Treatment of gunshot wounds in the maxillofacial region is a complex subject, especially controversial with respect to treatment time. Current literature supports immediate treatment rather than late care, claiming to achieve better results. Wounds are heterogeneous, with characteristics that must be analyzed so as to define treatment according to Kanzanjian and Converse's principles, but always adapting to specific needs. Handling is dependent upon type of weapon, bullet's disfiguring characteristics, kinetic energy, place of impact as well as patient’ s general health circumstances. The aim of the present research was to conduct a bibliographic review and expose our experience in maxillofacial gunshot wound treatment. We hereby document treatment of three facial gunshot wound patients who sought treatment at the Regional Hospital General Ignacio Zaragoza, Mexico City, Mexico.
El tratamiento de las heridas por arma de fuego en la región maxilofacial es un tema complejo, controversial especialmente en relación al tiempo de tratamiento. La literatura actual respalda el tratamiento inmediato sobre el tardío, presentando mejores resultados. Las heridas son heterogéneas con particularidades que deben analizarse y definir su tratamiento con base en los principios de Kazanjian y Converse, pero adaptándose a las necesidades específicas. Su manejo va en relación al tipo de arma, características deformantes de la bala, energía cinética, lugar de impacto y estado sistémico del paciente. El objetivo del trabajo es realizar una revisión bibliográfica y exponer nuestra experiencia en el manejo de heridas por arma de fuego a nivel maxilofacial. Se presenta el tratamiento de tres casos de heridas faciales por arma de fuego atendidas en el Hospital Regional General Ignacio Zaragoza.
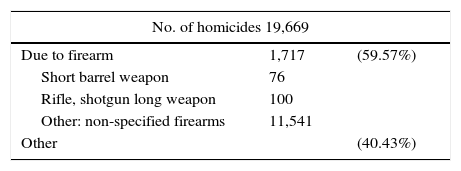
Records of the INEGI (National institute of Statistics and Geography) concerning culpable homicide in Mexican Territory in 2014 reveal 19,669 cases, out of which 11.717 (56%) were caused by firearms; this results in approximately one firearm murder committed every two hours (Table I).1 This would place gunshot wounds as a public health problem. This type of wounds represent a challenge in maxillofacial treatment due to their heterogeneity, complexity, multiple procedures in the same patient as well as high complication rate. These tissue injuries are caused during war conflicts, civil problems such as aggression, accidents and suicide attempts; each of them exhibiting particular characteristics.2
GENERAL ASPECTS OF BALLISTICSDamage degree is related to the energy caused by mass and impact speed of the projectile. This is represented by a formula, and is known as kinetic energy (KE), where speed is more important than mass.3
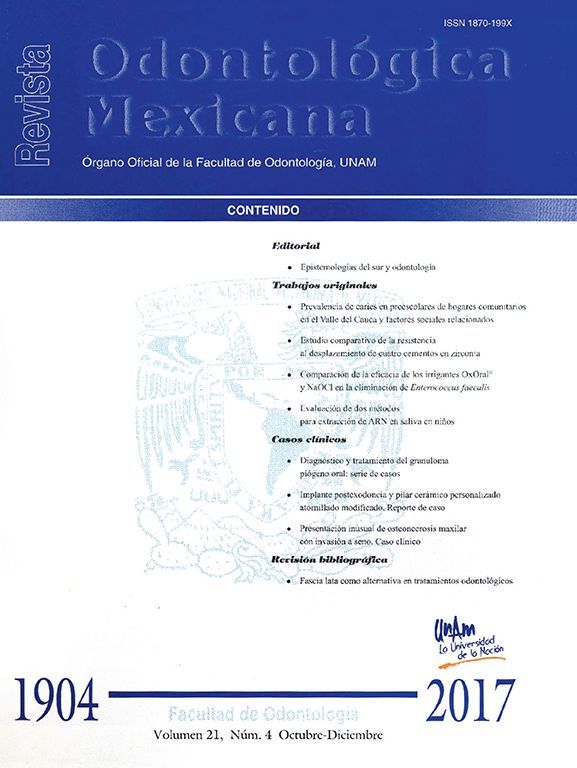
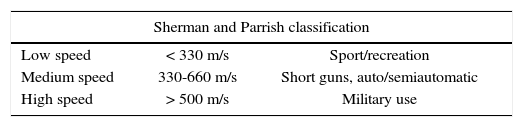
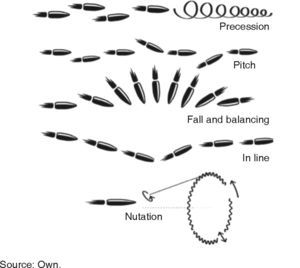
In these cases, the aim is to provide basic vital support, stabilize the patient and restore continuity, function and facial esthetics. For study purposes they are called ballistic wounds and are classified within penetrating trauma. Physics catalogues a projectile's movements into three parts: interior (within the barrel), exterior (from exit to impact), terminal (penetration into solid objects). The following displacement patterns can be observed: Precession, fall and balancing, pitching, in line and nutation (Figure 1).3,4 There is no universal agreement to classify them according to speed (velocity): US literature defines high speed to be found in the range 610-914 m/s, United Kingdom considers high speed anything over 335 m/s, Sherman and Parrish classify them in lesser than 330m/s (minor), between 330-600 m/s (medium) and in excess of 600 m/s (major) (Table II).2,5
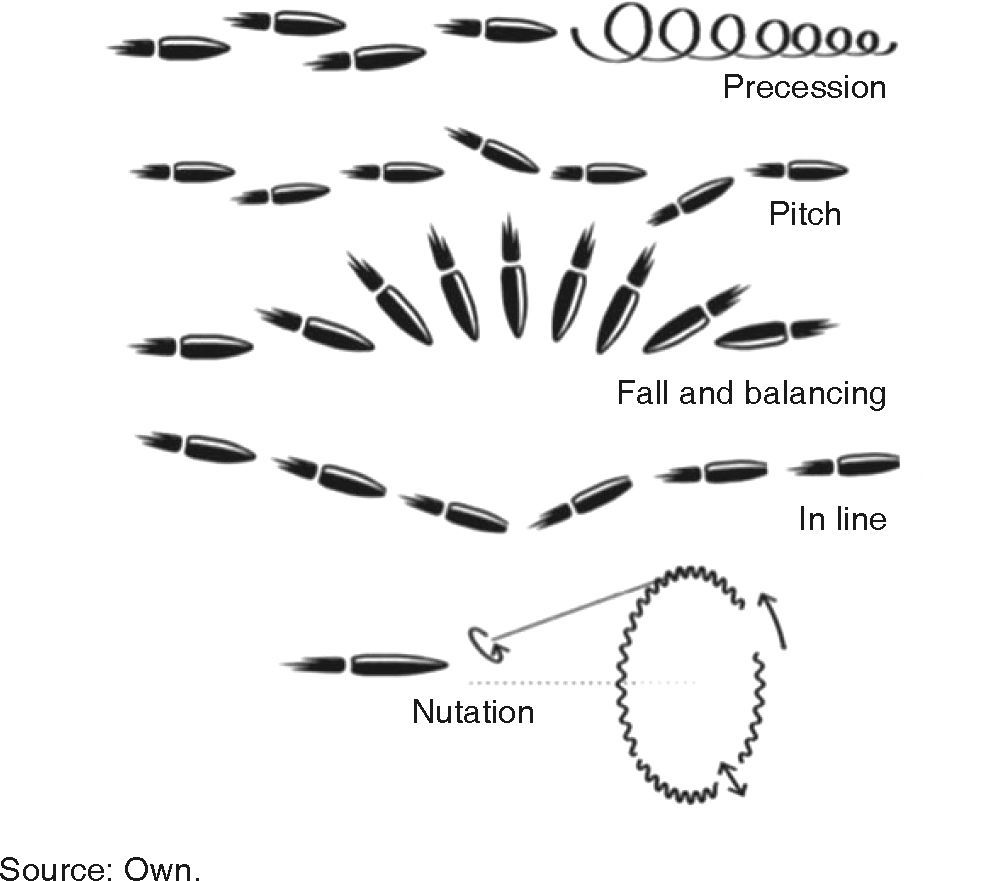
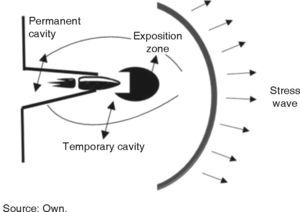
When compared to low speed projectiles, a high speed projectile generates greater kinetic energy, nevertheless, it is wrong to assume they cause greater damage. Injury level depends on many factors: kinetic energy, deformation capability, bullet fragmentation and resistance to deformation exhibited by involved tissue.5,6 In our assessment, not only speed was deemed relevant, impact zone, kinetic energy, bullet characteristics and penetration trajectory were equally deemed relevant in order to define damage as well as to provide prognosis and treatment plan. The moment a projectile enters the body, it creates a permanent cavity measuring a diameter similar to the projectile's; laterally it creates a temporary cavity caused by the expansion of the kinetic energy and forwardly it creates a stress wave (Figure 2).2,4 It must be considered that minimum speed to perforate skin is 50 m/s and to affect bone it is 60 m/s.2 Kinetic energy thus transferred to the body causes changes in tissue circulation, metabolism and electrolytic alterations.7 A critical factor to consider is the inability of bone to absorb energy without fracturing. Glass and bone are similar in their behavior in front of a bullet; energy distribution renders them fragile material.8 Hulke et al, consider several variables of bone damage according to kinetic energy, bullet characteristics and type of tissue: bone depression, simple fracture, comminuted fractures or full separation of bone segments. A high speed projectile can produce bone fragments which in turn will exit as projectiles in the direction of the bullet's entrance. When contacting the bone, the projectile might become deformed or fragment, causing thus greater damage to the soft tissue.3
EVALUATION, CATEGORIZATION AND STABILIZATIONAll patients having suffered any kind of trauma must be initially treated according to basic resuscitation rules, which have recently been renamed from ABC (airway breathing compression) to CAB (compression airway breathing) where priority is given to thoracic compressions in order to hemodynamically stabilize the patient.9,10 In a parallel manner, using Glasgow scale, the patient's consciousness state is determined. According to patient's circumstances, airway is secured (Step A) by means of intraoral objects (whenever available), cervical hyperextension is examined (to discard cervical damage) and/or cricothyroidotomy and tracheotomy. In a lesser than 8 value according to Glasgow scale, the following is recommended: nasotracheal or orotracheal intubation depending on whether there is respective facial fracture in the lower third or middle third.10 Demetriades et al in their study recommend, even in minor injuries, to ascertain presence of dissecting hematoma or hematoma blocking the airway. They inform that up to 35% subjects wounded by firearms require initial airway stabilization.11,12
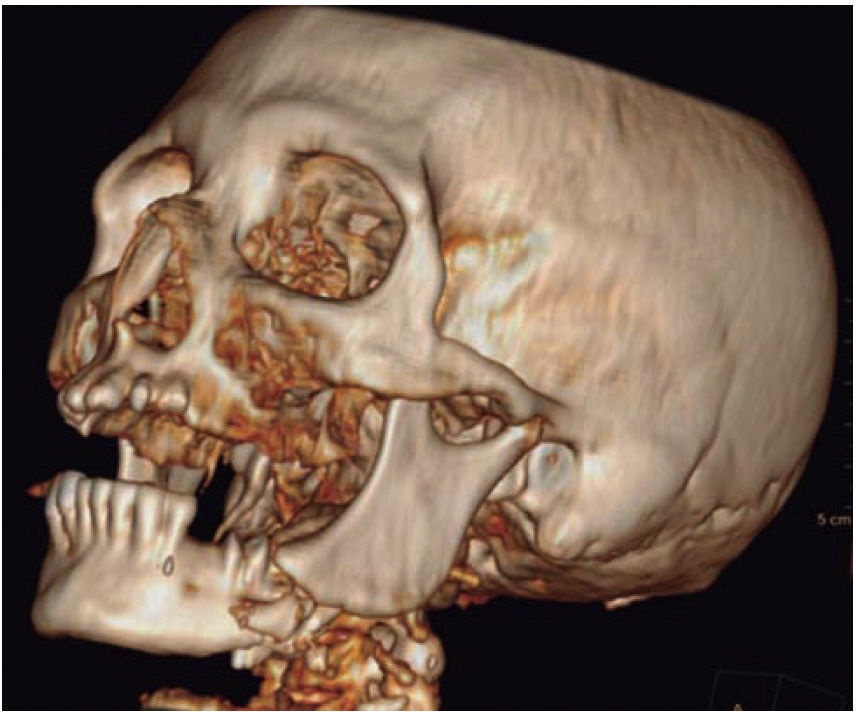
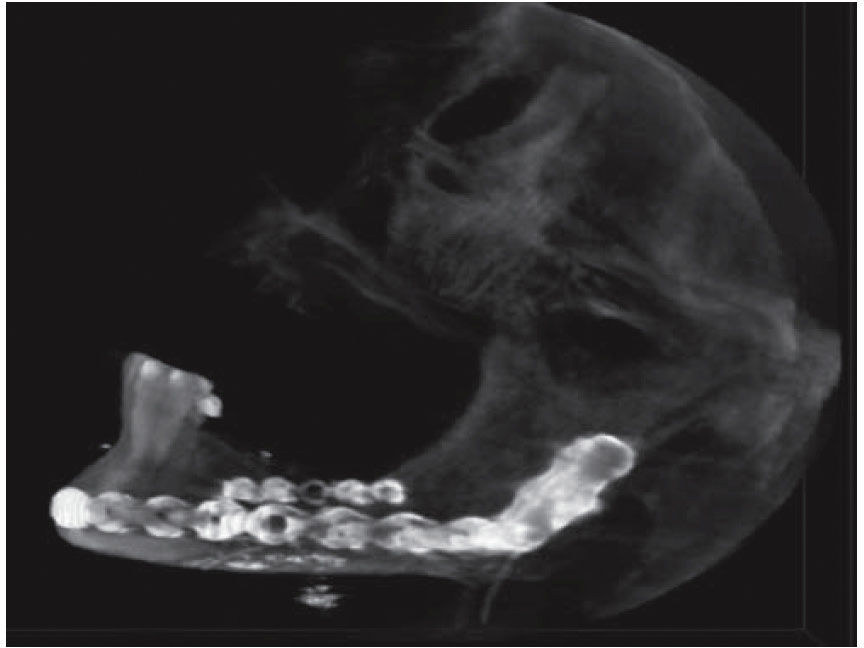
Clinical exploration and vital signs analysis provide a panorama of real bleeding and accumulated blood loss (Step B). Once the airway has been stabilized and the hemodynamic status is confirmed, proper ventilation of the patient must be secured with appropriate measures (Step C). In cases of active bleeding, first treatment is local pressure application with tamponade (plugging). If there is no improvement in hemodynamic situation, an angiography is performed, and as specific measure, an intervening image expert performs an embolism or surgical exploration and injured vessel ligation.13 Once the patient is stabilized, area specialists will assess presence of intracranial, thoracic, abdominal, orthopedic and ocular trauma.7 Pharmacological treatment initiates with, among others, administration of solutions, blood derivatives, antibiotics, analgesics, and anti-tetanic prophylaxis.14 Once urgent treatment has been provided by the aforementioned specialists, comprehensive assessment of firearm lesions in the maxillofacial region is undertaken. Manson uses four components for this evaluation: soft tissue damage, bone alteration, soft tissue loss and bone loss.15 The wound is cleansed with physiological solution; contaminant material, necrotic tissue and foreign bodies are removed. The projectile's entry and exit orifices are identified, as well as lesions caused in the course of trajectory. In cases when no exit orifice is found, it must be established in which space or tissue might the projectile be lodged.16 Bone damage assessment is initiated with palpation, and it is supported with simple image studies such as orthopantomography and Waters’ X-ray; in order to design treatment plan the aforementioned can be supplemented with a computerized tomography with 3-D reconstruction.12,17
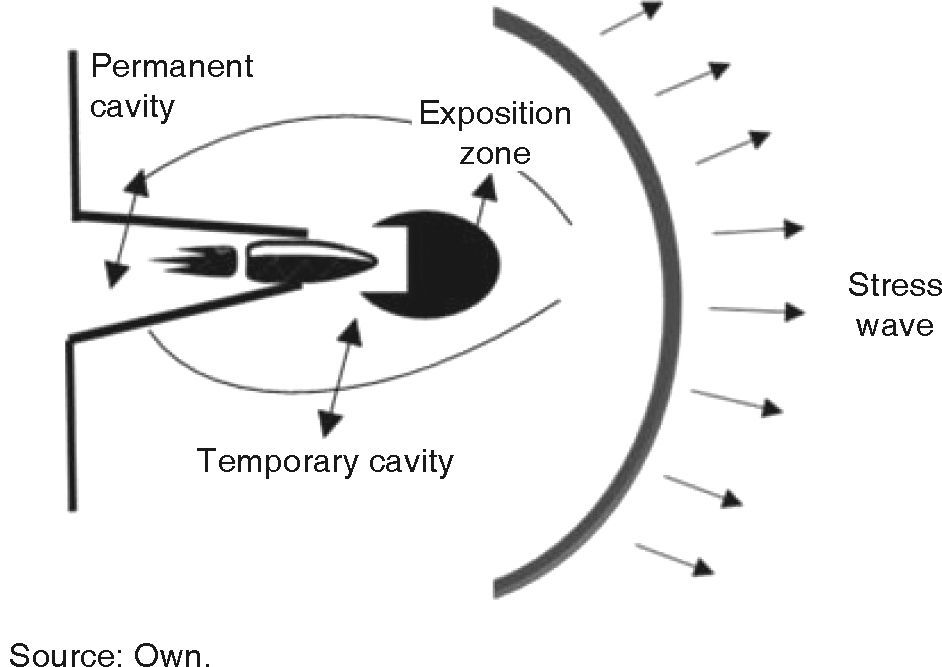
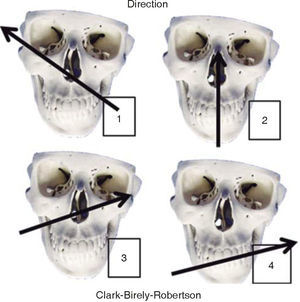
TREATMENTFirearms wounds are established and a guide is created to definitively treat these lesions. There are many classifications; nevertheless, we are based on four of them. The first classification is established in function of the projectile's entry and exit pattern, the second classification is established according to the weapon's caliber and distance of the projectile, the third classification, described by Clark-Birely Robertson, is in function of four possible trajectories of the projectile in the face (Figure 3),9 and the fourth classification, in low and high energy lesions, is established in function of mass loss and lesions inflicted in the face.16
Treatment is based on the knowledge Kazanjian and Converse acquired during WW1. They established three phases: first, debridement, removal of nonviable teeth, devitalized bone, wound cleansing and syneresis. Second: immobilization of bone fragments, third: reconstruction with filling material, grafts, final system of osteosynthesis.15 A high speed bullet does not necessarily cause high degree energy lesions, neither do low speed bullets cause low degree injury. As we previously mentioned, injury grade depends on distance and projectile's characteristics. It must be remembered that in a war situation weapons are used to incapacitate rather than to kill, since the wounded generate need for more human and physical resources than the deceased. Low degree energy lesions exhibit minimal soft tissue loss and scarce necrosis around the wound, in general terms, bone lesions are simple fractures with no bone avulsion. In this type of lesions prognosis is favorable due to the existing suitable soft tissue coverage.16,18 Wounds classified as caused by high energy weapons are those elicited by large projectiles, with deforming ammunition and firearms placed at short distance. These are wounds causing large losses of soft tissues, ischemia, tendency to necrosis and are accompanied by variable bone lesions, with bone loss and multiple or comminute fractures.16 These lesions must be treated in two or three steps: first, debridement and primary closure, second, fracture reduction, graft placement (bone, skin or myovascularized grafts), third, correction of residual deformities and implant rehabilitation. It is important to bear in mind that mandibular vascularity is provided by the periosteum, and early periosteum loss added to microcirculation alterations can cause bone sequestration, nevertheless, infection can appear in cases when bone segments remain mobile for a long time.19,20
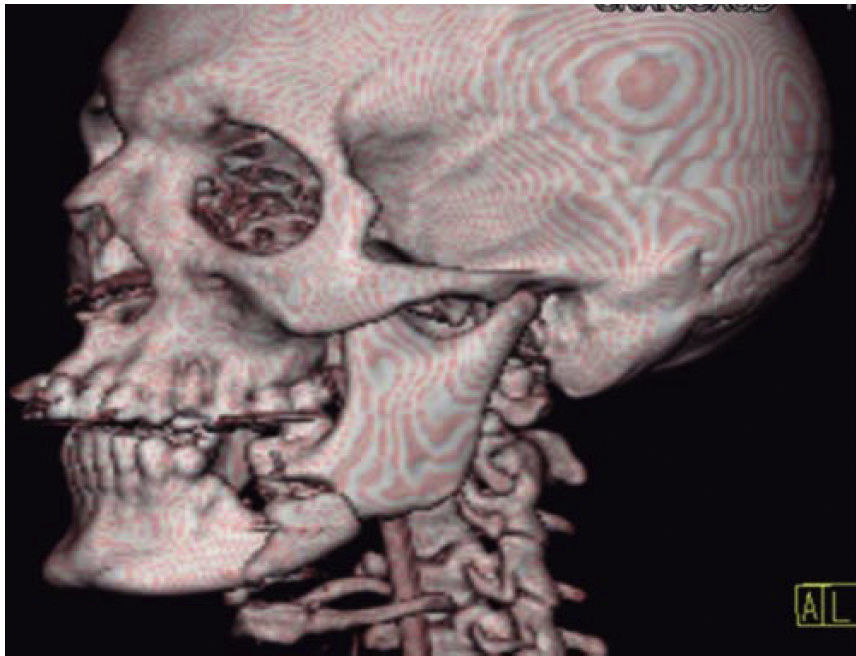
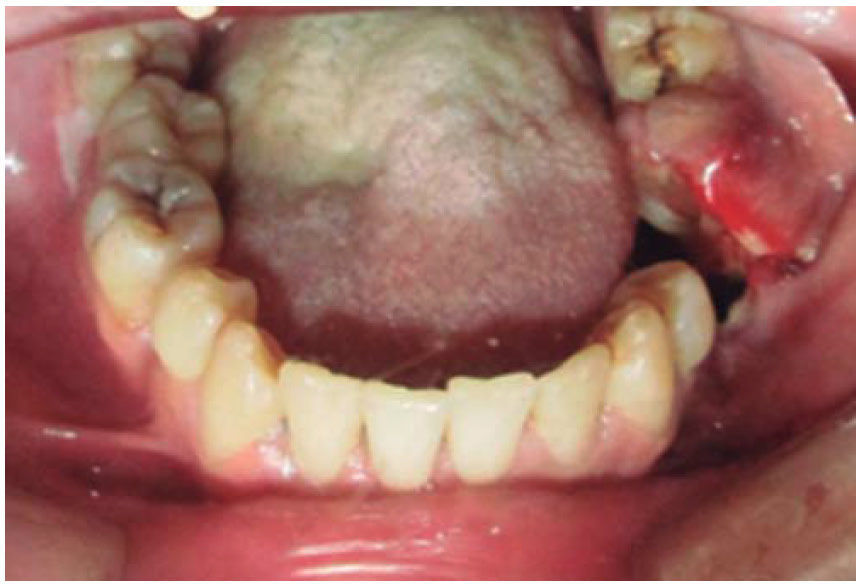
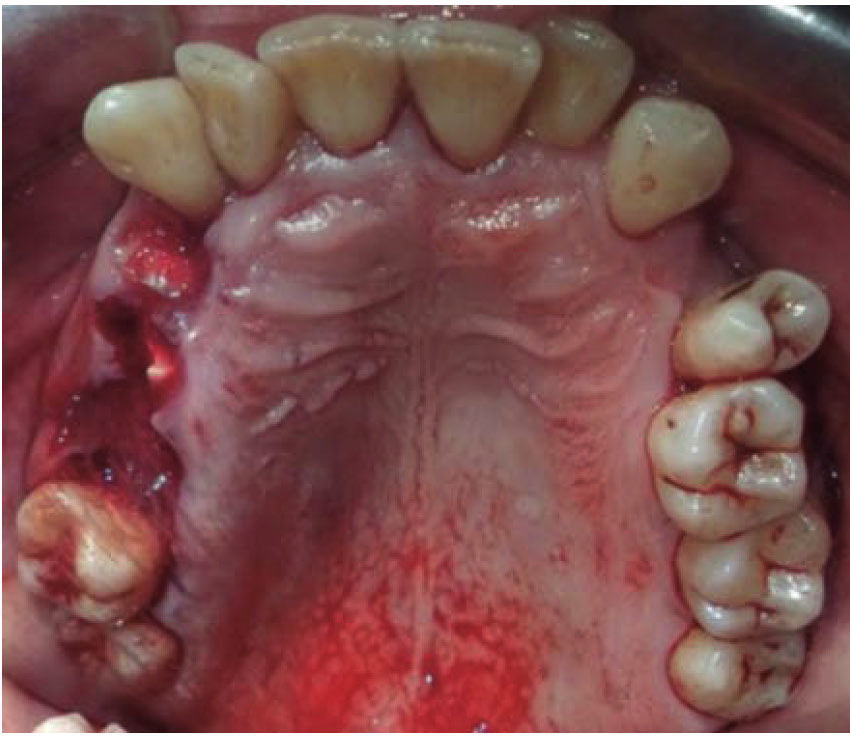
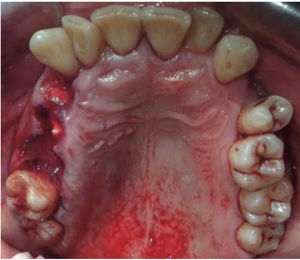
CLINICAL CASESClinical case 1The first case was that of a 30 year old male, with diagnosis of fracture of left mandibular body caused by firearm. The patient was assaulted after a fight which took place when he was leaving a nightclub, he received a bullet shot at a 4 meter distance. Patient exploration revealed edema at cervical, middle third and lower facial levels; he exhibited entry orifice at the left genial region and exit wound at the right submandibular level (Figure 4). Intraoral examination revealed a wound in the mandibular alveolar process at the fracture line, and absence of teeth (Figure 5). Treatment was initiated under general anesthesia with airway stabilization provided by tracheotomy. Debridement of wound edges was performed locally, with surgical soap washes, physiological solution and wound suture. After soft tissue treatment was completed, initial occlusal stability was attempted with an Erich-type bar arch. The patient was hospitalized under a therapeutic scheme of immunization, antibiotics and analgesics.
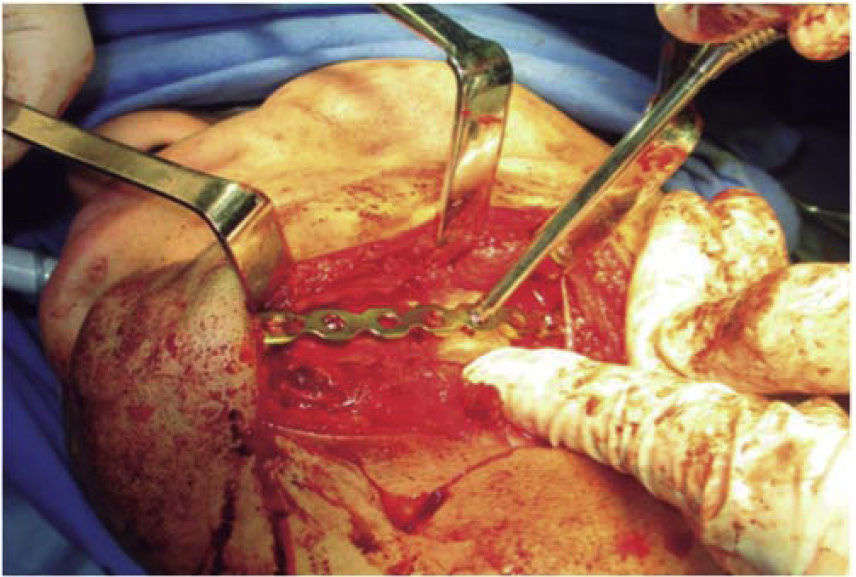
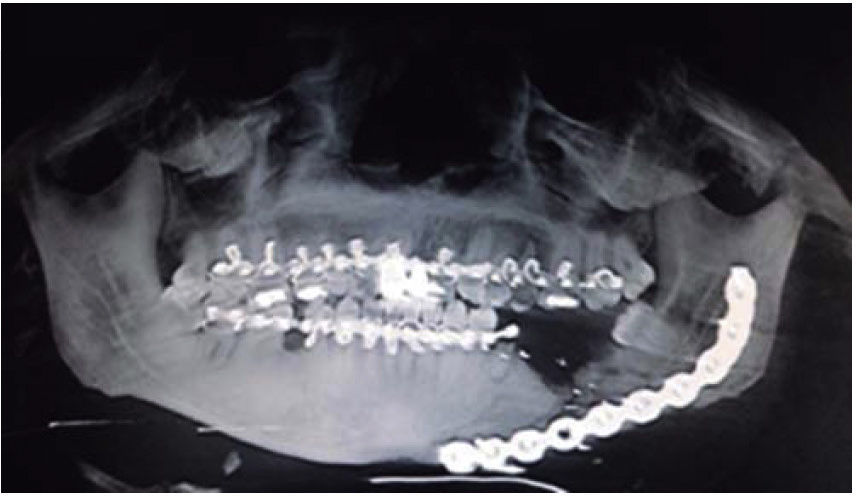
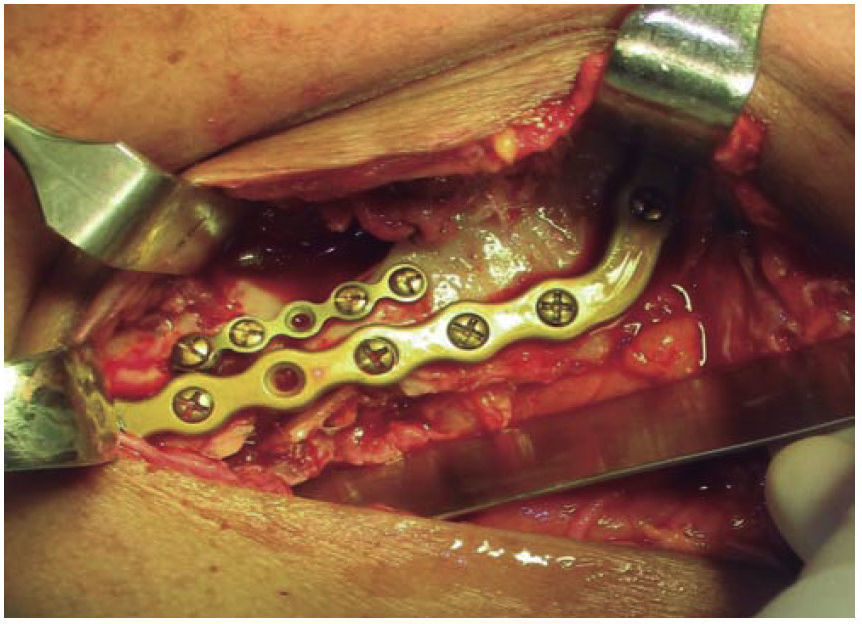
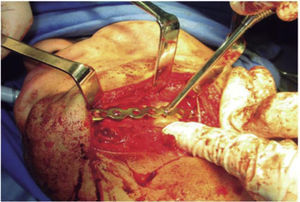
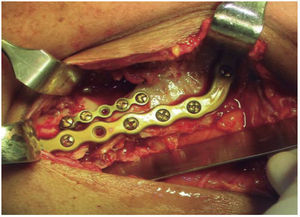
The second surgical event took place seven days later, performing extraoral approach. The fracture was reduced and bone edges were fixated with a 2.4 precontoured mandibular reconstruction plate (Figure 6). Occlusal stability was verified before suturing tissues and bar arches were removed (Figure 7). The patient remained in hospital for seven days, after which he showed suitable occlusion and appropriate healing. Suture points were then removed, a control study was performed and the patient was discharged. The patient did not attend control visits due to the fact that he was incarcerated.
Clinical case 2A 48 year old male arrived for treatment with diagnosis of facial wound caused by firearm. He was assaulted by a third party in the street. He did not inform of the shooting distance. The patient exhibited a projectile entry wound at the right genial region and no exit wound (Figure 8). Intra oral examination revealed a wound in the right cheek, tooth fracture at the level of the upper right hemi-arch, with fractures at the dental neck of first and second premolars and first molar (Figures 9 and 10) involvement. Under local anesthesia, the wound was washed with surgical soap and abundant physiological solution. The tongue was superficially dissected, the bullet was extracted (Figure 11), hemostasis was performed and wounds were sutured. Tooth remains were considered rests and deemed unable to be restored, for that reason they were extracted. The patient attended periodic evaluations with suitable healing of soft tissues and alveolar process. The patient refused implant therapy due to financial considerations, he was thus referred to be rehabilitated with a removable prosthesis.
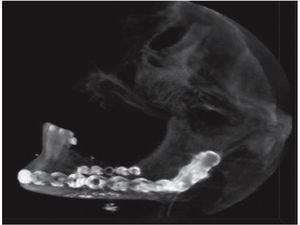
Clinical case 3A 73 year old female with diagnosis of fracture of left mandibular body due to firearm projectile (Figure 12). The patient informed she was assaulted in the street, and upon offering resistance to the theft of her vehicle, she was shot at a distance of two meters. She arrived at our institution eigt days after the assault, having previously been treated in another hospital. Physical exploration revealed hyperemic area and volume increase in fluctuating left submandibular region; entry orifice at left submandibular level with presence of fetid whitish secretion and closed exit wound at right cervical level. Intraoral examination revealed partial edentulism, with multiple maxillary septic foci, and at the left mandibular fornix, a root remnant of the first molar in the fracture line as well as accentuated mobility of the mandibular segment caused by fracture which hindered deglutition.
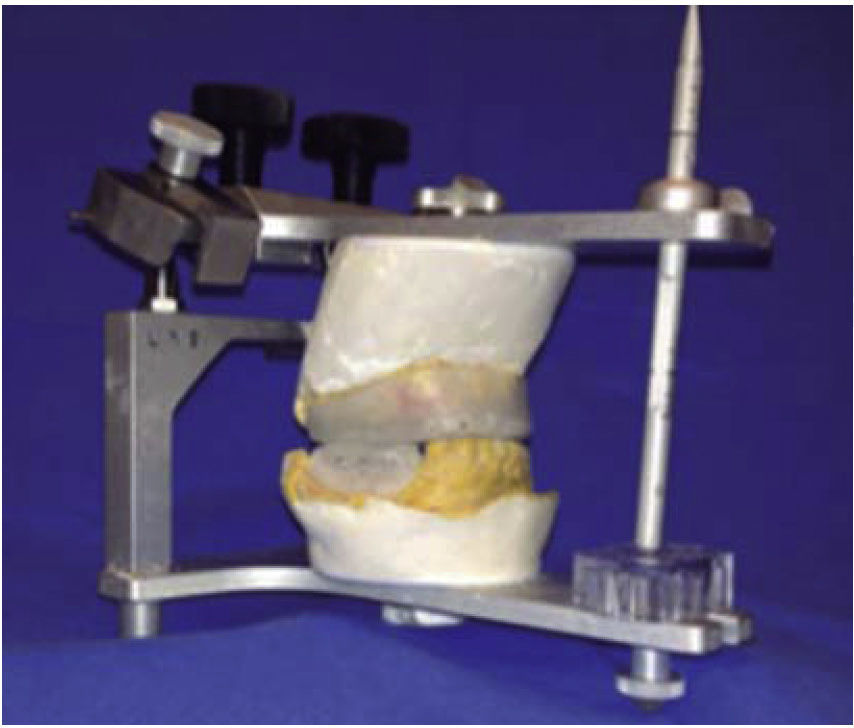
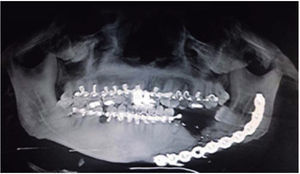
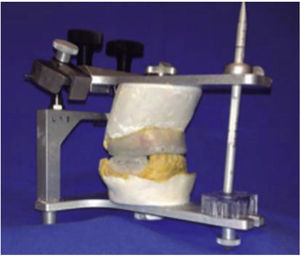
Treatment was initiated with immunization, antibiotic therapy, analgesia, extraction of septic foci and mechanical cleansing of the wound. The patient lacked removable or partial prostheses, so in order to establish inter-maxillary relationship and facial height, gunning splints were manufactured in order to establish inter-maxillary relationship (Figure 13). After ten days of initial treatment, the patient exhibited suitable alveolar healing, with presence of non-fetid secretion at the level of the mandibular wound. The second procedure was then undertaken with extra-oral approach; a 2.4 mandibular reconstruction plate and a 2.0 bone segment plate were used (Figures 14 and 15). The patient was discharged, and she attended periodic assessment visits which showed suitable healing (Figure 16) and adequate mandibular mobility. Three weeks after reconstruction, the patient was instructed to initiate prosthetic treatment in order to achieve rehabilitation.
DISCUSSIONControversy exists on the number of phases or surgical times required in order to attain satisfactory results in patients with firearm wounds. At one initial point in time, it was common to treat all patients in two phases, separated by 2 or 3 weeks; this would generate lesser quality scars and important tissue contraction. Stefanopoulos and Motamendi recommended immediate treatment of all lesions in order to improve functional and esthetic results.3,20 They agreed with Holes in leaving secondary treatments only for complex cases which involved reconstruction with bone grafts, myocutaneous flap rotation or micro-vascularized flaps.14,15 There is also a radical trend to conduct complex cases in one single initial phase, which includes harvesting of free grafts.21
Kasanjian and Converse avoided conducting immediate reconstructions bearing in mind risk of infection, nevertheless, this was proven to be unfounded.6,15 Conversely, suitable initial treatment is of the utmost importance, especially in the case of intraoral wounds, as well as fracture stabilization to decrease risk or as part of resolution in infectious complications. Cunningham et al recommended a more conservative approach, conducting treatment in several phases in cases of severe contamination or poor systemic circumstances which might cause failure of primary reconstruction.9,16 Leon et al considered suitable to conduct initial treatment and wait 6 to 18 days to undertake fracture treatment. This time frame allows to control infection, decrease edema and venous congestion and improve microvascular circulation.7 Our opinion is that it is viable to conduct an initial complex treatment in one single phase, in cases when patients are in a trauma-specialized center, with multi-disciplinary personnel frequently treating these type of cases. In our case, care provided was within a General Hospital, where frequency of this type of problems was not very common, therefore, we decided to conduct treatment in two surgical phases whenever the defect was large or there were infection complications. Concurring with several authors,14,21 we stress the need to conduct a cone-beam or axial topographic study in order to determine damage to hard tissue and location of the projectile in cases when there is no exit wound. All patients suffering firearm wounds must receive multi-disciplinary treatment in a trauma center.
In all three presented cases, treatment was initiated with cardio-pulmonary evaluation, including airway management, hemodynamic control, ventilation, neurological disability and specific damage.9–11 Physical exploration provides information on damage extension in tissues, as well as presence of entrance and exit wounds, in order to discard presence of the bullet within a cavity or tissue (case 2). Maxillofacial treatment is initiated with conservative debridement, cleansing, extraction of root remnants, suture and occlusal stabilization. Fracture reduction and fixation (cases 1 and 3) were conducted with reconstruction plates in a second surgical phase. In all cases here presented, suitable evolution was observed as well as favorable bone healing and the need to continue with oral rehabilitation processes with prostheses or bone-integrated implants. Complications and sequels are common and generally caused by the severity of initial lesions, and delays of treatment caused by life-threatening circumstances or systemic situation of the patient.
CONCLUSIONSMaxillofacial wounds caused by firearms are relatively common in our country. They cause life-threatening severe facial trauma. Treatment of these lesions is similar to that generally used in facial trauma. This treatment represents a challenge in the health area, which has to conduct interdisciplinary treatment from the beginning.
Selection of therapeutic course depends on many factors such as experience, availability of means, lesion extension and general health circumstances of the patient. In cases 1 and 3, which exhibited mandibular fracture, it was observed that treatment in two phases, with a time frame of 7 to 20 days between them, provided suitable esthetic and functional results.
Graduate student at the Oral and Maxillofacial Surgery Program, School of Dentistry, National University of Mexico (UNAM).
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam