Some studies have proposed reducing unnecessary hospitalization days after total hip arthroplasty surgery to just a single overnight stay with discharge the morning after surgery. However, the available evidence on patient safety is of poor quality. The main objective was to analyze patient safety after discharge from the hospital the morning after total hip arthroplasty surgery (rapid discharge), comparing it with the standard 3-day postoperative stay.
Material and methodsA prospective, non-randomized comparative study was designed to compare two consecutive cohorts over time. The first cohort included patients with a postoperative stay of 3 days, while the second cohort had discharge the morning after surgery. The study evaluated the rate of complications and adverse events both postoperatively and after hospital discharge, as well as pain control using the visual analog scale, functional outcome using the Harris hip score, patient satisfaction, and economic cost.
ResultsThe rates of unexpected visits to the emergency room, early complications, readmissions, and reinterventions were similar in both groups, with no significant differences. The functional outcome was also similar in both groups, but the rapid discharge group experienced earlier recovery and significant financial savings.
ConclusionRapid discharge, the morning after surgery, is a safe, effective and efficient procedure for primary total hip arthroplasty in the majority of patients, with respect to a 3-day stay.
Algunos estudios han planteado la reducción de días de ingreso innecesarios tras la cirugía de la, disminuyendo la estancia a una sola pernoctación con alta en la mañana siguiente a la cirugía, pero las evidencias disponibles sobre la seguridad de los pacientes son de escasa calidad. El objetivo principal fue analizar la seguridad del paciente tras recibir el alta hospitalaria en la mañana siguiente a la cirugía de artroplastia total de cadera (alta rápida), comparándola con la estancia postoperatoria estándar de 3 días.
Material y métodosSe diseñó un estudio comparativo prospectivo, no aleatorizado, para comparar 2 cohortes consecutivas en el tiempo. La primera cohorte incluyó a pacientes con una estancia postoperatoria de 3 días; la segunda cohorte, con alta en la mañana siguiente de la cirugía. Se evaluaron la tasa de complicaciones y los eventos adversos postoperatorios y tras el alta hospitalaria, así como el control del dolor mediante escala visual analógica, el resultado funcional mediante la escala de cadera de Harris, la satisfacción del paciente y el coste económico.
ResultadosLas tasas de visitas inesperadas a urgencias, complicaciones precoces, reingresos y reintervenciones fueron similares en ambos grupos, sin diferencias significativas. El resultado funcional fue parejo en ambos grupos, pero con recuperación más precoz y ahorro económico importante en el grupo de alta rápida.
ConclusiónEl alta rápida, en la mañana siguiente a la cirugía, es un procedimiento seguro, efectivo y eficiente para la artroplastia total de cadera primaria en la mayoría de los pacientes, respecto a la estancia de 3 días.
Total hip arthroplasty (THA) is a major and aggressive surgery that entails risk for the patient. Several studies have shown that shortening the postoperative length of stay in individuals undergoing THA to 2–3 days lowered the rate of complications and readmissions, without increasing postoperative complications.1
Prosthetic hip surgery incurs a high healthcare expenditure, and mitigating these costs may be feasible by shortening the length of hospital stay.2–4 Some authors have found that minimising hospitalisation times also resulted in less early postoperative morbidity and mortality.4 More recently, others have demonstrated that an even shorter postoperative stay lasting a mere one or two days could prove advantageous, promoting a faster and more comfortable recovery for the patient.5,6
A number of studies2,5,7–9 have examined discharge outcomes within the first 24h following surgery, although all of them were retrospective in design. Hence, at the present time, there is a paucity of evidence of sufficient quality regarding the safety, effectiveness, and efficiency of primary THA surgery with only a single overnight stay for individuals who were not subject to a strict selection screening.
The hypothesis of this study was that discharge at 24h did not pose excess risk or adverse effects for the person undergoing primary THA surgery as compared to the standard 3-day stay. The objectives were to compare the safety of the procedure with 24h discharge with respect to the standard 3-day stay, in terms of complications and early postoperative readmissions, as well as to assess patient function and satisfaction.
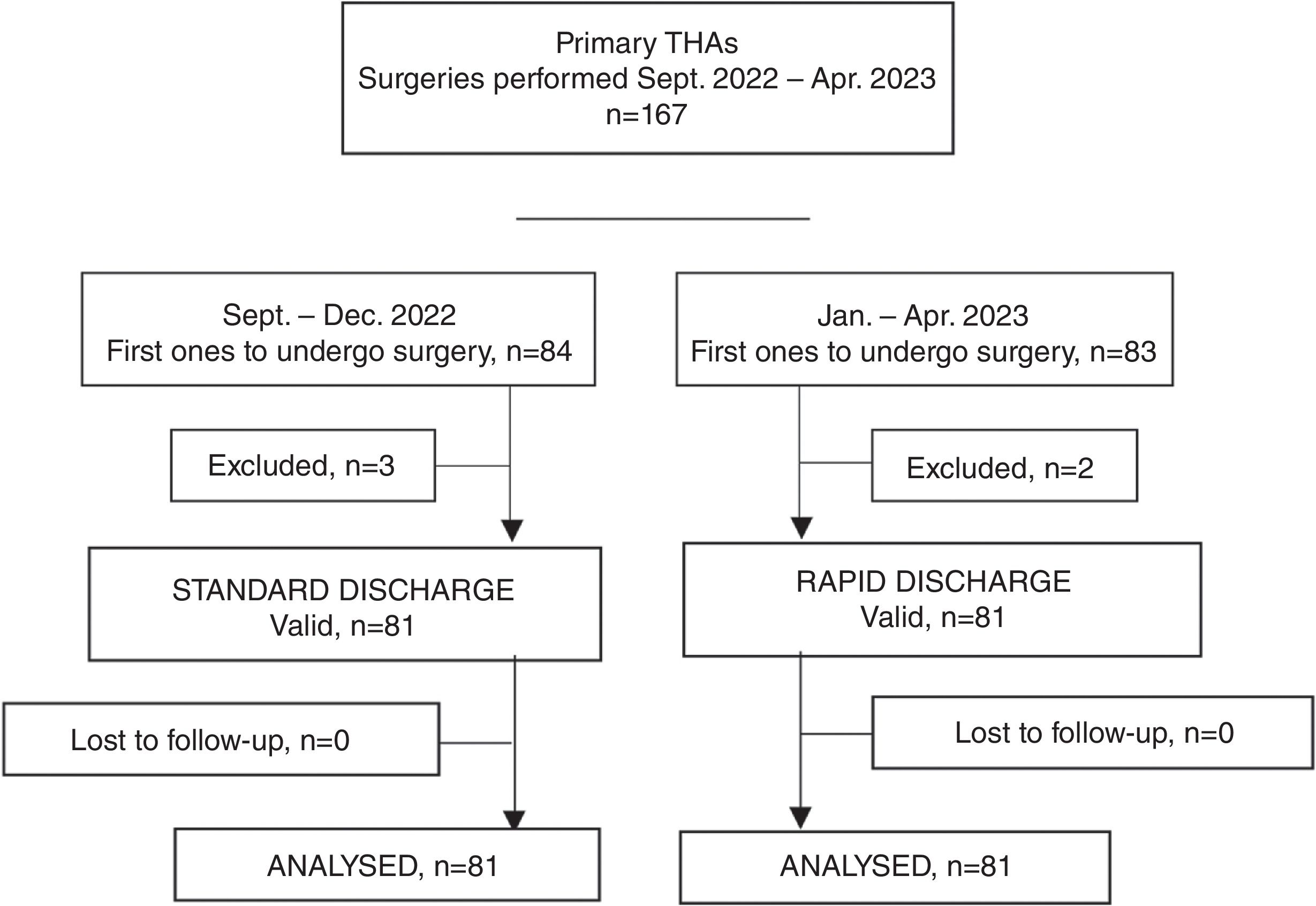
Material and methodsThe study population consisted of individuals undergoing THA surgery at a single centre between September 2022 and April 2023, with two sequential and consecutive study cohorts: (1) a cohort with a 3-day stay, who had the procedure between September and December 2022 (standard discharge group) and (2) another cohort that remained in the hospital for 24h, who had their operation between January and April 2023 (rapid discharge group).
A prospective, non-randomised study was designed for the purpose of comparative analysis of the outcomes. It was carried out in accordance with the ethical standards as recognised by the Declaration of Helsinki and resolution 8430 of 1993 and has the approval of the Institution's Ethics Review Board (PI2024-013); all of the participants granted their informed consent.
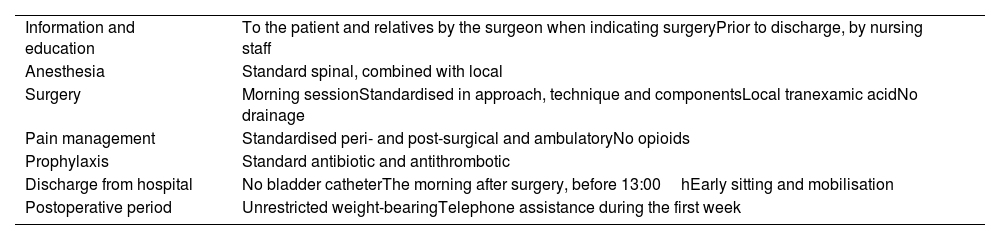
Table 1 presents the indispensable criteria in order to be authorised for rapid discharge.
Principles for rapid discharge.
| Information and education | To the patient and relatives by the surgeon when indicating surgeryPrior to discharge, by nursing staff |
| Anesthesia | Standard spinal, combined with local |
| Surgery | Morning sessionStandardised in approach, technique and componentsLocal tranexamic acidNo drainage |
| Pain management | Standardised peri- and post-surgical and ambulatoryNo opioids |
| Prophylaxis | Standard antibiotic and antithrombotic |
| Discharge from hospital | No bladder catheterThe morning after surgery, before 13:00hEarly sitting and mobilisation |
| Postoperative period | Unrestricted weight-bearingTelephone assistance during the first week |
The selection criteria were the same throughout the study and for all patients. The inclusion criteria consisted of individuals aged 18–85 years, implantation of a primary THA, sufficient cognitive ability to follow postoperative instructions, and family support at home. Patients were excluded if they were at high anaesthetic risk (ASA IV), morbidly obese, or living in an institution.
Surgical procedureAll the patients in both groups were admitted on the same day their surgery took place. The operations were performed in the morning by the same team of surgeons. Thirty minutes prior to the surgical incision, a regional block of the hip joint capsule was administered under ultrasound guidance and local anaesthesia (1% lidocaine and 0.25% bupivacaine), with spinal anaesthesia and sedation in all cases.
The direct anterior Smith–Petersen approach was the surgical approach adopted and the uncemented modular hip system (Bioimpianti, Milan, Italy) was implanted. In those participants older than 65 years, the acetabular insert was made of vitamin E-crosslinked polyethylene with a cobalt–chromium femoral head, while in younger patients, the ceramic–ceramic pair was implanted.
Before closing the capsule of the hip, intra-articular tranexamic acid was infused, without the use of aspiration drainage. Antibiotic prophylaxis with first-generation cephalosporin was administered 24h postoperatively, and antithrombotic prevention with oral rivaroxaban over the course of four weeks. Following the intervention, the patient was transferred to the post-anaesthesia recovery room for approximately one hour, and underwent pain and analytical monitoring on the hospital ward.
In the routine discharge group, all of the participants were allowed immediate sitting and ambulation from the first day following surgery, and were instructed to bear weight according to tolerance, with the use of a walking frame and under the supervision of a physical therapist.
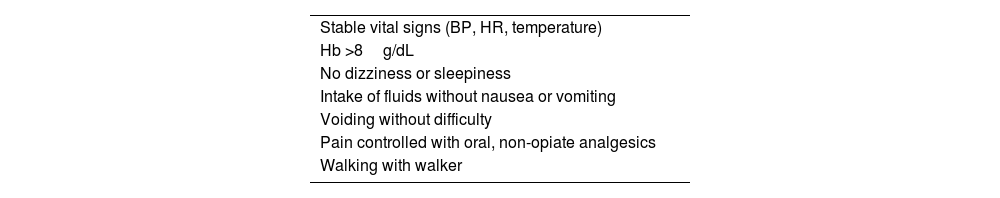
In the rapid discharge group, subjects were allowed to sit immediate and walking with the aid of a walker and the assistance of a physical therapist was permitted approximately 4–6h after being transferred to the ward. The morning after surgery, the surgeon assessed the individual for discharge from hospital. If they met the criteria for discharge (Table 2), a nurse reminded the patient as well as their relatives of what was involved in home care and warning signs. During the period between discharge and the first check-up appointment, they were had contact with nursing staff by telephone over the course of 24h to report any questions or incidents. The day after discharge, a nurse called them to check in on the condition of the surgical dressing and the need for analgesic medication.
Clinical criteria for hospital discharge.
| Stable vital signs (BP, HR, temperature) |
| Hb >8g/dL |
| No dizziness or sleepiness |
| Intake of fluids without nausea or vomiting |
| Voiding without difficulty |
| Pain controlled with oral, non-opiate analgesics |
| Walking with walker |
HR: heart rate; BP: blood pressure.
All of the participants in both groups underwent standardised clinical and radiological evaluation both preoperative assessments, as well as again at one, three, and six months after surgery. For the purposes of data analysis, the 1- and 6-month postoperative examinations were carried out by an independent surgeon, who had not been involved in the surgery with respect to the decision regarding discharge from the hospital.
The primary outcome variable was the safety of the procedure and was assessed by recording complications within 30 days of hospital discharge, readmission within 90 days of hospital discharge, and the need for surgical reintervention within 90 days of hospital discharge. Complications were recorded as per the principles outlined by Healy et al.10 Major complications could be medical (death, thrombosis, pulmonary embolism, cardiac crisis) and/or surgical (periprosthetic fracture, peripheral nerve injury, infection, instability), while minor complications were drainage from the surgical wound, anaemia requiring transfusion, surgical wound dehiscence, or urinary tract infection.
Secondary outcome variables were the rate of unexpected extended postoperative stay and the reason for it, emergency department visits rate in the first 30 days, pain assessment using a visual analogue scale from 0 (no pain at all) to 10 (the worst pain imaginable), functional outcome according to the Harris hip scale, as well as patient satisfaction with the discharge procedure using a 5-category Likert-type scale: very satisfied, satisfied, indifferent, dissatisfied, dissatisfied, very dissatisfied. Results were analysed by grouping the responses into satisfied (very satisfied and satisfied) and dissatisfied (the other three responses).
The economic cost of each procedure was also examined. The costs associated with admission, preoperative assessment, operating theatre, surgery, prosthetic material, and recovery room are similar regardless of the length of hospitalisation. The only factor that could be modified in terms of the final cost is the length of stay. At our centre, the average daily cost of hospital stay is 250€, regardless of whether or not it is a full 24h stay; in addition to this, the average cost for standard pain medication and treatment materials is 50€.
Statistical analysisThe minimum required sample size was calculated on the basis of the primary endpoint of the rate of major postoperative complications requiring that the patient be readmitted. A prospective, European, multicentre study reported a rate of 4% among individuals who had a standard 3-day short stay.11 In light of this finding, a non-inferiority test was proposed for the rapid discharge group after only one night, such that the rate in this group would be at least similar to, and not higher than, that outlined for the routine short stay lasting three days. Assuming a statistical significance of p<0.05 and an 80% statistical power, 154 patients were required; i.e., 77 in each group. Allowing for a possible loss to follow-up of 5% of the participants to be included, a sample of 162 patients was estimated: 81 in each arm.
Statistical analyses were performed using the SPSS® v. 21 software (SPSS Inc., Chicago, USA). The normal or non-parametric distribution of the variables was evaluated using the Kolmogorov–Smirnov test. Intergroup comparison of qualitative variables was carried out with the chi-square test or Fisher's exact test. The means of independent samples were compared by means of the Student's t-test or the non-parametric Mann–Whitney test, whereas the paired samples were compared using the paired Student's t-test or the non-parametric Wilcoxon signed-rank test. For all tests, statistical significance was considered at p<0.05.
ResultsOver the course of the entire study period, 167 patients with primary THA underwent surgery, from which the aim was to recruit the first 81 patients in each period who met the criteria. During the first period, between September and December 2022, which constituted the routine discharge group, three patients of the first 84 patients who underwent surgery were excluded, two because they were over the age of 85 years and one because he had suffered a myocardial infarction six months prior to the arthroplasty. Eighty-one patients were still valid for the study, with no loss to follow-up until the end of the study. During the second period, between January and April 2023, from which the rapid discharge group was recruited, of the first 83 subjects undergoing THA, two were excluded: one because they resided in a nursing home and the other due to being older than 85 years of age. Eighty-one patients remained valid for the study, with no loss to follow-up until the end of the study (Fig. 1).
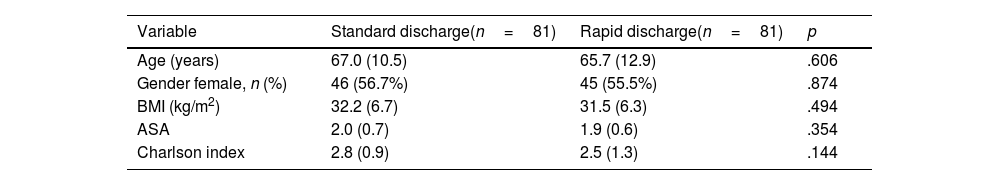
The baseline characteristics of both groups can be found in Table 3.
Patients’ baseline characteristics.
| Variable | Standard discharge(n=81) | Rapid discharge(n=81) | p |
|---|---|---|---|
| Age (years) | 67.0 (10.5) | 65.7 (12.9) | .606 |
| Gender female, n (%) | 46 (56.7%) | 45 (55.5%) | .874 |
| BMI (kg/m2) | 32.2 (6.7) | 31.5 (6.3) | .494 |
| ASA | 2.0 (0.7) | 1.9 (0.6) | .354 |
| Charlson index | 2.8 (0.9) | 2.5 (1.3) | .144 |
Data regarding continuous variables are expressed as the mean (standard deviation).
ASA: American Society of Anaesthesiologists; BMI: body mass index.
With respect to the primary outcome variable, there were no post-discharge complications in the first 30 days, no readmissions, and no secondary surgeries during the first 90 days in either study group.
The mean length of stay for the sample in the standard discharge group was 3.1 days (SD 0.6; range 3–8) and 1.1 days (SD 0.5; range 1–6) in the rapid discharge group (p=0.000). The hospital stay was as planned in 74 patients (91.2%) in the standard discharge group. As for the remaining seven patients, the postoperative stay had to be unexpectedly prolonged beyond the planned three days, with a total increased stay of 11 days. In the rapid discharge arm, the hospital stay proceeded as planned in the case of 77 participants (95.0%). In the remaining four patients, the post-surgical stay was prolonged unexpectedly beyond the pre-arranged 24h, leading to a total increase of 8 days.
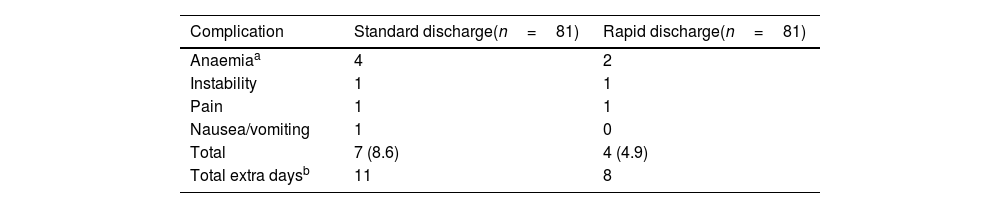
During their hospitalisation, seven individuals pertaining to the standard discharge group and four in the rapid discharge group (p=0.534) developed complications that prompted a delay in discharge (Table 4). In the routine discharge arm, there was one case of prosthetic instability that made closed reduction necessary, and, consequently, the persons’ stay was prolonged for an additional five days. Four participants exhibited postoperative anaemia and required allogeneic blood transfusion, thereby increasing the stay by an additional day, while two patients also required an additional day due to pain and nausea with vomiting, respectively. Similarly, in the rapid discharge group, there was also one case of prosthetic instability that was resolved by closed reduction, extending the person's stay for an additional five days. Two individuals with postoperative anaemia required allogeneic blood transfusion, prolonging their stay by one day, and another patient had poorly controlled pain, which resulted in an extra day of hospitalisation over the planned length of stay.
Complications in the immediate postoperative period, during hospital stay.
| Complication | Standard discharge(n=81) | Rapid discharge(n=81) |
|---|---|---|
| Anaemiaa | 4 | 2 |
| Instability | 1 | 1 |
| Pain | 1 | 1 |
| Nausea/vomiting | 1 | 0 |
| Total | 7 (8.6) | 4 (4.9) |
| Total extra daysb | 11 | 8 |
Data expressed as cases (n). Total expressed as n (%).
No further episodes of instability were documented in patients that required reduction, nor were there any intraoperative complications, infections, or periprosthetic fractures during the study period.
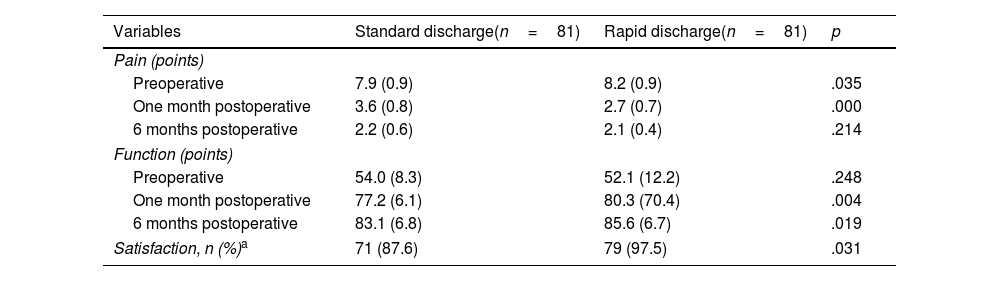
Postoperative pain was significantly higher among the population included is the routine discharge group at the one-month post-surgical period, albeit not at the six-month follow-up period. Furthermore, according to the postoperative functional assessment, there were significant intergroup differences at the one- and six-month follow-up visit. Satisfaction with the procedure was significantly greater among those participants included in the rapid discharge group (Table 5).
Results for secondary variables.
| Variables | Standard discharge(n=81) | Rapid discharge(n=81) | p |
|---|---|---|---|
| Pain (points) | |||
| Preoperative | 7.9 (0.9) | 8.2 (0.9) | .035 |
| One month postoperative | 3.6 (0.8) | 2.7 (0.7) | .000 |
| 6 months postoperative | 2.2 (0.6) | 2.1 (0.4) | .214 |
| Function (points) | |||
| Preoperative | 54.0 (8.3) | 52.1 (12.2) | .248 |
| One month postoperative | 77.2 (6.1) | 80.3 (70.4) | .004 |
| 6 months postoperative | 83.1 (6.8) | 85.6 (6.7) | .019 |
| Satisfaction, n (%)a | 71 (87.6) | 79 (97.5) | .031 |
Data for continuous variables given as mean (standard deviation).
In the rapid discharge group, two different individuals consulted by telephone during the first week to have their analgesia adjusted. No one presented to the emergency department in the first 30 days.
The difference in length of stay between the standard and the rapid discharge was two days following surgery. As a result, this accounts for a per procedure price difference of 600€. With a study population of 81 patients in each group, the cost of hospitalisation was 76,200€ for the routine discharge group (300€×254 stays) and 26,700€ for the rapid discharge group (300€×89 stays); this translates into a 49,500€ difference between both procedures.
DiscussionThe most important finding to come out of this study was that discharge 24h post THA was more effective and efficient, and no less safe, than discharge three days after surgery. Ninety-five percent of subjects completed the 1-day admission as scheduled, as opposed to 91.3% in the 3-day group; nonetheless it failed to achieve statistical significance.
Scientific evidence has proven that the reduction of the length of hospital stay among individuals undergoing THA also resulted in fewer complications, fewer readmissions, and less rehabilitation time was required for the patient to restore walking, without causing an increase in postoperative complications, as well as greater patient satisfaction.12,13 Some authors have recommended that an overnight stay with discharge the morning after surgery should be preferred over outpatient surgery,2,7,8 given that most postoperative complications or problems arise within the first 24h.1,5
This study evinces that discharge the morning after surgery is a safe procedure for primary THA patients, inasmuch as the early complication rate is similar to the standard 3-day postoperative stay. Moreover, we also noted that there were no ED visits and no complications, readmissions, or reinterventions following discharge.
At the 4-week postoperative follow-up visit, those participants who had pertained to the rapid discharge arm had significantly less pain and better function than those who had been discharged after the standard three days. At six months, statistically significantly more subjects were satisfied and had a better functional outcome after the rapid discharge procedure, although there were no statistically significant intergroup differences with respect to pain as quantified using a visual analogue scale. The higher percentage of satisfied patients could possibly be due to the fact that they felt safe at home, with adequate pain control, and in a more comfortable and familiar environment.
There is a dearth of studies involving patients undergoing THA with a single day's hospital stay. In the only prospective study available14 analysed a series of 378 patients undergoing primary THA surgery, and found that the mean postoperative length of hospitalisation was 26h, with a 6% complication rate during the three months post-discharge, and a 2% rate for both readmission and reintervention. These rates are higher than those found in the present study, though it must be mentioned that den Eeden et al. included both primary and revision surgeries.14 In another retrospective study with discharge the day after surgery, the authors concluded that the overnight stay was an unnecessary cost, as most patients did not receive direct medical care. That being said, however, during this short stay, 66% of the patients required fluid therapy for hypotension or bladder catheterisation for urinary retention.15 In a review of a series of 7466 consecutive patients undergoing primary hip and knee arthroplasty, shortening the postoperative length of stay from two to only one day was not associated with an increase int the risk of ED visits or readmissions within the first three months of hospital discharge, with pain being the main cause for both; individuals with more co-morbidities were more likely to undergo reoperation versus those without co-morbidities.16
Another two studies compared patients discharged the day after surgery and those who were discharged 2– days following surgery.17,18 Kiskaddon et al.17 conducted a retrospective, comparative study and detected similar rates of visits to the emergency department, readmissions within 30 days after surgery and reinterventions within 90 days post-discharge. The authors therefore concluded that next-day discharge was as feasible and safe a procedure as a longer stay. In a retrospective, observational study of 124,150 people who underwent THA surgery and were identified in a US national database, Mundi et al.18 compared those who were discharged on the same day as surgery, the next day, or 2–3 days following intervention. In the latter two groups, the risk of readmission or reintervention was lower among those subjects who were discharged the following day and the risk of readmission was significantly lower among patients discharged the following day compared to those who were discharged the same day.
Head to-head studies between outpatient surgery and surgery involving a longer postoperative stay report that outpatient surgery does not increase postoperative complications.19,20 Nonetheless, studies on outpatient surgery tend to include highly selected patients who are younger, have fewer co-morbidities, and lower BMI versus those released after a longer stay.2,21,22 This leads to a lower likelihood of postoperative complications than in individuals seen in routine practice.1,23 Furthermore, a significant percentage of these patients could not be discharged on the same day as their surgery, and remained in hospital for at least one night24; many stated that they preferred to be discharged after having spent at least one night in hospital following surgery, and that they felt safer doing so.25,26
We believe that the strengths of the present study were that the data were collected prospectively; patient selection was not overly restrictive and in line with standard practice, and that the same surgeon performed the surgeries following the same methodology. The most important limitations were a postoperative follow-up time of only six months, despite the fact that the aim was to examine the safety of early discharge from hospital and its possible impact on acute complications, readmissions, and secondary surgeries in the first few months following surgery. Mechanical and septic complications are generally unrelated to the length of hospitalisation. The distribution was sequential and non-randomised, decreasing the level of evidence, although the absence of significant differences in the study population's baseline characteristics between the two groups studied minimised selection bias. The analysis of economic costs did not use exact data, determined by DRG process code with complexity modifiers by procedure and patient, making for a less precise comparative analysis of this variable.
ConclusionIn this study, rapid discharge the morning following primary THA surgery has proven to be more effective, more efficient, and entail a higher degree of patient satisfaction compared to a 3-day stay; likewise, it is not inferior in terms of the safety of the procedure.
Level of evidenceLevel of evidence II.
FundingThis research has not received any specific grant of any kind from any public or private funding institution or from the non-profit sectors.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to thank Prof. Alejandro Lizaur Utrilla for his advice in the design of the study and interpretation of the data.