Intrapelvic suprapectineal plates play an important role in acetabular fracture fixation. However, the shape of these implants may interfere with the quality of reduction evaluations using plain X-rays. We sought to evaluate this artefact and its relationship with CT findings.
Materials and methodsIn a retrospective, single-centre series of 22 acetabular fractures, postoperative AP, alar and obturator X-ray views and CT images were evaluated by three independent observers. Cohen's kappa was used to examine interrater reliability.
ResultsSuprapectineal plates interfered with the evaluation of the weight-bearing surface in 75.3%, and with all three oblique views in 43.9% of cases. The central segment was most consistently interfered with, corresponding to the area where the greatest malreduction was in 46.9% coronal and 42.4% of sagittal CT views.
ConclusionsSince the quality of reduction has prognostic value and is a necessary guide for the surgical team, that CT may be considered for the postoperative examination of the most challenging acetabular fracture cases.
Las placas intrapélvicas suprapectíneas juegan un importante papel en la osteosíntesis moderna de las fracturas del acetábulo. Sin embargo, la particular forma de estos implantes puede interferir con la valoración de la calidad de reducción utilizando radiografías simples (RX). En este trabajo, buscamos evaluar este artefacto y su relación con los hallazgos de la tomografía computarizada (TC).
Materiales y métodosEn una serie retrospectiva y unicéntrica de 22 fracturas acetabulares, las RX en proyecciones anteroposterior, alar y obturatriz; así como las imágenes de TC, fueron valoradas por 3 evaluadores independientes. Se utilizó el coeficiente Kappa de Cohen para analizar la concordancia entre observadores.
ResultadosLas placas suprapectíneas interfirieron con la valoración de la calidad de la reducción en la superficie de carga de un 75,3% de evaluaciones, y con las 3 proyecciones en un 43,9% de los casos. El segmento central fue el más consistentemente afectado, correspondiendo al área donde se observó el mayor desplazamiento residual en un 46,9% de cortes coronales y un 42,4% de cortes sagitales de TC.
ConclusionesDado que la calidad de la reducción tiene valor pronóstico y es una información necesaria para guiar el desempeño del equipo quirúrgico, debería valorarse complementar la RX con la TC en el examen postoperatorio de las fracturas acetabulares más complejas.
In recent years, we have seen a great expansion in the indications for fixation of acetabular fractures using anterior intrapelvic approaches, in particular the modified Rives–Stoppa approach. This is a less aggressive approach that allows better visualisation of the fracture, facilitates its reduction, and allows a more biomechanically competent fixation, with better radiological results and lower complication rates than the classic ilioinguinal approach.1–8 This expansion has been accompanied by the development of anatomical plates with quadrilateral lamina support, facilitating fixation of fractures with a medial vector. These patterns are particularly common in the elderly, where hip arthroplasty can be considered in a single procedure.1,2,9,10 Despite their advantages, the particular shape of intra-pelvic implants can interfere with post-operative assessment of the quality of reduction on plain radiographs (XR).11,12 This information is of great prognostic importance as it is related to both future joint function and native hip survival.13,14
The main aim of this study was to evaluate interference by intrapelvic suprapectineal plates on postoperative radiographs after fixation of acetabular fractures. We also evaluated this interference using postoperative computed tomography (CT) and compared the results of the two imaging tests. We hypothesised that suprapatellar plates would consistently interfere with postoperative assessment of acetabular reduction.
Material and methodThis is a retrospective case series (level of evidence IV) of patients undergoing surgery consecutively at a single public tertiary university hospital. The recruitment period was from March 2015 to December 2021. The research was approved by our Clinical Research Ethics Committee with reference number PR(ATR)369/2020. Drafting of the paper adhered to the standards of the PROCESS statement.15 We included all skeletally mature patients (age≥18 years) with acetabular fractures stabilised using an anatomical suprapectineal plate (PRO Pelvic and Acetabulum Plating System [Stryker, Kalamazoo, USA]) who underwent both XR and CT in the immediate postoperative period. Patients who had undergone sequential approaches were excluded to avoid potential interference from other implants in the radiological evaluations.
All patients were admitted through our emergency department and managed according to advanced trauma life support guidelines. Once stabilised, and depending on their clinical status, the patients were transferred to conventional wards or intensive care. In all cases, perioperative thromboprophylaxis and antibiotics were administered according to our hospital protocol. Acetabular surgery was scheduled as soon as sufficient stability was achieved. All osteosynthesis was performed using a modified Stoppa anterior intrapelvic approach, with or without the addition of a lateral window, according to the technique described in a previous publication.3 The patients were discharged when there was sufficient improvement in all clinical parameters.
X-ray and CT images obtained in the immediate postoperative period were analysed in each case. A 90° angle from the lateral edge of the acetabulum defined the weight-bearing dome (WBD) in the 3 radiographic projections: anteroposterior (AP), alar, and obturator. The WBD was divided into 3 segments equidistant by 30° (medial, central, and lateral) in each projection according to Nishii et al.16 The overlap of the plate on the acetabular joint line was recorded for each segment and in all projections. In order to focus on the artefact caused by the plate itself, any interference caused by the screws was ignored. A circumference centred on the centre of rotation of the hip and adapted to the subchondral bone was traced to measure both the residual step-off and gap in the WBD as described by Verbeek et al.17 (Fig. 1).
Post-operative XR of a 67-year-old male following fixation of an acetabular fracture using a suprapectineal plate. The 90° WBD is traced starting at the free edge of the acetabulum and is divided into 3 equidistant 30° segments (medial, central, and lateral). A circumference adapted to the articular surface is used as a guide to measure malreductions in gap and step-off. The overlap of the plate over the joint line is also recorded. (A) AP projection. No interference or malreduction. (B) Alar projection. Interference of the plate in the medial and central segments. There is no significant displacement of the WBD. (C) Obturator projection. Interference only in the medial segment. No residual displacement is observed. The quality of the reduction is considered anatomical, but 3 of the 9 segments are artefacted and cannot be correctly evaluated.
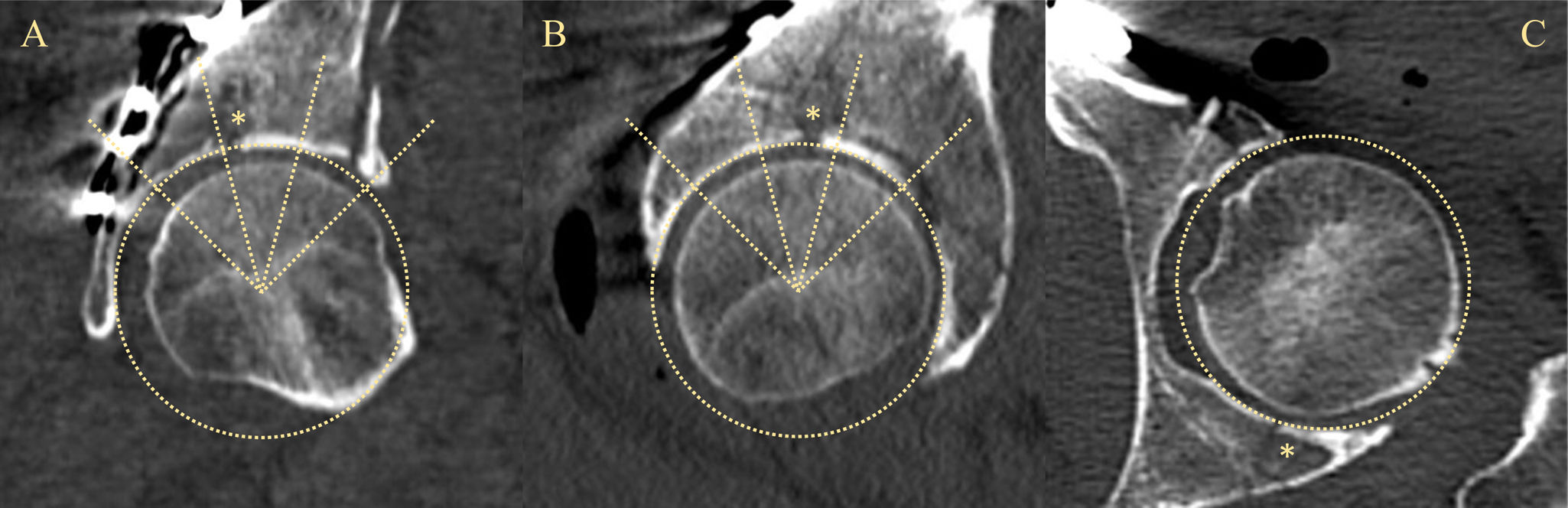
Axial, coronal, and sagittal CT views showing the largest diameter of the femoral head were evaluated. As on XR, the 90° WBD was defined from the lateral edge of the acetabulum on the coronal views. On the sagittal views, a 90° angle was defined centred on a vertical line through the centre of rotation of the hip. The coronal and sagittal WBDs were also divided into 3 segments: medial, central, and lateral for the coronal views and anterior, central, and posterior for the sagittal views.16 On the CT scan, a circumferential line was also drawn along the joint line to measure the gap and step-off (Fig. 2).17 Axial sections were used to determine whether the displacement involved the anterior or posterior wall.
Postoperative CT of the same 67-year-old male. As on the XR, the 90° WBD is defined and divided into 3 segments of 30°. On this occasion, the 90° angle faces the dome in a completely vertical direction to the plane of the examination. A circumference is also adapted to the articular surface, which is used as a guide to measure malreductions in gap and step-off. (A) Coronal section. Medial, central, and lateral segments. Main displacement in the central segment, with a space of 2.6mm. (B) Sagittal section. Anterior, central, and posterior segments. Space of 1.8mm, also in the central segment. (C) Axial section. Step-off of .7mm in the posterior wall. The * indicates the area of maximum residual displacement. The quality of the reduction is considered imperfect. All segments have been clearly evaluated.
Each image was evaluated by three independent observers, all residents in orthopaedic surgery and traumatology at our hospital (CLP, AFE, PMC). Matta's criteria were used to evaluate the reduction on both XR and CT, classifying their quality as: anatomical (0–1mm displacement), imperfect (2–3mm), and poor (>3mm).18
The Radiological Archive and Image Management (RAIM) programme (Corporació Sanitaria Parc Taulí, Sabadell, Spain) was used to evaluate the images. Clinical data were extracted from a database in SAP format (SAP SE, Walldorf, Germany). Both sets of data were entered into a Microsoft Excel database with coded identities. Stata/IC 14.2 software (StataCorp, College Station, USA) was used for statistical analysis.
Means and standard deviations (SD) were used to summarise continuous variables. Counts and percentages (%) were used for categorical variables. Cohen's kappa coefficient (κ) was used to assess inter-rater agreement for categorical variables, with inter-observer agreement categorised as none (κ=0–.20), low (κ=.21–.40), moderate (κ=.41–.60), substantial (κ=.61–.90), and near perfect (κ>.91). All p-values<.05 were considered statistically significant.
ResultsSample compositionDuring the study period, 47 intrapelvic suprapectineal plates were implanted in our hospital. There were no cases of bilateral acetabular fracture. Four patients with sequential approaches and 21 with incomplete radiological studies were excluded. Therefore, 22 patients with a mean age of 48.9 years (SD=15.4) were available for analysis. High energy mechanisms (n=18) and male patients (n=17) predominated. All fractures had a medial vector and involved both the anterior column and the quadrilateral lamina, with 11 elementary patterns (6 transverse and 5 anterior column fractures) and 11 associated patterns (6 anterior column and posterior hemitransverse, 4 type T, and 1 fracture of both columns). In 3 patients an associated instability of the posterior frame of the pelvic ring was noted, which in all cases was stabilised with iliosacral screws.
Interference according to radiological projectionIn 75.3% of the 198 radiographic evaluations (3 observers evaluating 3 projections [AP, alar, and obturator] in each of the 22 patients), the observers felt that the plate significantly interfered with the postoperative radiographic evaluation at some point of the WBD. In 29 (43.9%) of the 66 evaluations (3 observers and 22 patients), there was simultaneous interference in the 3 projections. The most commonly artefacted projections were the obturator and the alar, both of which showed plate overlap with a point on the WBD in 89.4% of evaluations. However, although the interobserver agreement for the presence of interference with the radiological evaluation was only low on the alar projection (κ=.36; p<.01), it was none for the obturator projection (κ=−.12; p=.83). On the AP projection, we found interference in 47% of the evaluations with moderate interobserver agreement (κ=.57; p<.01).
Interference by segment and relationship with the maximum residual displacementOn average, the plate was found to overlap one segment (SD=.4) in a total of 198 radiological evaluations. The average number of artefacted segments was .6 for the AP (SD=.5), 1.3 for the alar (SD=.5), and 1.1 for the obturator projection (SD=.4). For all radiological projections, the central segment of the WBD was the most consistently interfered, with low to moderate interobserver agreement for all projections (Table 1). The central segment was also the most common location of residual displacement on coronal CT views, accounting for 46.9% of CT assessments, followed by the medial (37.9%) and lateral (15.2%) segments. Unfortunately, interobserver agreement on the location of maximum displacement was poor for all segments on these views, probably related to the metallic artefact of the intra-pelvic implant, which mainly affected the coronal views. On the sagittal CT views, the greatest displacement was predominantly in the anterior and central segments (42.4% each), followed by the posterior segment (15.2%). Moderate to substantial interobserver agreement was observed for all segments (κ=.61, p<.01 for anterior; κ=.45, p<.01 central; κ=.50, p<.01 posterior).
Inter-observer agreement on the interference of the plate with assessment of the WBD for each segment and XR projection.
| WBD segment | |||
|---|---|---|---|
| Medial | Central | Lateral | |
| XR projection | |||
| AP | .42; <.01 | .43; <.01 | .06; .70 |
| Alar | .04; .37 | .52; <.01 | −.03; .60 |
| Obturator | −.03; .59 | .24; .03 | −.05; .65 |
Reported as Cohen's κ coefficient; p-value associated with κ.
Agreements between observers that are not significant or non-existent are shown in italics.
On average, the reduction assessed on XR was anatomical in 45.5%, imperfect in 9.1%, and poor in 45.5%. On the CT images, 63.6% of reductions were considered imperfect and 36.4% were considered poor. There was no significant agreement between observers for the reductions seen on XR and CT (κ=.11; p=.19) or between different observers evaluating the same test (κ=.19; p=.06 for XR; κ=.02; p=.42 for CT).
DiscussionThe interference caused by acetabular plates on postoperative radiology has already been mentioned by other authors, although without going into detail.1,2,19,20 Paradoxically, some have observed a better quality of reduction with CT than with XR, which they attribute precisely to the metallic artefacts that the implants can cause on the articular surface on XR.19 Although CT evaluations may also be affected for this reason, they appear to be less affected.11 In our study, we found that the peculiar silhouette of the suprapectineal plate interfered with assessment of the WBD on the majority of the postoperative radiographs (75.3%) and simultaneously affected the 3 projections in almost half of the cases. The central segment was the most consistently interfered with, which coincided with the greatest residual displacement on coronal and sagittal CT images. Although inconsistent, this would suggest that in many cases XR was unable to detect the most significant residual displacement of the WBD. The influence of joint gap and step-off on joint survival and functional outcome after acetabular osteosynthesis has been well documented.13,14 This implies that metallic artefacts caused by intra-pelvic implants may result in the loss of information of significant prognostic value.
CT has several advantages over radiography in the postoperative evaluation after fixation of acetabular fractures. Firstly, it has a higher sensitivity for detecting malreduction, which generally means finding a reduction of lower quality than that detected by XR, consistent with our results and those of other authors.11,19,21,22 It also allows better detection of implant malposition, which may influence the decision to re-operate.11,21,23 In addition, the residual displacement measured by CT relates better to the long-term prognosis of the hip, including its survival.17,19,21 All of this valuable information is necessary for the surgical team to perform correctly.
Despite its many advantages, the routine use of CT has several disadvantages. First, CT exposes the pelvic organs to higher doses of radiation, which may be of particular concern in patients with high-energy trauma who undergo multiple imaging studies and accumulate high doses of ionising radiation.11,23 CT scans are much more expensive than X-rays and are not readily available in all settings.11,17,22 There is also a risk of over-reliance on imaging for decision making, to the detriment of exploratory findings and other clinical aspects.17 For all these reasons, it is necessary to consider the rational use of these imaging tests.
The available literature shows that the quality of reduction is good to excellent in 82–92% of patients with acetabular fractures treated with modified Stoppa approaches.3,4,7,24,25 In our series, all patients had an imperfect or poor reduction on postoperative CT scans. However, we believe that these results were influenced by the composition of our sample, since only fractures with postoperative CT were included, which was probably requested in more complex cases. Interobserver agreement in assessing the quality of reduction appears to be better with CT than with XR.12,17 However, in our study we did not find agreement between our 3 observers when assessing the same tests or between individual observers when assessing both imaging modalities, which may be due to our limited sample size.
We acknowledge the limitations of this study, particularly its retrospective nature and small sample size. However, we believe that the description of a previously unstudied limitation of suprapectineal implants and the completeness of the radiological evaluations, which allowed an analysis of the interobserver agreement, add to the value of the present work.
In conclusion, anatomical intrapelvic suprapectineal plates play an important role in modern osteosynthesis of acetabular fractures. However, their unique configuration can make it difficult to assess the quality of reduction using XR. Since this information has important prognostic implications and is essential for the performance of the surgical team, we postulate that CT should be considered as a complement to radiography in the postoperative evaluation of the most complex acetabular fractures.
Level of evidenceLevel of evidence iv.
Authors’ contributionsPreparation of materials, data collection, and analysis were carried out by JVAP, CLP, ABM, and PMC. The first draft of the manuscript was prepared by JVAP and all authors commented on subsequent versions. All authors read and approved the final version of the manuscript.
Ethical considerationsThis study was approved by our Clinical Research Ethics Committee (CREC) with reference number PR(ATR)369/2020. This is a retrospective study. Its conduct did not involve any risk to the participants and all data collected were anonymised. Consequently, the CREC approved a full waiver of informed consent.
FundingNo outside funding was received for this study.
Conflict of interestsThe authors have declared conflicts of interest with Smith & Nephew, Zimmer-Biomet, Link Orthopaedics, Stryker, and MBA Surgical Empowerment.
Data availabilityThe data supporting the results of this study are available on request from the corresponding author, JVAP.