauma or condition. These insufficient bone situations are called alveolar ridge deformities; they have been classified according to their morphology.5 According to this classification, class I consists on bone loss in buccal-lingual direction, this provides more predictable results when applying techniques of horizontal bone volume increase.6,7 Among these techniques, the following are described: autogenous bone graft trechniques,8 block bone allografts,9 and bone ridge expansion techniques.10 Nevertheless, autogenous block bone graft, up to this date, is the technique most frequently used and is considered the gold standard due to the fact it has shown satisfactory long term results.11 On the other hand, disadvantages of this technique must also be considered: there can be greater morbidity due to donor zone and waiting time required before implant placement.12 On the contrary, this article purports to present the technique called divided crest with bone expansion and placement of organic bovine bone graft as an alternative to the rehabilitation in a case of maxillary atrophy, performed at the Dental Clinic of the Universidad de Los Hemisferios, Quito, Ecuador.
CASE REPORTPatientA 55 year old male patient in apparent good health attended the Dental Clinic of the University Los Hemisferios, Quito Ecuador requesting manufacture of a prosthesis for his upper jaw; the patient additionally informed of tooth mobility and discomfort when speaking or chewing. As relevant history, the patient informed he suffered controlled blood hypertension and habit of smoking over ten cigarettes a day.
Clinical examinationIntraoral examination revealed absence of most teeth in the upper jaw, tooth extrusion, presence of abundant dental plaque and calculi, presence of periodontal pockets larger than 7mm, dental caries, multiple gingival recessions and evident atrophy of upper alveolar ridge affecting patient's facial aesthetics.
Radiographic examinationRadiographic examination revealed generalized horizontal bone resorption, pneumatization of both maxillary sinuses, caries in tooth 1.3, radio-lucid lesions at the height of periapex of teeth 1.3, 1.4, 2.6 and 4.4 (Figure 1).
DiagnosisBased on information harvested from clinical and radiographic examinations, the following diagnoses were established: severe generalized chronic periodontitis in tooth 1.3, dental abscesses in teeth 1.3, 1.4, 2.6 and 4.4 as well as upper and lower partial edentulism with upper alveolar ridge atrophy and bilateral maxillary sinuses pneumatization.
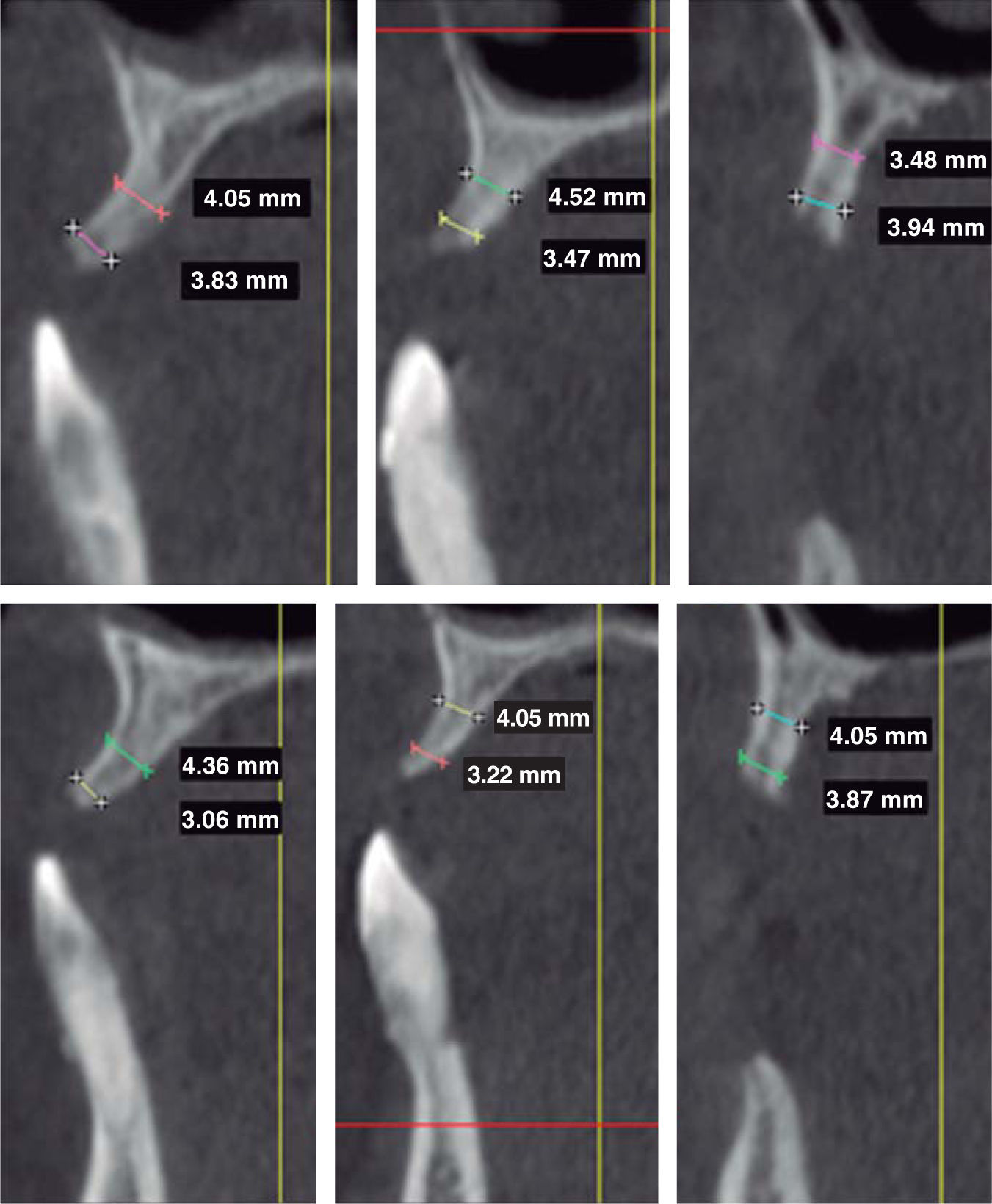
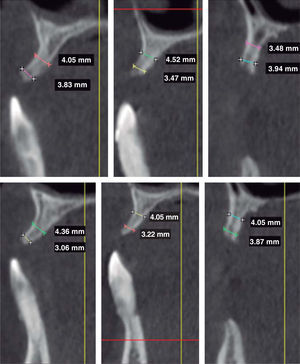
Tomographic evaluationA cone beam computerized tomography was indicated in order to assess remaining bone availability which could allow implant placement. Tomographic evaluation revealed that, in the upper jaw, in spite of generalized bone resorption, there was sufficient bone mass to place a crown-apical implant. Contrarily, in buccal/palatal direction, no sufficient bone mass was found for conventional implant placement (Figure 2). Therefore, this jaw would correspond to Seibert's class III alveolar ridge deformities, thus, the need arose to perform additional surgical procedures to allow placement of at least six implants.
The lower jaw exhibited a bone defect compromising vestibular and lingual aspects of remaining bone at the level of tooth 4.2. Nevertheless, sufficient bone mass was found to place four implants in the inter-foramen area.
TreatmentConsidering that the patient was a heavy smoker and the poor periodontal circumstances exhibited by his teeth, the following procedures were undertaken: patient was instructed to quit smoking and to continue with treatment, oral hygiene instruction was provided, roots were scaled and planed, all upper and lower teeth were extracted and provisional prostheses were manufactured. After this, placement of six implants for the upper jaw and four implants for the lower jaw was planned in order to manufacture implant supported prostheses (full bone anchorage) at a later point in treatment.
Surgical procedureUpper JawHalf an hour before commencing surgical procedure, patient was medicated with amoxicillin, 1g, orally, dexamethasone 4mg and ketorolac 60mg intramuscularly. Intraoral asepsis was achieved with 0.12% chlorhexidine, extraoral asepsis was conducted with iodopovidone. Surgery was performed with local anesthesia (lidocaine 2% with epinephrine 1:100,000).
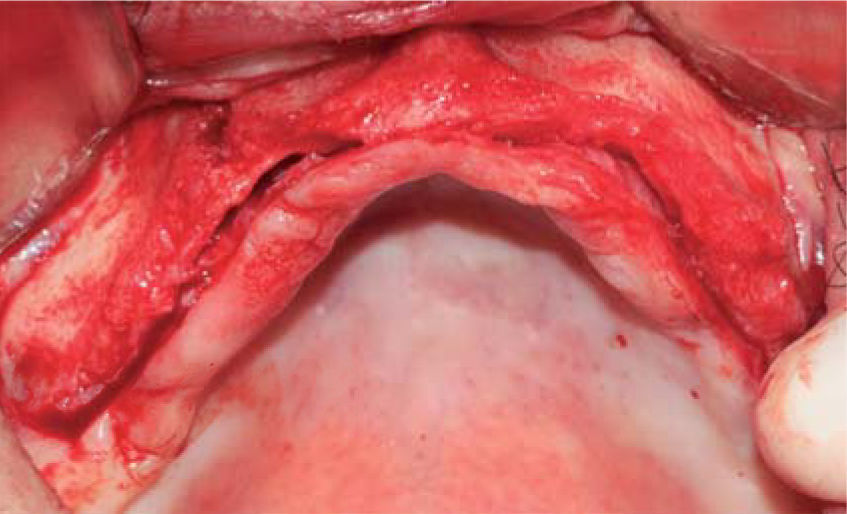
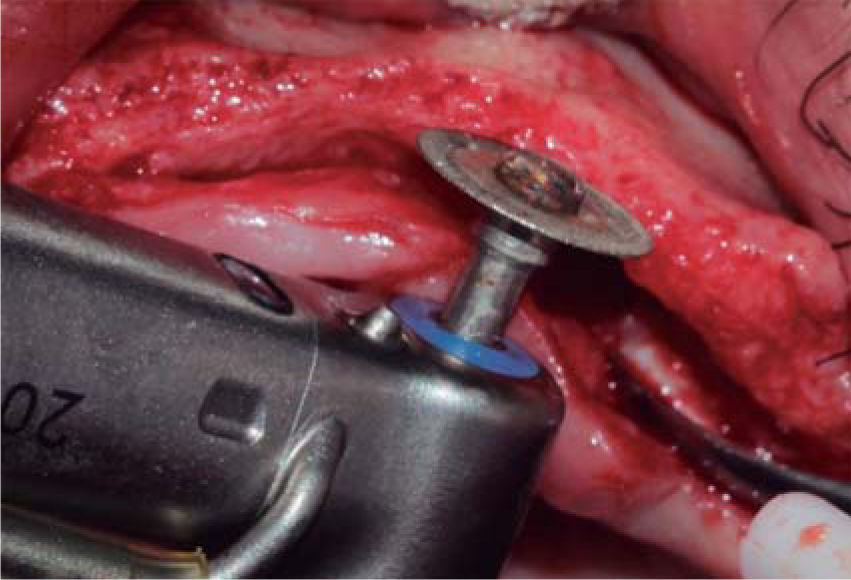
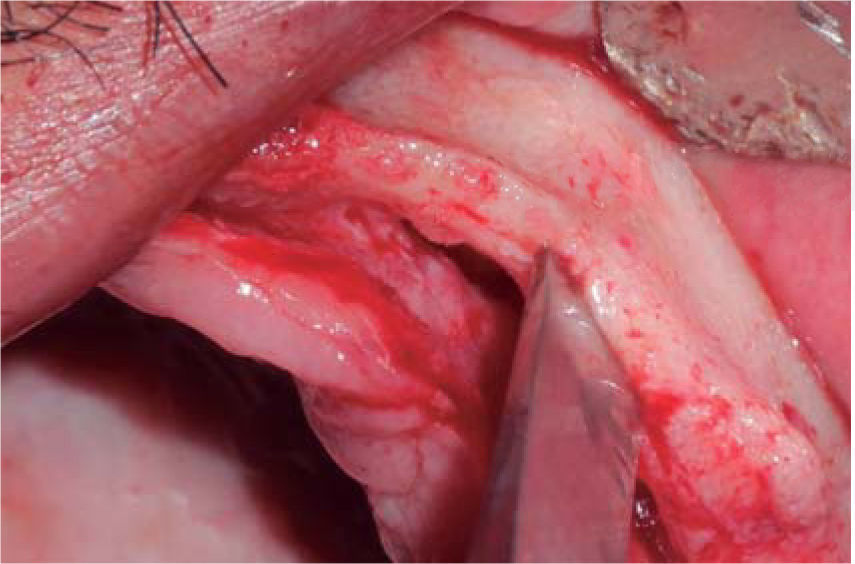
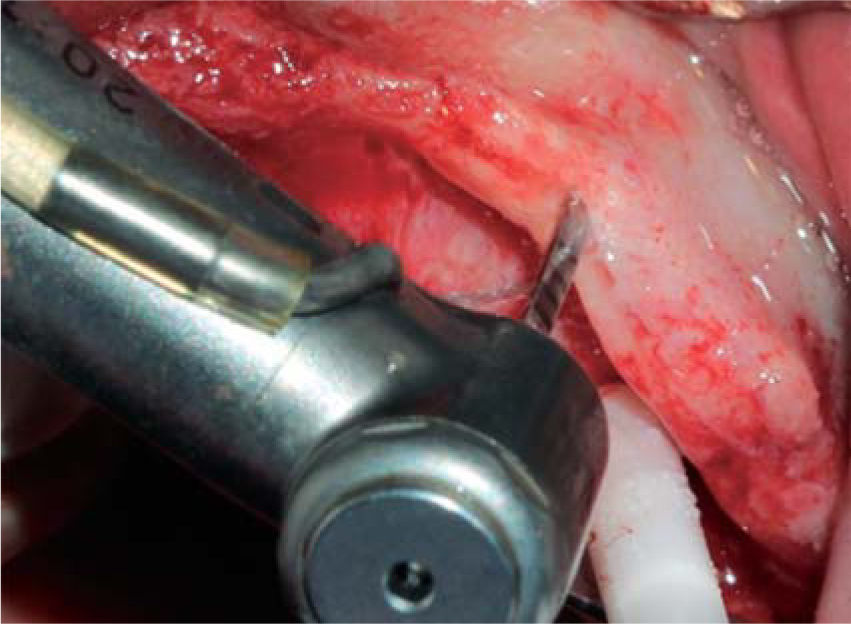
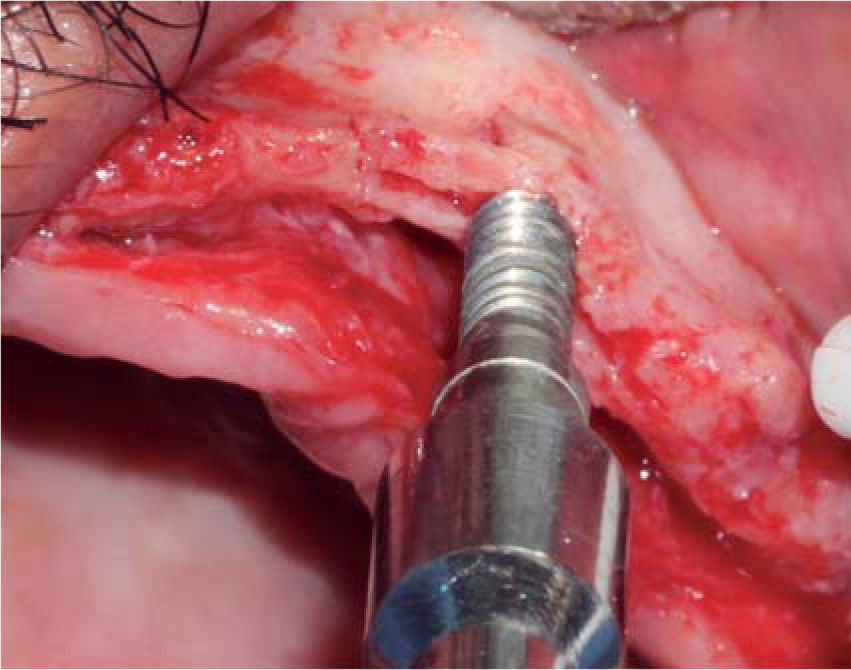
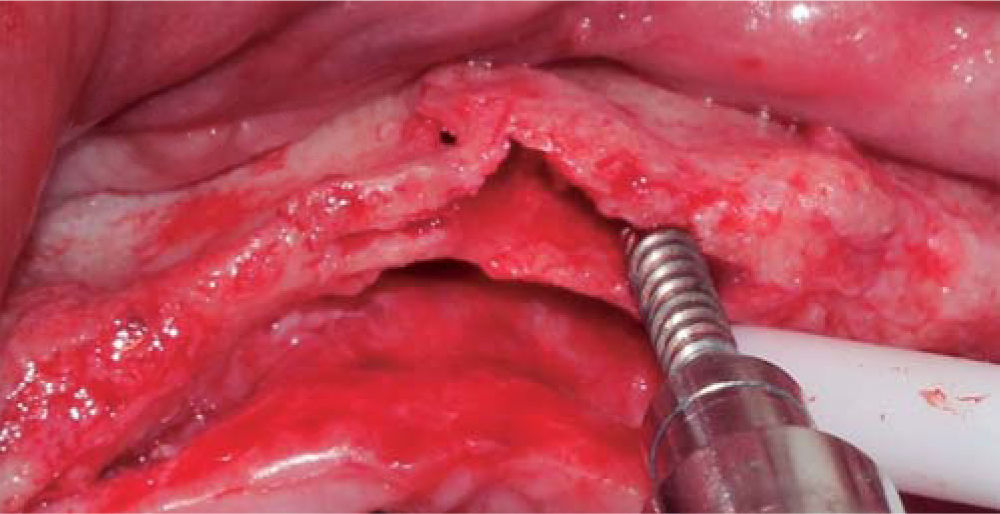
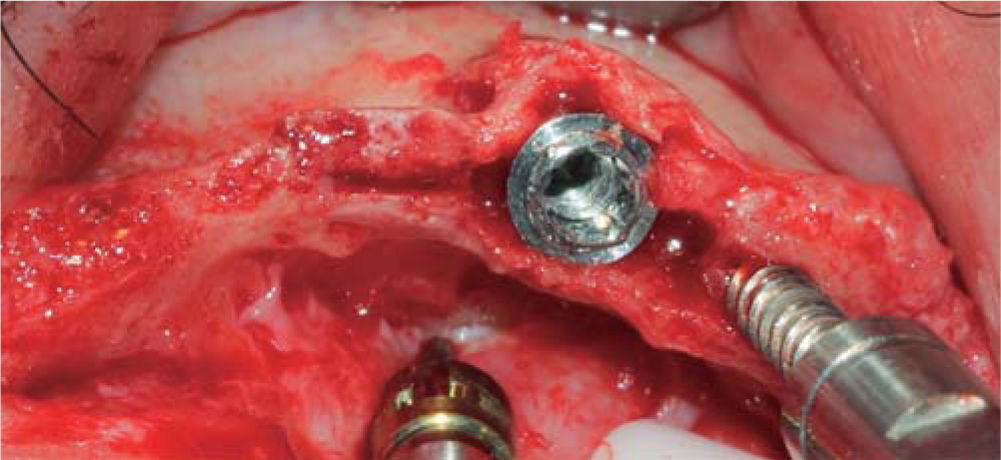
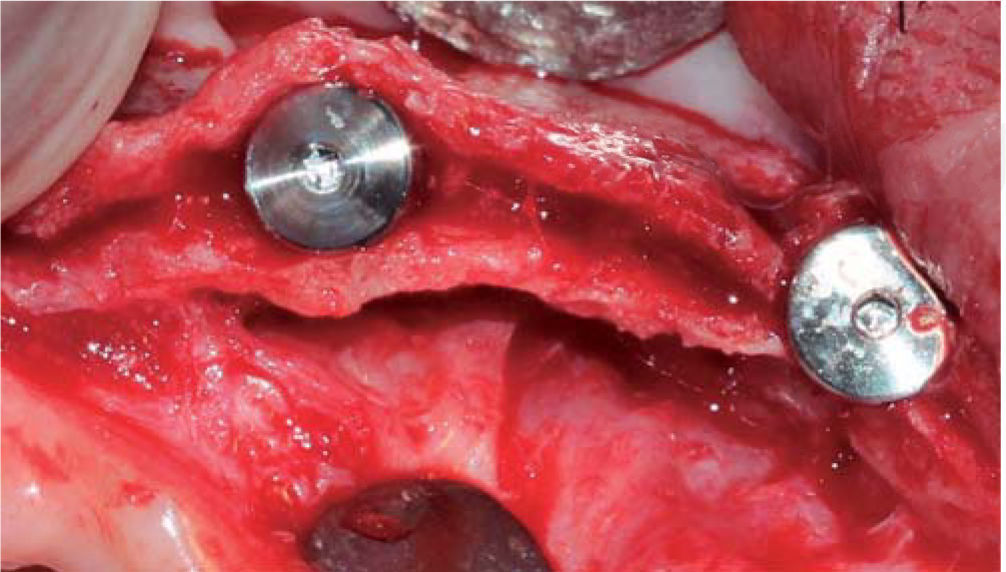
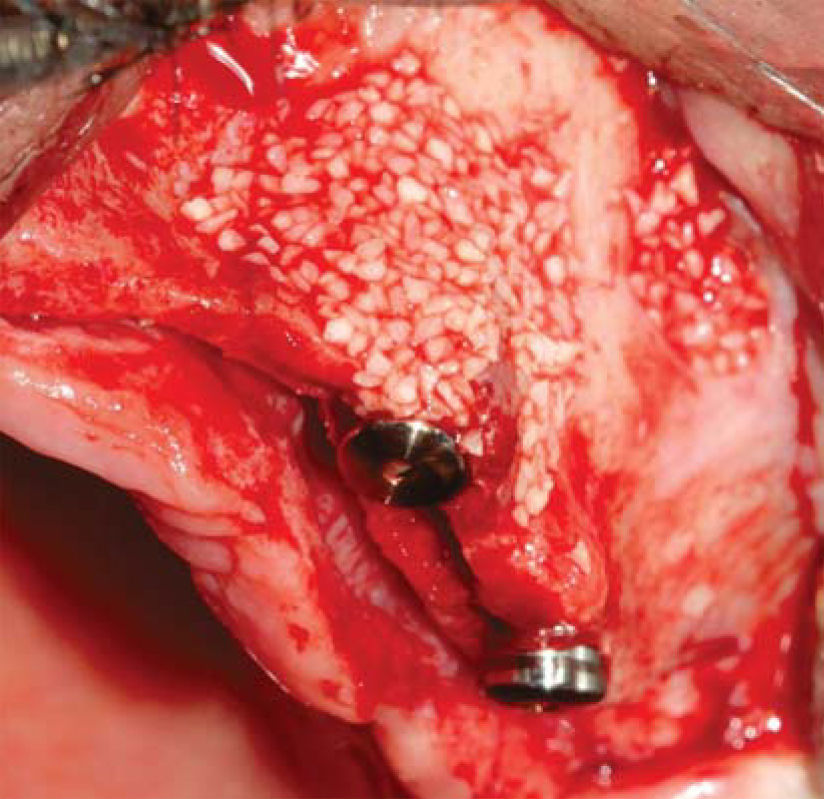
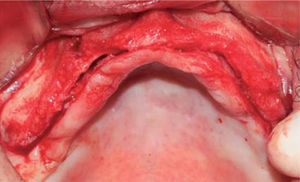
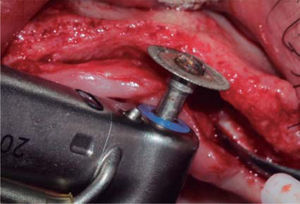
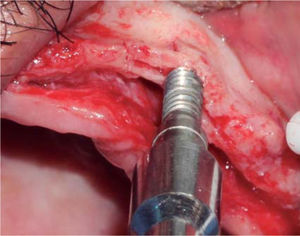
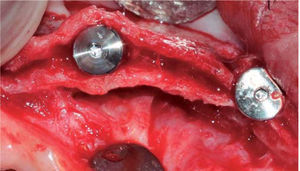
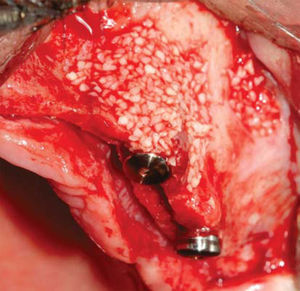
A full thickness incision over the crest was performed, raising a mucoperiosteal flap exposing bone table up to 4mm from the top of the crest in vestibular direction; from that point the flap was divided into partial thickness (Figure 3). After this, impact points were marked in designated places according to surgical guide for implant placement; perforations were initiated with a 1.6mm diameter burr in order to determine desired implant depth and axis. After this, a ridge was created on the crest with a diamond burr, fracturing cortical bone to create chisel's access to cancellous bone, and with the aforementioned, bone tables were separated until reaching a 5mm depth (Figures 4 y 5). Perforations were further continued with a 2.0 diameter burr (Figure 6), and vestibular table expansion was undertaken creating greenstick fracture with the expanders, until reaching sufficient osseous bed diameter (3.2mm diameter) (Figures 7 y 8). Implants were then placed at a 25rpm speed and 35 Nem torque (Figures 9 y 10). After this, a particulate bovine bone graft was placed (Bonefill® Bionnovation Biomedical, Sao Paulo, Brazil) with the aim of preserving integrity of vestibular bone tables (Figure 11). All these procedures were repeated for placement of all six implants. Finally, sutures were undertaken with monofilament nylon 5/0.
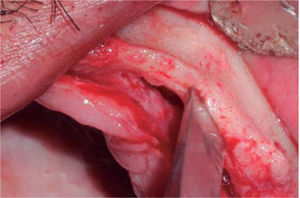
For this surgical procedure, the patient received the same pre-surgical preparation than that used for the upper jaw. Procedure was initiated with an incision between grooves at the level of all teeth, after which a mucoperiosteal flap was raised. Teeth were then extracted and adjacent granulation tissue was removed, trying to preserve all bone remnants. After this, bone ridge was regularized and remodeled using multi-laminated burrs with abundant irrigation. With a conventional burr sequence, perforations were then initiated at places designed for implant placement. After this, all four implants were placed, locating prosthetic platforms at one same level. Since there was presence of bone defects and three walls around the implants, particulate bovine bone graft was placed (Bonefill® (R) Bionnovation Biomedical, Sao Paulo, Brazil). Finally, sutures were applied with monofilament nylon 5/0.
Postsurgical medicationAmoxicillin, 500mg orally every 8hours for five days.
Ketarolac, 60mg intramuscularly every 12hours for one day.
Dexamethasone, 4mg, intramuscularly, every 12hours for one day.
Ketarolac, 10mg orally every 8 days for three days.
Mouth rinses with 0.12% chlorhexidine gluconate.
This protocol was indicated for surgical procedures of both jaws.
Post-surgical controls were conducted after 24hours, seven days and 14 days. No complications were observed and suture points were removed.
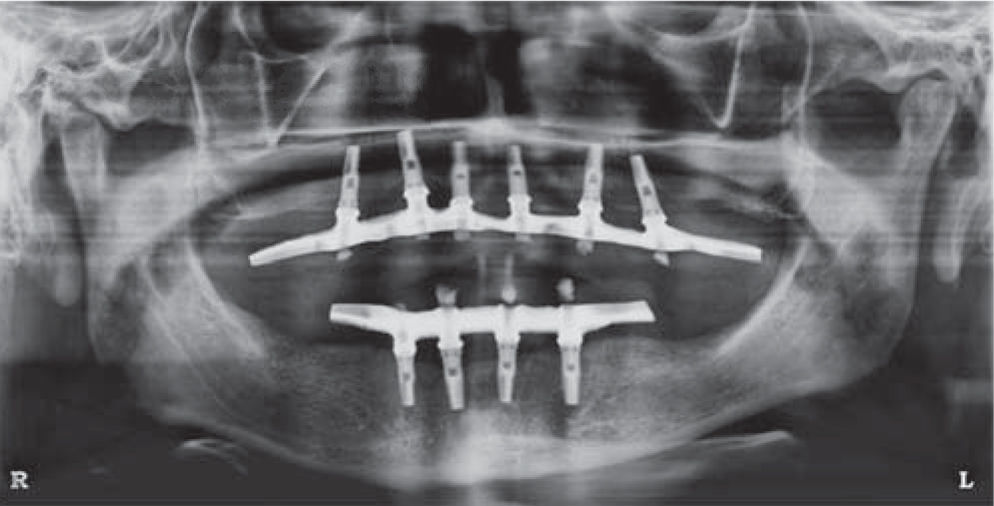
After six months, radiographic evaluation was conducted, which revealed preserved bone tissue surrounding the implants and no signs of complications. After this, surgical exposition and healing screw placement was undertaken and bone integration of all implants was observed.
Implant supported prosthesisTwo weeks later, manufacture of implant-supported prosthesis for both jaws was undertaken. Both prostheses were of hybrid design (full bone anchorage).
The case was followed for 18 months; no complications were observed and final result was functional and aesthetically satisfactory.
DISCUSSIONSplit-crest technique allows primary stabilization of tooth implants in atrophied bone ridges by means of bone expansion. This technique can be indicated as an alternative to regenerative procedures avoiding morbidity of donor sites, decreasing the number of surgical procedures and treatment time.13 Nevertheless, bone defect morphology is an important consideration for the techniques’ suitability. Requirements are: an alveolar ridge mostly composed of medullar bone, with a wide base and crest in the shape of a knife blade, with sufficient bone height (10mm at least) and width of 3 to 5mm.13,14 Thus, the technique purports the objective of creating a space through the division of the bone crest into two sections, with greenstick longitudinal fracture, allowing immediate insertion and stabilization of implants in the most apical, nonfractured portion of the bone ridge.14
This intact bone region in the apical portion must be able to allow for a 3 to 4mm deep preparation as a minimum, in order to obtain primary stability during implant insertion.13,14
Another important aspect during bone preparation is the use of surgical guides as protocol to avoid unfavorable implant inclination. Some studies describe an excessive inclination of implants in the direction of the vestibular table which was moved during the expansion procedure thus functionally and aesthetically compromising final treatment result.10,15,16
Moreover, it has been said that it is frequently necessary to fixate with wire the fractured table onto the palatal table; this would render the procedure more complex, and in some cases, the ligature could be prematurely exposed; this would require an additional procedure to remove it before the implants complete the period of oseointegration.17
The Split Crest technique provided horizontal ridge increase of about 1-4mm; the upper jaw exhibited the greatest increase (4-3mm) when compared to the lower jaw (1-1.5mm).14 Likewise, greater numbers of complications have been reported when this technique has been used in the lower jaw.18 Therefore, indications for this procedure are more frequent and bear better prognosis when used in the upper jaw. It is worth mentioning there is controversy with respect to use of biomaterials during performance of Split Crest procedures. Use of membranes,14,19 bone grafts17 and materials such as tricalcium phosphate β (β-TCP) associated to platelet rich plasma13 have been described.
It has been reported that use of membranes as a barrier along with bone expansion entails greater difficulty for flap primary healing, increasing possibility of membrane exposition and infection during postoperative periods.20 Other reports compare intercortical bone space obtained after expansion with an extraction site that does not require filling with graft, they highlight the importance of periosteum and matrix in the regenerative process.21 Nevertheless, the present article describes use of bone graft composed of bovine inorganic matrix to fill osseous beds resulting from table division. Thus, the bone graft is surrounded by bone walls and also covered by periosteum, allowing ingress of osteoblasts and pre-osteoblasts into the graft.17,22 Bone reparation followed by this procedure is similar to that of a fracture, non-elevated vestibular mucoperiosteum is responsible for vascular nutrition and fixation of mobilized bone segment. After a five month period, a trabeculated area was observed with mature bone characteristics and remodeling capacity as well as the ability to withstand functional loads through the implants.23 For this reason reports advise to wait for a six month healing period before loading the implants.13,14,17
Likewise, in the case described in the present article, it was decided to wait for six months before subjecting the implants to functional loads. Moreover, all implants were bone-integrated and were loaded without any complication at an 18 month followup period. This result concurs with the survival and success rates of implants placed with the split crest technique reported by other authors.13,14,18,19
Due to all the aforementioned facts, it is recommended to carefully select those cases where this technique can be used, taking into consideration ridge morphology and bone density. It is also suggested to carefully handle all tissues in order to preserve periosteum integrity and use filling material to reduce risk of vestibular bone table loss.
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam