By May 5 2023, WHO announced the end of the pandemic due to declining COVID-19 cases and deaths, coupled with high levels of immunity from vaccination and previous infections. However, the virus remains a global health threat with potential for new variants. Acupuncture, a traditional Chinese medicine technique, has shown promise in treating various conditions, including respiratory infections. This review investigates acupuncture's impact on acute COVID-19 infection and its potential as a complementary therapy.
MethodologyA comprehensive literature search was conducted using PubMed, Science Direct, Scielo, and CNKI, focusing on the impact of acupuncture on COVID-19 patients.
ResultsThe search yielded 35 studies, with five meeting the inclusion criteria. These included two randomized clinical trials and three case reports, all incorporating acupuncture alongside conventional treatments.
Case reports and clinical trials indicated that acupuncture improved symptoms such as shortness of breath, rapid heart rate, and cough in COVID-19 patients. Acupuncture was associated with elevated SpO2 levels, reduced heart rate, and an anti-inflammatory effect. Studies highlighted that acupuncture may activate neuro-immune pathways, leading to modulation of immune responses.
Common acupuncture points used included S 36 Zú sān l¿, and LI 4 Hé g¿. Techniques involved inserting needles at specific depths and angles to achieve the Deqi sensation, with treatments lasting 20–30 min per session.
ConclusionAcupuncture appears to be a valuable complementary therapy for managing acute COVID-19 infection. It enhances clinical outcomes by alleviating symptoms and reducing recovery time. Further research is warranted to fully integrate acupuncture into standard COVID-19 treatment protocols.
El 5 de mayo de 2023, la OMS anunció el fin de la pandemia debido a la disminución de casos y muertes por COVID-19, junto con altos niveles de inmunidad por vacunación e infecciones previas. Sin embargo, el virus sigue siendo una amenaza para la salud global con potencial para nuevas variantes. La acupuntura, una técnica de la medicina tradicional china, ha mostrado potencial en el tratamiento de diversas condiciones, incluidas las infecciones respiratorias. Esta revisión investiga el impacto de la acupuntura en la infección aguda por COVID-19 y su potencial como terapia complementaria.
MetodologíaSe realizó una búsqueda exhaustiva de literatura en PubMed, Science Direct, Scielo y CNKI, centrándose en el impacto de la acupuntura en pacientes con COVID-19.
ResultadosLa búsqueda arrojó 35 estudios, de los cuales cinco cumplían con los criterios de inclusión. Estos incluían dos ensayos clínicos aleatorizados y tres informes de casos, todos incorporando la acupuntura junto con tratamientos convencionales.
Los informes de casos y los ensayos clínicos indicaron que la acupuntura mejoró síntomas como dificultad para respirar, frecuencia cardíaca rápida y tos en pacientes con COVID-19. La acupuntura se asoció con niveles elevados de SpO2, reducción de la frecuencia cardíaca y un efecto antiinflamatorio. Los estudios destacaron que la acupuntura puede activar vías neuro-inmunes, lo que lleva a la modulación de las respuestas inmunitarias.
Los puntos de acupuntura comunes utilizados incluyeron S 36 Zú sān l¿ y LI 4 Hé g¿. Las técnicas involucraron la inserción de agujas a profundidades y ángulos específicos para lograr la sensación Deqi, con tratamientos de 20–30 minutos por sesión.
ConclusiónLa acupuntura parece ser una terapia complementaria valiosa para el manejo de la infección aguda por COVID-19. Mejora los resultados clínicos al aliviar los síntomas y reducir el tiempo de recuperación. Se necesita más investigación para integrar completamente la acupuntura en los protocolos estándar de tratamiento del COVID-19.
The emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for COVID-19, was first noted in December 2019 in Wuhan, China.1 The World Health Organization (WHO) declared the COVID-19 outbreak a pandemic on March 11 2020.2 On May 5 of 2023, the WHO officially declared the end of the pandemic due to the declining COVID-19 deaths, hospitalizations, intensive care unit admissions, and high levels of immunity from vaccination and previous infections.3 In April 21 of 2024, the number of COVID-19 infections and deaths stopped being officially reported daily with a final count of 775,364,261 cases and 7,046,320 deaths worldwide.4 However, this does not mean the virus is no longer a threat to global public health. It continues to claim lives worldwide, with the possibility of new variants emerging and leading to additional cases and deaths.5 Moreover, the COVID-19 is the third major coronavirus outbreak6–8 and researchers are systematically trying to predict future pandemics.9–12
Given the threat still posed by COVID-19 and the need to brace for similar future challenges, it is crucial to understand which strategies effectively assist in combating the disease and contribute to improved health outcomes.
Acupuncture, a traditional Chinese medicine therapeutic technique, involves the precise insertion of fine needles into specific points along the body's channels, where it is believed that qi, or life energy, flows.13,14 Its objective is to regulate the nervous, circulatory, endocrine, and exocrine systems, ultimately fostering a heightened sense of well-being.15 Acupuncture is well known for relieving pain16 but seems to possess other applications from osteoporosis17 to insomnia18 and infertility.19 Although few studies exist, acupuncture is suggested to have positive effects on respiratory virus infection.20,21 This review seeks to investigate the impact of acupuncture on acute COVID-19 infection and to discern its potential complementary role in the treatment of these patients.
MethodologyFor this review, we searched prominent databases including PubMed, Science Direct, the Scientific Electronic Library Online (Scielo), and the China National Knowledge Infrastructure (CNKI) for articles investigating the impact of acupuncture on patients diagnosed with COVID-19. The search strategy employed the following formula: “Acupuncture AND ((SARS-CoV-2) OR (COVID-19))”.
Inclusion and exclusion criteriaOriginal clinical research studies in patients infected with COVID-19 were included. We excluded studies of acupuncture for Post-COVID-19 sequelae, LONG-COVID, and prevention.
ResultsOur search yielded a total of 35 studies of which only 5 met the inclusion criteria. The studies investigated the impact of acupuncture on COVID-19 patients.
Methodologically, two studies utilized a randomized clinical trial design, while three were based on case reports. All studies incorporated acupuncture alongside conventional treatments. Among them, three studies combined acupuncture with Chinese herbal medicine, while two studies solely utilized acupuncture.
DiscussionA case report by Yin et al.22 describes the case of an older patient (81 years-old, female) with severe COVID-19, infected at the beginning of 2020. A comprehensive medical approach was conducted with laboratory and imaging test being conducted. The patient received conventional treatment plus acupuncture and herbal medicines as adjuvant treatment. The acupuncture treatment was focused on improving the patient's critical clinical symptoms, such as shortness of breath, rapid heart rate, and lack of appetite. The authors indicate that acupuncture significantly alleviated the patient's respiratory distress, elevated SpO2 (peripheral capillary oxygen saturation) levels, and reduced heart rate. Concurrently, acupuncture induced a sense of calmness in the patient while demonstrating an anti-inflammatory effect. According to the review by Li et al.,23 acupuncture activates various neuro-immune pathways, such as the cholinergic anti-inflammatory pathway, the vagus-adrenal medulla-dopamine pathway, the sympathetic pathway, and the hypothalamus-pituitary–adrenal axis. This stimulation leads to the modulation of immune cells through the release of essential neurotransmitters and hormones. These effects produced by acupuncture provide a scientific foundation and perspective for the clinical utilization of acupuncture across diverse inflammatory conditions.
The case report by Tao et al.,24 also describes the application of acupuncture and herbal medicines as an adjuvant therapy in the treatment of a COVID-19 patient (64 years-old, female). As the previous case, the authors note significant improvement in clinical symptoms, including cough and sputum, following initial treatments. By the tenth day, the patient had fully recovered, with no residual shortness of breath or cough, a conclusion supported by CT imaging. The integrated approach notably accelerated the overall recovery process. In fact, research has shown that acupuncture can reduce the levels of C-reactive protein (CRP), interleukin-6 and 10 (IL-6, IL-10), and tumor necrosis factor-α (TNF-α), which explains why it can enhance the prognosis of respiratory infections.
The study Gong et al.25 proceeds to report two COVID-19 cases treated with an integrative approach of conventional medicine and Chinese medicine (acupuncture + herbal medicine). The main objective of the intervention was to achieve a quicker recovery of the physical strength, the restoration of immunity and elimination of epidemic toxins in these two patients (81 and 72 years-old, both female). Furthermore, specific symptoms such as hypertension and depression were also managed, given their potential to hinder recovery or exacerbate the clinical condition. Cardiovascular conditions, especially hypertension, are risk factors that exacerbate the prognosis of COVID-19 infections.26,27 Similarly, mood disorders like depression are linked to immune dysregulation and inflammation.28 This personalized and comprehensive approach exemplifies the holistic principles of Chinese medicine, strengthening its role as a complementary therapy.
In this study, authors observed that the synergistic effect of treatments might help prevent the progression of disease, lower fatality rates, and enhance curative outcomes.
Helianthi et al.29 developed a single-blinded randomized clinical study to evaluate the impact of combining acupuncture and pharmacologic treatment on hospitalized COVID-19 patients with mild to moderate symptoms. After the intervention period, laboratory analyses revealed that the experimental group experienced an increase in lymphocyte count and erythrocyte sedimentation rate, whereas both parameters were decreased in the control group. However, the differences were not statistically significant. One cause of low lymphocyte levels in COVID-19 patients is the increase in pro-inflammatory cytokines like TNF-α and IL-6. TNF-α suppresses blood cell production and can cause low blood cell counts. IL-6 is linked to reduced effectiveness of T cells and NK cells. High levels of these cytokines also stimulate the production of granulocytes and myeloid cells while suppressing lymphocyte production in the bone marrow. This leads to higher monocyte and granulocyte counts, more cytokines, and fewer lymphocytes.30
The C-reactive protein and ferritin levels decreased in both groups and the differences were also not statistically significant. Finally, the experimental group showed a statistically significant reduction in the duration of cough symptoms compared to the control group. Similar to the previous studies reported in this review, upper respiratory symptoms such as cough could be associated with the prognosis of recovery. Therefore, acupuncture appears to provide significant relief and aid in the recovery of COVID-19.
The three-arm assessor-blinded randomized controlled trial by31 compared the effectiveness of acupuncture and warm cupping, both combined with conventional treatment, to conventional treatment alone in preventing the progression of COVID-19 among hospitalized patients with moderate-to-severe infection.
Results demonstrated a significant improvement in SpO2 and respiratory rate in the acupuncture and cupping groups but no differences in the control group (conventional treatment only). Recovery time was also significantly shorter for both experimental groups in comparison to the control group.
After 7 days of intervention, the severity score of dyspnea, chest tightness, dry cough, and wet cough declined significantly among all three groups, except wet cough in the control group. However, after 3 days of intervention, reduction of the severity score of all symptoms was statistically greater in both acupuncture and cupping groups in comparison with the control group. As well, after 3 days of intervention, results show a significant reduction in the severity scores for weakness, sore throat, myalgia, anorexia, and headache in all three groups, except for sore throat in the control group. This significant improvement persisted up to day 7 of the intervention. However, symptom severity improved more in the experimental groups compared to the control for all symptoms.
Serious adverse events such as ICU admission, intubation or death was also significantly lower in the experimental groups in comparison to the control group.
This clinical research confirmed that the two non-pharmaceutical therapies, warm cupping and acupuncture, offer opportunities to improve respiratory signs, reduce hospitalization duration and serious adverse events, and alleviate symptoms in COVID-19 patients.
In fact, combining acupuncture with standard care in respiratory diseases seems to reduce cytotoxic T lymphocyte CD8+ levels, which are associated with airway inflammation and obstruction, improves the CD4+/CD8+ T-cell ratio, and enhances respiratory functions, according to the study of Wu et al.32 As well, the study of Qin et al.33 showed that acupuncture significantly improves spirometry parameters (FEV1, FVC, and PEF), anti-inflammatory biomarkers (IL-4, IL-8, and interferon gamma), and T-cell counts (CD3+ and CD4+/CD8+ ratio). Additionally, Wei et al.34 demonstrated that acupuncture reduces hypersensitivity, inflammation, and excessive mucus in airways by regulating serum cytokine levels.
Since high levels of TNF-α and IL-6 are linked to higher mortality rates in COVID-19 patients,35,36 by inhibiting macrophage activation and regulating proinflammatory cytokines, acupuncture may assist in reducing hospitalization duration, ICU admission rates, and mortality in COVID-19 patients.
Acupuncture methodologiesYin et al.22 and Tao et al.24 used the same acupuncture methodology.
Bilateral acupuncture points K 3 Taì xī, Dàixiè, and Zhichuan were selected for the acupuncture treatment. The insertion depth varied between 15 to 25 mm, depending on the specific point, with twisting and lifting motions applied until the Deqi reaction was achieved. Disposable filiform needles with a gauge of 0.25 mm × 40 mm were used. Needling was performed for approximately 15–30 s before removing the needles. Acupuncture sessions were conducted daily.
Tao et al.24 provides more information in their study about needle insertion. At K 3 Taì xī on the left side, the needle was inserted obliquely with the tip pointing towards the proximal direction. Conversely, at K 3 Taì xī on the right side, the needle was inserted obliquely with the tip pointing towards the distal direction, facilitating the regulation of qi by ascending on the left and descending on the right. For Dàixiè and Zhichuan points, the needles were inserted perpendicularly to a depth ranging from 12.5 mm to 25 mm.
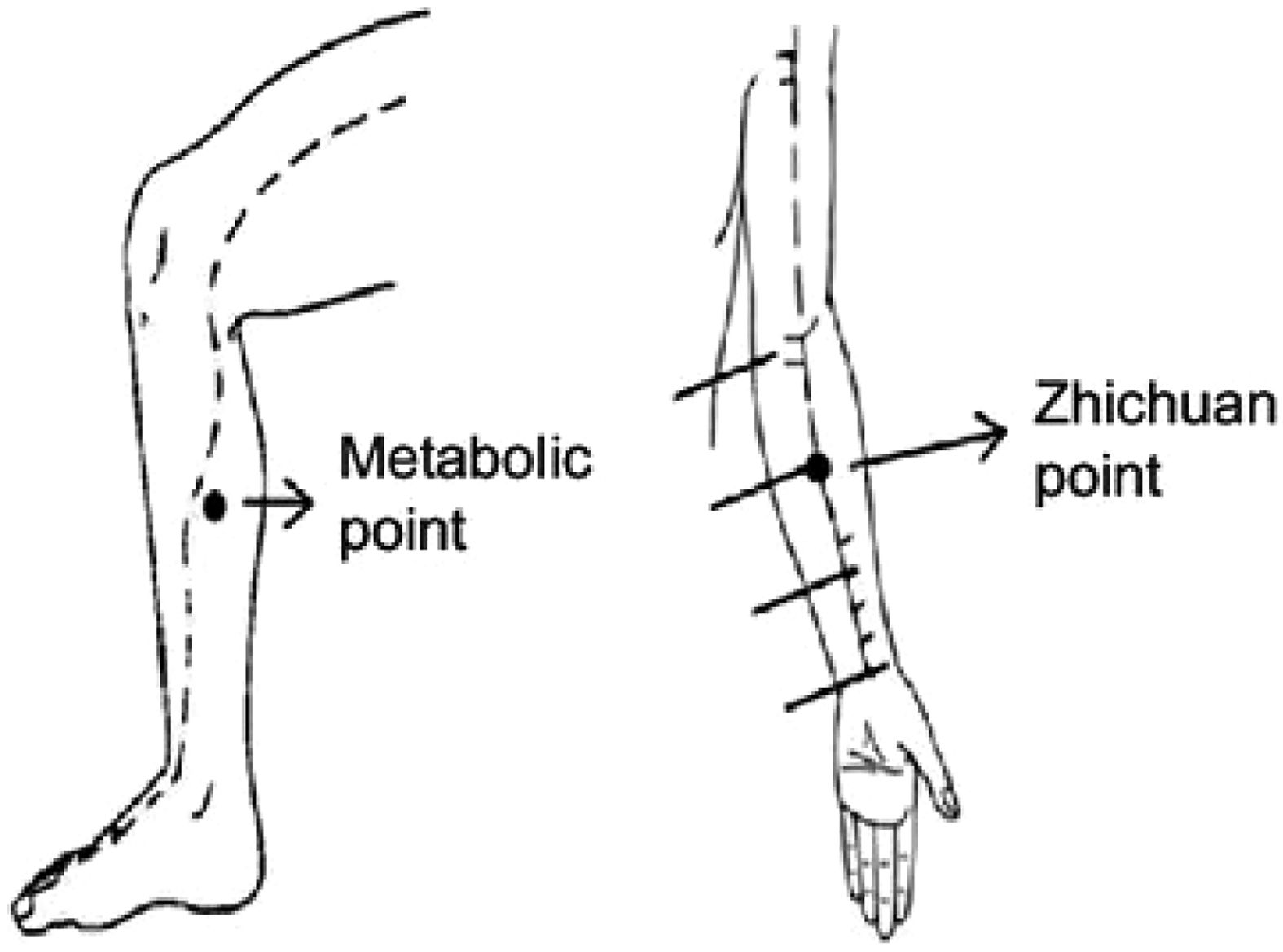
Dàixiè is an empirical point, situated along the midline of the inner aspect of the leg, 8 cun above the tip of the medial malleolus, positioned at the posterior border of the leg's inner aspect, intersecting with the liver meridian of foot-jueyin. It is commonly used for treating loss of appetite, poor appetite, weakness, and fatigue. Zhìchu¿n is another empirical point, located on the palm side of the forearm, positioned along the line between PC 3 Qū zé and PC 7 Dà líng, specifically on the upper one-third of the line between the wrist transverse crease and the elbow transverse crease. It is usually employed for addressing the lack of consciousness, heart palpitations, chest tightness, and shortness of breath.22 Visual localization is provided in Fig. 1.
Localization of Dàixiè (metabolic point) and Zhichuan. Adapted from Yin et al.22
During the treatment regimen in the study of Gong et al.,25 specific acupuncture points were targeted, including S 36 Zú sān l¿, Sp 6 Sān yīn jiāo, Li 3 Taì chōng, LI 4 Hé g¿, L 7 Liè quē, PC 6 Nèi guān, and LI 11 Qū chí.
Needles were inserted at various depths and angles depending on the acupuncture point. For S 36 Zú sān l¿, Sp 6 Sān yīn jiāo, Li 3 Taì chōng, LI 4 Hé g¿, PC 6 Nèi guān, and LI 11 Qū chí, needles were inserted perpendicularly at a 90-degree angle, with depths ranging from 25 to 35 mm. However, for L 7 Liè quē, needles were inserted obliquely at a 15 to 30-degree angle, with the tip directed towards the elbow, at depths of 5 to 10 mm. During the procedure, an even needling technique was employed, and the depth of insertion was adjusted to achieve the deqi sensation. Stimulation and manipulation of acupuncture points occurred once every 10 min.
Disposable needles 0.25 mm × 40 mm was utilized for the treatment sessions. Each acupuncture session lasted for 30 min.
The treatment schedule consisted of daily sessions for 12 consecutive days, continuing until the patient was discharged. Following every 12 acupuncture treatments, a 3-day interval was observed before commencing the next course of treatment.
As for the treatment regimen of Helianthi et al.,29 specific acupuncture points included LI 4 Hé g¿, LI 11 Qū chí, and S 36 Zú sān l¿. For each point, the needle was inserted and then stimulated by twirling it once. Disposable acupuncture needles with a diameter of 0.25 mm and a length of 25 mm were used. Each treatment session lasted for 30 min. The frequency of treatments involved three sessions per week for a period of two weeks.
In the study of Alipour et al.,31 the treatment protocol employed specific acupuncture points including GV 20 B¿i huì, L 5 Ch¿ zé, L 7 Liè quē, LI 4 Hé g¿, Li 3 Taì chōng, Li 14 Qí mén, CV 12 Zhōng w¿n, CV 17 shān zhōng, and S 36 Zú sān l¿.
For Li 3 Taì chōng, LI 4 Hé g¿, S 36 Zú sān l¿, and L 5 Ch¿ zé, the needles were inserted perpendicularly at a 90-degree angle to the skin, reaching a depth of 20–25 mm. However, at GV 20 B¿i huì, L 7 Liè quē, CV 12 Zhōng w¿n, CV 17 shān zhōng, and Li 14 Qí mén, the needle was inserted obliquely at a 15–30-degree angle, with the needle tip directed towards the elbow at L 7 Liè quē and towards the distal point at other locations, reaching a depth of 5 to 10 mm.
Acupuncture points, except GV 20 B¿i huì, were stimulated and manipulated after 10 min using an even manipulating technique, involving 10-s intervals of twirling and up-and-down movement. Disposable stainless-steel needles with a diameter of 0.25 mm and a length of 40 mm were utilized. Each treatment session lasted for 20 min. Treatment frequency involved daily sessions for a duration of 3–7 consecutive days, depending on the patient's hospitalization period, starting from the first day of hospitalization and continuing up to a maximum of the seventh day of hospitalization.
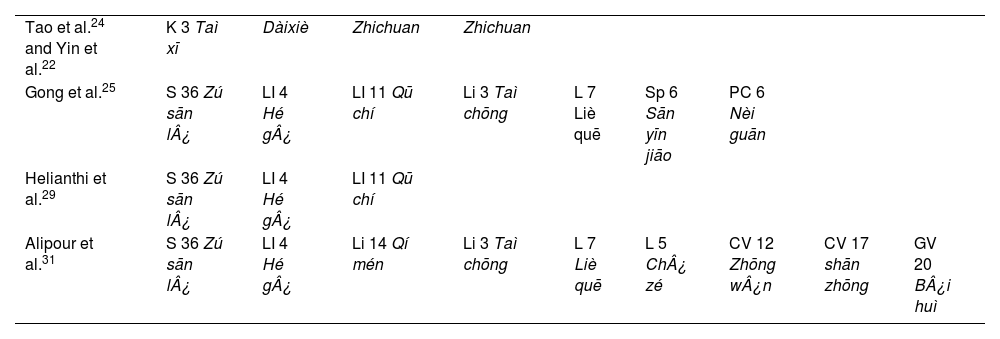
Among the studies included in this review, we noticed the predominant use of some acupuncture points (Table 1).
Acupuncture points used in the reviewed studies.
| Tao et al.24 and Yin et al.22 | K 3 Taì xī | Dàixiè | Zhichuan | Zhichuan | |||||
| Gong et al.25 | S 36 Zú sān l¿ | LI 4 Hé g¿ | LI 11 Qū chí | Li 3 Taì chōng | L 7 Liè quē | Sp 6 Sān yīn jiāo | PC 6 Nèi guān | ||
| Helianthi et al.29 | S 36 Zú sān l¿ | LI 4 Hé g¿ | LI 11 Qū chí | ||||||
| Alipour et al.31 | S 36 Zú sān l¿ | LI 4 Hé g¿ | Li 14 Qí mén | Li 3 Taì chōng | L 7 Liè quē | L 5 Ch¿ zé | CV 12 Zhōng w¿n | CV 17 shān zhōng | GV 20 B¿i huì |
S 36 Zú sān l¿ was used in 3 studies.25,29,31
S 36 Zú sān l¿ is positioned within the tibialis anterior muscle, approximately four fingers below the lower margin of the patella and one finger lateral to the anterior border of the tibia. According to Chinese medicine theory, it is believed to fortify the spleen and stomach, promote meridian relaxation, activate collaterals, and enhance overall bodily strength.
The study of Lou et al.37 suggest that S 36 Zú sān l¿ and Sp 6 Sān yīn jiāo suppress the TLR4/NF-κB pathway in alveolar monocytes/macrophages and reduce the expression of TNF-α, IL-1, IL-6, and MPO during acute lung injury. This leads to the relief of pulmonary interstitial edema, alveolar congestion, and bleeding, thus restoring the damaged alveolar structure. Additionally, acupuncture at Feishu (BL13) and S 36 Zú sān l¿ boosts the accumulation of HO-1 and Nrf2 proteins in the nucleus by modulating the Nrf2/HO-1 pathway via the p38 MAPK signaling pathway. This further reduces the release of TNF-α, IL-1β, and IL-6 in lung tissues and plasma. Consequently, this anti-inflammatory effect helps prevent lung damage caused by the excessive release of oxygen free radicals and inflammatory factors in the ischemic region.38
As well, LI 4 Hé g¿ was used in 3 studies.25,29,31 This acupuncture point is the yuan (source) point of the Large Intestine channel of hand-yangming. It is located at the midpoint of the radial side of the second metacarpal bone.
LI 4 Hé g¿ seems to stimulate a molecule called peroxisome proliferator-activated receptor γ, which acts as a brake on the TLR4/NF-κB pathway. This slows down the TLR4/MyD88 signaling process, switching alveolar macrophages from the harmful M1 type to the beneficial M2 type. Consequently, this reduces the activity of the NF-κB pathway and decreases the release of inflammatory substances like TNF-α, IL-1β, and IL-6. This overall effect helps alleviate acute respiratory distress syndrome.39
According to Li et al.,23 the acupuncture points commonly used for various inflammatory respiratory diseases often include B 13 Fèi shū, S 36 Zú sān l¿, and LI 4 Hé g¿.
Final remarksThis review highlights the potential of acupuncture as a complementary therapy in the treatment of acute COVID-19 infection. The studies reviewed demonstrate that acupuncture, particularly when used in conjunction with conventional treatments, can significantly improve patient outcomes by alleviating respiratory symptoms, reducing inflammation, and enhancing overall immune function.
The consistency in the use of specific acupuncture points, such as S 36 Zú sān l¿, and LI 4 Hé g¿, underscores their importance in treating inflammatory respiratory conditions.
Given the threat of COVID-19 and the potential for future pandemics, it is crucial to explore and integrate effective complementary therapies like acupuncture into mainstream medical practice.
However, the main limitations of this review include the small number of available studies, the heterogeneity of patient groups, and the variability in treatment protocols. To confirm these findings and establish standardized acupuncture guidelines for respiratory infections, including COVID-19, further rigorous clinical trials and research are essential.
Overall, acupuncture offers a promising complementary approach to enhance the management and treatment of acute COVID-19, contributing to improved patient health outcomes and potentially reducing the burden on healthcare systems.
ConclusionsAcupuncture appears to be a valuable complementary therapy for managing acute COVID-19 infection. It enhances clinical outcomes by alleviating symptoms, reducing inflammation, and supporting immune function. Further research is warranted to fully integrate acupuncture into standard COVID-19 treatment protocols.
FundingThis research received no external funding.
Ethical approvalThis review does not require ethical approval.
CRediT authorship contribution statementPatrícia Soares Bernardo: Conceptualization, Data curation, Formal analysis, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. Jorge Magalhães Rodrigues: Data curation, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.