To evaluate the results of surgical treatment of intraarticular calcaneal fractures, and also to analyse the variables that influence the final clinical and radiological outcomes as well as the complications.
Material and methodsWe retrospectively analysed 86 intraarticular calcaneal fractures in 78 patients, who underwent surgery with an extended lateral approach and reconstruction plate. The mean age was 48 years (16–74 years) and the mean follow-up was 4.6 years (9–99 months); 54 patients (69.2%) suffered falls from less than 3m in height or banal injuries and 24 patients (30.8%) falls from more than 3m in height or high energy-accidents. According to the Sanders classification we operated 12 (15%) type II, 54 (62.8%) type III and 20 (23.2%) type IV fractures.
ResultsThe postoperative mean AOFAS score was 73.9 points, with good or excellent results in 57% of the patients. Twelve cases (14%) suffered surgical wound complications and 11 (12.8%) required subtalar arthrodesis. Significantly better results were obtained in the patients younger than 30 years old, patients that fell from less than 3m in height and patients with Sanders fractures types II and III compared to type IV, which were associated with higher rate of subtalar arthrodesis.
ConclusionsWe consider that open reduction and internal fixation of intraarticular fractures of the calcaneus with reconstruction plate is a valid treatment alternative. Given the complications described and the secondary subtalar arthrodesis rate, we recommend a meticulous technique carried out by experienced surgeons.
Evaluar los resultados del tratamiento quirúrgico de las fracturas intraarticulares de calcáneo. Analizar las variables que influyen en el resultado clínico y radiológico final, así como las complicaciones dadas.
Material y métodosAnalizamos de forma retrospectiva 86 fracturas intraarticulares de calcáneo en 78 pacientes, intervenidas en nuestro servicio mediante abordaje lateral extendido y placa de reconstrucción. La edad media fue de 48 años (16-74 años) y el seguimiento medio de 4,6 años (9-99 meses); 54 pacientes (69,2%) sufrieron caídas de menos de 3 m de altura o traumatismos banales, y 24 (30,8%) de más de 3 m o accidentes de alta energía. Según la clasificación de Sanders, intervinimos 12 fracturas (15%) tipo II, 54 (62,8%) tipo III y 20 (23,2%) tipo IV.
ResultadosLa puntuación AOFAS media postoperatoria fue de 73,9 puntos (42-98 puntos), con resultados buenos o excelentes en el 57% de los casos; 12 casos (14%) presentaron complicaciones a nivel de la herida quirúrgica y 11 (12,8%) precisaron una artrodesis subastragalina. Obtuvimos resultados significativamente mejores en pacientes menores de 30 años, pacientes con caídas de menos de 3 m de altura y pacientes con fracturas tipos II y III de Sanders respecto a las tipo IV, asociándose a estas una mayor tasa de artrodesis subastragalina.
ConclusionesConsideramos la reducción abierta y fijación interna de las fracturas intraarticulares de calcáneo con placa de reconstrucción una alternativa vigente. Dadas las complicaciones descritas y la tasa de artrodesis subastragalina secundaria, recomendamos una técnica meticulosa por parte de cirujanos experimentados.
The bone most commonly injured in the tarsus is the calcaneus, accounting for between 1% and 2% of all fractures. Approximately 75% will be intraarticular, with 10% associated with fracture at rachis level and 26% other fractures at lower limb level.1,2
The great majority of these fractures occur in young people in a working environment, frequently due to haste or high energy accidents, leading to long sick leave and major socio-economic impact.3,4
Intraarticular calcaneal fractures are characterised by current controversy regarding their treatment, since many different solutions and opinions may be encountered for the same fracture.5 However, although authors in the literature agree that available evidence is insufficient to state that surgical treatment is superior to conservative treatment,6,7 the current trend is for open reduction and internal fixation.8–10 Due to orthopaedic surgeons’ fear of the complications described for surgical wounds using the “extended L shaped lateral approach” considered the gold standard surgery,1 minimally invasive techniques are now increasing. Described outcomes are favourable although technically these techniques are more demanding and require a greater learning curve.11
The objectives of surgical treatment are to restore the three-dimensional anatomy of the calcaneus (in height, length and width) and the anatomical reduction of the joint surfaces. Finally, functional restoration is sought as soon as possible, with a stable osteosynthesis.1,12–14
Therefore, given the gravity and complexity of this type of injury, associated with the rate of surgical complications and physical sequelae it may entail, calcaneal fractures continue to be a genuine challenge for the orthopaedic surgeon. The aim of our study is to assess the result of surgical treatment of intraarticular calcaneal fractures, and to analyse the variables which have an influence on obtaining these results. We therefore conducted an retrospective observational study in patients who had undergone surgery for intraarticular calcaneal fractures.
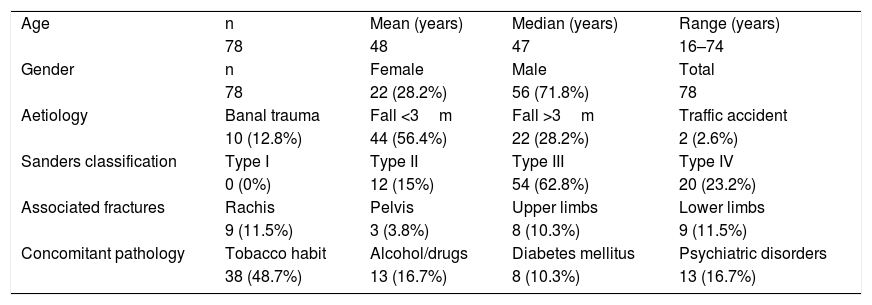
Material and methodsBetween August 2006 and March 2016 a total of 97 consecutive calcaneal fractures were performed in 88 patients (9 bilateral fractures) using an extended lateral “L-shaped” approach and a low profile reconstruction plate. We excluded from the study all patients with fractures which were considered conservative and we included all patients who underwent surgery using the said technique. Ten patients were lost to follow-up: 2 (2.3%) died from non-surgical causes; 3 (3.4%) were patients who were inmates in a prison, who were transferred to centres outside of our healthcare area, and we were unable to locate 5 patients (5.7%). The final sample included 78 patients and 86 intraarticular calcaneal fractures (8 patients with bilateral surgery) whose clinical and radiologic follow-up has been retrospectively analysed.
Out of the 78 patients, 56 (71.8%) were male and 22 (28.2%) female. Mean age at surgery was 48±12.24 years. A total of 53 patients (67.9%) presented with associated comorbidity: 38 patients (48.7%) with a tobacco habit; 20 (25.6%) with a history of psychiatric disorders; 13 (16.7%) with drug or alcohol abuse; 13 (16.7%) with chronic use of corticosteroids; 8 (10.3%) with diabetes mellitus and 8 (10.3%) with infectious-contagious diseases (HIV or hepatitis B or C).
With regard to the production mechanism, 44 (56.4%) of patients suffered from falls of under 3m height and 22 (28.2%) of over 3m. Ten patients (12.8%) presented with fractures after ankle sprain or banal trauma and 2 patients (2.6%) after high energy traffic accidents. Nineteen patients (24.4%) presented with associated fractures: 9 (11.5%) with fractures at rachis level; 9 (11.5%) with fractures in lower limbs; 8 (10.3%) in upper limbs and 3 (3.8%) at pelvic level. Seventeen patients (21.8%) had fractures of both heel bones, and 8 of them underwent bilateral surgery.
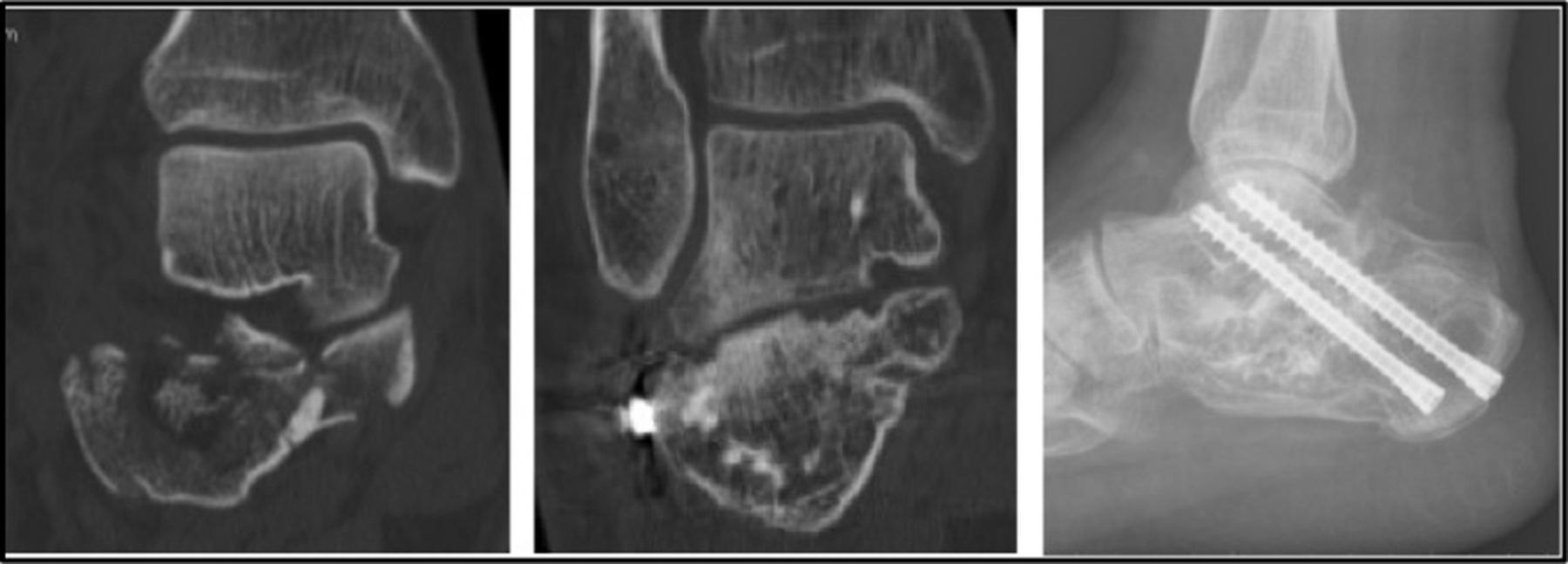
All the fractures were classified in accordance with Sanders15 classification, based on computerised tomography imaging (CAT), resulting in 12 (15%) type II fractures, 54 (62.8%) type III and 20 (23.2%) type IV (Table 1). We measured the Böhler and Gissane angles on the lateral radiographies, obtaining a preoperative mean Böhler angle of 17.1±7.29° and a preoperative mean Gissane angle of 83.3±11.4°.
Demographic data of all patients.
| Age | n | Mean (years) | Median (years) | Range (years) |
| 78 | 48 | 47 | 16–74 | |
| Gender | n | Female | Male | Total |
| 78 | 22 (28.2%) | 56 (71.8%) | 78 | |
| Aetiology | Banal trauma | Fall <3m | Fall >3m | Traffic accident |
| 10 (12.8%) | 44 (56.4%) | 22 (28.2%) | 2 (2.6%) | |
| Sanders classification | Type I | Type II | Type III | Type IV |
| 0 (0%) | 12 (15%) | 54 (62.8%) | 20 (23.2%) | |
| Associated fractures | Rachis | Pelvis | Upper limbs | Lower limbs |
| 9 (11.5%) | 3 (3.8%) | 8 (10.3%) | 9 (11.5%) | |
| Concomitant pathology | Tobacco habit | Alcohol/drugs | Diabetes mellitus | Psychiatric disorders |
| 38 (48.7%) | 13 (16.7%) | 8 (10.3%) | 13 (16.7%) |
n: number of patients.
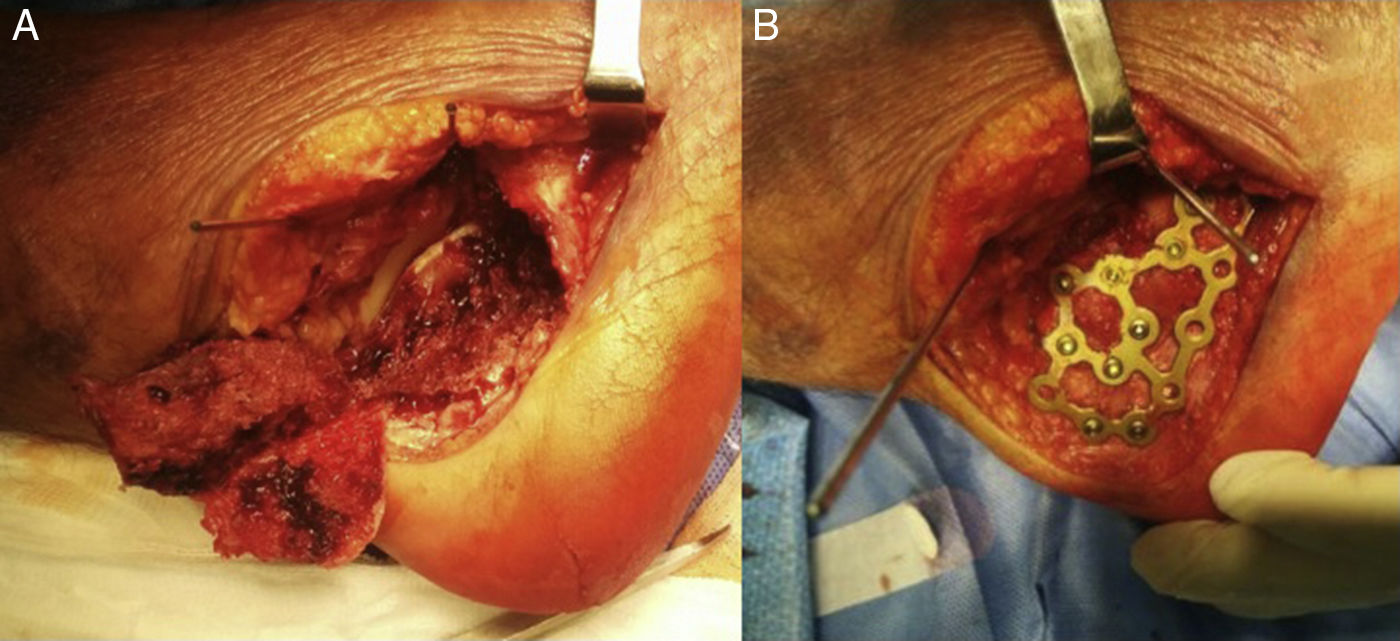
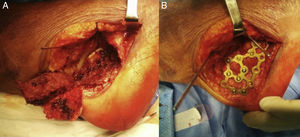
All cases were operated on by the same surgical team. 80.2% of patients were operated on during the first 15 days after the fracture (range between 4 and 22 days), provided that the state of the soft tissues was optimal and the wrinkle test positive. Mean time in surgery was 132±33min. Surgery was performed with the patient in lateral decubitus position, lower extremity ischaemia positioned at thigh level and with intraoperative fluoroscopy control (profile, axial and Broden projections). In order to do this, in all cases, we used the “extended lateral L shaped approach” proposed by Palmer and Letournel and later modified by Benirschke.16–18 We made a complete flap protecting the sural nerve and the peroneal tendons. The fracture was reduced after removal of the side wall (Fig. 1A), beginning with the anterior tuberosity and continuing through the anteromedial articular facets and subtalar joint, finishing in the posterior tuberosity, with provisional attachment using Kirschner needles and with accurate three-dimensional reconstruction of the calcaneus and articular surfaces confirmed by fluoroscopy. After this, after repositioning the side wall in its anatomic location, fixation was performed low profile plates in all cases with non-blocking nails (Synthes Locking Calcaneal Plate®, Synthes USA, Paoli, USA) (Fig. 1B). We inserted a Redon type aspiration drainage system in all patients, which was removed after 48h if it had not been productive. Partial weight bearing was not permitted until the sixth week and complete weight bearing until the 12th week.
Postoperative evaluationAll patients were assessed at 4 weeks, 8 weeks, 3 months, 6 months and subsequently annually for clinical examination and radiographic follow-up. Standard evaluation in each visit included the American Orthopaedic Foot and Ankle Society Score (AOFAS),19,20 taking the score obtained in the last patient check-up in the last consultation considered as the final follow-up. We then analysed the relationship between the score from the AOFAS and each of the different variables: gender, age, presence of comorbidity (tobacco habit, drug or alcohol abuse, a history of psychiatric disorders, diabetes, chronic intake of corticosteroids or infectious and contagious diseases), bilaterality or unilaterality of concomitant fractures, lesional mechanism and classification of fracture according to Sanders. We finally compared the post-surgical radiologic results in the last check up to the preoperative studies by measuring the Böhler and Gissane angles, and we analysed their relationship to final functional results.
Statistical analysisData analysis was performed using the SPSS 22 statistical programme for MAC OS (version 22; SPSS, Chicago, IL, USA). We made a descriptive analysis, expressing the qualitative variables such as absolute and relative frequencies and the quantitative variables such as the mean and standard deviation (SD). We conducted a bivariate study, using the parametric Fisher Student's t-test for the quantitative variables and the non-parametric Mann–Whitney U test for normality of distribution, the parametric Chi-squared test for the qualitative variables and the exact Fisher test for the non-parametric test. The significance level was established at 5%.
ResultsMean follow-up time of the 86 cases (78 patients) was 55±25 months.
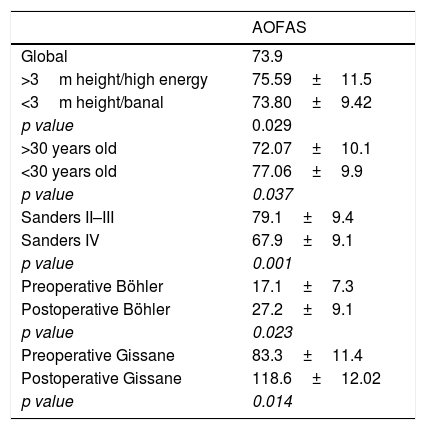
Clinical and radiologic results. The mean AOFAS score obtained was 73.9±10.2 points out of 100 (95% CI: 74.49–78.95 points), with excellent results (90–100 points) in 8 cases (9.3%), good (75–89 points) in 40 (47.7%), acceptable (50–74 points) in 35 (39.5%) and poor (0–49 points) inn 3 cases (3.5%).
The mean postoperative Böhler angle was 27.2±9.1°, and Gissane angle was 118.6±12.02°. We achieved a restoration of the Böhler angle (between 20° and 40°) in 60 patients (69.8%).
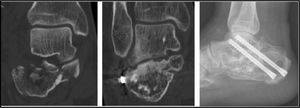
All patients had presented with a complete fracture consolidation at the 6 month check up after surgery. 36 cases (42%) had developed subtalar joint arthrosis which were all found using CAT. In 11 (12.8%), it was necessary to perform subtalar arthrodesis, which was in one of the 12 cases made with Sanders type II fractures (8%), in 5 of the 54 cases with Sanders type III fractures (9%), and in 5 of the 20 cases with Sanders type IV fractures (25%) (Fig. 2).
Complications. Thirteen patients (20.5%) presented with a total of 16 complications; 12 cases (14%) of complications at surgical wound level, 5 (5.8%) cases of superficial infection, treated with surgical cleaning and extraction of osteosynthesis material in 4 cases; 3 patients (3.4%) developed a deep infection or osteomyelitis, all of which were treated with aggressive debridement, extraction of the osteosynthesis material and filling of the defect with antibiotic bone cement. In 2 of these 3 patients, two-stage arthrodesis was performed. In 4 cases (4.7%) a defect in the wound closure occurred without the infection being diagnosed, with treatment being carried out in collaboration with the Ulcer Unit through the application of vacuum therapy. However, in one subject it was necessary to remove the osteosynthesis material and to make a flap closure using plastic surgery. Two patients (2.3%) presented with a neuropathy of the sural nerve; there was one case (1.2%) of Sudeck algodystrophy and one case (1.2%) of calcification at peroneal tendon level treated with surgical tenolysis.
Analysis of resultsStatistical analysis did not reveal any statistically significant differences (p>0.05) in the functional results obtained in the AOFAS test with respect to gender, patients with unilateral fractures versus bilateral, patients with other concomitant fractures or the cohort of patients under 60 compared with those over 60. Neither did we find any significant association between the patients who presented with an associated comorbidity with functional results (p>0.05) or the appearance of complications during follow-up (p>0.05). However, we did obtain significantly better results in patients with falls under 3m height compared with patients with falls of over 3m height or high energy accidents (p=0.029); the cohort of patients under 30 (p=0.037), and patients with Sanders type II and II fractures compared with Sanders type IV fractures (p=0.001). In contrast, we did not find results were better if we compared the patients with Sanders type II fractures to those with type III fractures (p=0.963). The mean difference of the Böhler and Gissane angles was 10.1° (95% CI: 4.3–12.1°) and of 35.3° (95% CI: 29.4–39.1°) respectively, with this improvement being significant (p=0.023 and p=0.014) (Table 2). We did not find any better functional results in the cohort of patients where a reduction in the Böhler angle was obtained (20–40°) (p>0.05).
Correlation between functional outcomes and variables with statistically significant relevance.
| AOFAS | |
|---|---|
| Global | 73.9 |
| >3m height/high energy | 75.59±11.5 |
| <3m height/banal | 73.80±9.42 |
| p value | 0.029 |
| >30 years old | 72.07±10.1 |
| <30 years old | 77.06±9.9 |
| p value | 0.037 |
| Sanders II–III | 79.1±9.4 |
| Sanders IV | 67.9±9.1 |
| p value | 0.001 |
| Preoperative Böhler | 17.1±7.3 |
| Postoperative Böhler | 27.2±9.1 |
| p value | 0.023 |
| Preoperative Gissane | 83.3±11.4 |
| Postoperative Gissane | 118.6±12.02 |
| p value | 0.014 |
p value: statistical significance.
At present there is a tendency among orthopaedic surgeons use surgical treatment for intraarticular calcaneal fractures and specifically open reduction and fixation with a plate with “extended lateral L-shaped approach”.1,6,8–10 Despite this, evidence is insufficient in the literature to support better surgical treatment outcome as opposed to conservative treatment.6,7 In our environment, intraarticular calcaneal fractures are of the few intraarticular fractures which have usually been treated conservatively in a high percentage of cases, specifically 57.98%. This result was obtained through a survey carried out in 29 Spanish hospitals and with a total of 624 fractures.21 This was due to technical complexity and especially to the fear of developing any of the described complications, and in particular those relating to surgical wounds.21 The progression of a subtalar arthrosis was therefore unavoidable due to the unacceptable residual articular congruence, accompanied on many occasions by a non-union with three-dimensional anatomical change of the hindfoot.10,21–23 In their recent meta analysis Luo et al.7 concluded that surgical treatment is not superior to conservative treatment but, despite the lower rate of complications in non-surgical treatment, the risk of subtalar arthrodesis is much higher. In a prospective, randomised controlled study Buckley et al.9 compared the outcome of surgical treatment to conservative treatment, obtaining better clinical results in those patients where anatomical reduction had been achieved, and particularly in those who did not present with occupational disputes. The patients who were conservatively managed were 5.5 times more likely to be operated on again with subtalar arthrodesis. Similarly, Howard et al.24 demonstrated that the patients who had been treated conservatively had five times more risk of subtalar arthrodesis compared to those who underwent surgery. In their study Brauer et al.3 demonstrated a more favourable outcome in cost-effective analysis for surgical treatment. For their part, Radnay et al.22 concluded that arthrodesis was highly complicated in cases which had initially been treated conservatively, demonstrating better outcome and a lower rate of complications in patients who had been treated surgically from the beginning, provided that anatomical parameters had been correctly restored.
In our series, on subdividing the sample according to the type of fracture, we observed that the patients with Sanders type IV fractures presented with poorer clinical outcome than those with types II and III, with scores on the postoperative AOFAS scale of 67.9 points for type IV and 79.5 and 78.1 points for type II and III, respectively. A quarter of cases with Sanders type IV fractures required subtalar arthrodesis compared with 8% and 9% of types II and III, respectively, thereby tripling the risk of arthrodesis. Csziy et al.25 concluded in their study that Sanders type IV fractures had 5.5 times more possibilities of developing subtalar arthrosis. The worst prognosis of Sanders type IV fractures, and of the patients who presented with high energy trauma was due firstly to higher complexity in achieving anatomical reduction of the joint and secondly to the poor viability of the joint cartilage after the initial high energy impact,1,12,22,26 responsible for the post-traumatic joint degeneration, which was irreversible in the medium and long term, regardless of the reduction obtained.
There is currently no consensus regarding the treatment of Sanders type IV fractures. Several authors recommend primary subtalar arthrodesis,15,27 whilst others advocate primary osteosynthesis as having acceptable outcomes.22 Schepers28 published a systematic review of results after primary arthrodesis with excellent outcomes. However, Buckley et al.9 compared the results obtained after primary osteosynthesis to those of primary arthrodesis and found no major improvement in favour of either technique. In contrast, primary arthrodesis is recommended in patients who seek faster functional recovery in their occupational environment and to avoid possible two-stage surgery, with the financial benefit this entails. In our centre, given the results obtained in Sanders type IV fractures, we decided to initially perform osteosynthesis since 3 out of every 4 patients who underwent surgery did not require subtalar arthodesis. Furthermore, we consider it is more technically complex to carry out primary arthodesis as final treatment, because the need to anatomically reconstruct the calcaneus with stable assemblage in addition to the use of necessary bone grafting to achieve arthrodesis, thus increasing time in surgery and potential complications.
The main problem associated with the “extended L-shaped lateral approach” are surgical wound level complications and the rates of these vary between 19% and 23% in the 3 most widely published series.6,9,29 In their series Buckley et al.9 present 17% superficial and 5% deep surgical wound complications. Griffin et al.29 reported problems on the surgical wound level in 19% of cases. For their part, Agren et al.6 presented superficial wound complications in 19% of cases and deep infections in 4% of cases. We had similar results in our series, treating these patients with the Ulcer Unit with vacuum therapy and performing primary surgery with as least trauma possible to the soft tissues, provided that the status of the soft tissues was optimum. In contrast with other authors,24,30 we found no direct relationship between comorbidities and functional outcome, nor with the appearance of complications, although it is true that the control exerted for this type of patient is much narrower.
With regards to the limitations of our study, our case series was analysed descriptively and retrospectively, and is thus prone to the limitations this type of study. The follow-up period is relatively short and heterogeneous among the different patients, which does not allow for long-term evolution. In our study we did not control the interaction and confusion variables, and the differences found in the results could be due to the causes other than surgical treatment. Moreover, we did not make a comparative study with another surgical technique nor identify the intraarticular calcaneal fractures conservatively during this period. One of the advantages of our study is that the number of cases and their heterogeneity is representative for a unit dealing with this type of trauma on a regular basis.
ConclusionsFrom the results obtained in our series, we may conclude that open reduction and internal fixation of intraarticular calcaneal fractures using the “extended L-shaped lateral approach” is a valid alternative. An accurate surgical technique and optimum care of soft tissues is vital due to the frequent surgical wound complications. From the results obtained, we believe that primary osteosynthesis in patients with Sanders IV type fractures is a valid option, although it must be performed by surgeons who are experienced in this technique.
We believe the Sanders classification is an important prognostic factor, as is the lesional mechanism and age of the patients. Poorer functional outcome presents in patients with Sanders type IV fractures, with high energy traumas and the cohort of patients over 30 years of age compared with those under 30. Similarly to Biz et al.31 we found no correlation between the anatomical reduction of the Böhler angle and functional results. For this reason, we believe that this angle has no predictive value as a measurement for outcome following surgery.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments have been performed on humans or animals in this research.
Confidentiality of dataThe authors declare that they have adhered to the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors received no financial assistance for this study nor signed any agreements to receive any benefits or fees from any business entity. Furthermore, no business entity has or will pay any foundations, educational institutions or other non-profit organisations with which the authors are affiliated.
Please cite this article as: Diranzo-García J, Bertó-Martí X, Castillo-Ruiperez L, Estrems-Díaz V, Hernández-Ferrando L, Villodre-Jiménez J, et al. Tratamiento de las fracturas intraarticulares de calcáneo mediante placa de reconstrucción. Resultados y complicaciones de 86 fracturas. Rev Esp Cir Ortop Traumatol. 2018;62:267–273.