Scoliosis in pediatric patients encompasses a highly heterogeneous group and is one of the most common reasons for consultation, with a prevalence ranging between 1.5% and 3% of the pediatric population. The most common categories of pediatric scoliosis include idiopathic, neuromuscular, and congenital forms. Surgical correction of spinal deformities is a complex procedure, and although major complications are rare, it remains a crucial intervention. The main goal of surgical treatment is to prevent deformity progression while minimizing morbidity, maximizing postoperative function, and improving the patient's quality of life. This study aims to evaluate complication rates associated with surgical treatment of pediatric scoliosis and analyze the variables linked to increased complication rates over a 30-year period.
MethodsThis study involved a retrospective review of prospectively collected data from a single institution's registry of patients who underwent surgical treatment for pediatric scoliosis over a 30-year period.
ResultsBetween 1991 and 2021, 779 patients underwent surgery. A total of 63 complications (8.08%) were recorded. Neuromuscular scoliosis had the highest complication rate, with 34 complications in 186 patients (18.28%), followed by congenital scoliosis with 6 complications in 57 patients (10.53%), and 23 complications in 536 patients with adolescent idiopathic scoliosis (4.29%). Infections were the most frequent complications at 4.49%. Neuromuscular scoliosis had the highest infection rate at 10.75%, followed by congenital scoliosis at 5.26%, and idiopathic scoliosis at 2.24%. Neurological deficit rates varied significantly according to the etiology of scoliosis (p<.001), with the highest rate in neuromuscular cases (2.69%), followed by congenital cases (1.75%), and idiopathic scoliosis (0.93%). Neuromuscular and congenital scoliosis had the highest rates of clinical complications, at 3.76% and 1.75%, respectively, followed by idiopathic scoliosis (1.12%).
ConclusionAn overall complication rate of 8.09% was observed in our series following surgery for pediatric scoliosis. Although neuromuscular scoliosis presented the highest morbidity, relatively high complication rates were observed across all groups. This information can be valuable for preoperative counseling and surgical decision-making in the treatment of pediatric scoliosis.
La escoliosis en los pacientes pediátricos abarca un grupo altamente heterogéneo, siendo una de las razones más comunes de consulta, con una prevalencia que oscila entre el 1,5 y el 3% de la población pediátrica. Las categorías más comunes de escoliosis pediátrica incluyen las formas idiopáticas, neuromusculares y congénitas. La corrección quirúrgica de las deformidades espinales es un procedimiento complejo y, aunque las complicaciones mayores son raras, sigue siendo una intervención crucial. El objetivo principal del tratamiento quirúrgico es prevenir la progresión de la deformidad al tiempo que se minimiza la morbilidad, se maximiza la función postoperatoria y se mejora la calidad de vida del paciente. Este estudio tiene como objetivo evaluar las tasas de complicaciones asociadas con el tratamiento quirúrgico de la escoliosis pediátrica y analizar las variables vinculadas con el aumento de las tasas de complicaciones a lo largo de un período de 30 años.
MétodosEste estudio implicó una revisión retrospectiva de datos recopilados prospectivamente del registro de una sola institución sobre los pacientes que se sometieron a tratamiento quirúrgico para la escoliosis pediátrica durante un período de 30 años.
ResultadosEntre 1991 y 2021, 779 pacientes fueron tratados mediante cirugía. Se registraron un total de 63 complicaciones (8,08%). La escoliosis neuromuscular presentó la tasa más alta de complicaciones, con 34 complicaciones en 186 pacientes (18,28%), seguida de la escoliosis congénita con 6 complicaciones en 57 pacientes (10,53%), y 23 complicaciones en 536 pacientes con escoliosis idiopática del adolescente (4,29%). Las infecciones fueron las complicaciones más frecuentes con un 4,49%. La escoliosis neuromuscular tuvo la tasa más alta de infecciones con un 10,75%, seguida de la escoliosis congénita con un 5,26%, y la escoliosis idiopática con un 2,24%. Las tasas de déficit neurológico variaron significativamente según la etiología de la escoliosis (p<0,001), siendo la tasa más alta en los casos neuromusculares (2,69%), seguida de los casos congénitos (1,75%) y la escoliosis idiopática (0,93%). La escoliosis neuromuscular y la escoliosis congénita tuvieron las tasas más altas de complicaciones clínicas, con un 3,76 y un 1,75, respectivamente, seguidas de la escoliosis idiopática (1,12%).
ConclusiónSe observó una tasa general de complicaciones del 8,09% en nuestra serie después de la cirugía para la escoliosis pediátrica. Aunque la escoliosis neuromuscular presentó la mayor morbilidad, se observaron tasas relativamente altas de complicaciones en todos los grupos. Esta información puede ser valiosa para el asesoramiento preoperatorio y la toma de decisiones quirúrgicas en el tratamiento de la escoliosis pediátrica.
Paediatric spinal deformity, with scoliosis being the most common manifestation, is a diverse group of conditions that affect the quality of life of children and adolescents.1 Paediatric scoliosis is one of the most common reasons for consultation with paediatric orthopaedic surgeons. It is estimated to affect between 1.5% and 3% of the paediatric population. Historically, scoliosis has been defined as a spinal deformity in the coronal plane of more than 10°, but it encompasses a set of more complex three-dimensional deformities.1,2 Idiopathic scoliosis is the most prevalent form, followed by neuromuscular scoliosis, congenital scoliosis, and other syndromes.3–5 The natural history of scoliosis is highly variable depending on its aetiology. Generally, neuromuscular scoliosis and congenital scoliosis are more likely to progress and eventually require surgery than adolescent idiopathic scoliosis. Spinal deformity may progress during periods of skeletal growth and even after skeletal maturity.6 Indications for surgical correction of scoliosis include neurological deficit, curve progression, pain, cardiopulmonary compromise, aesthetics, and severe scoliosis (defined as any spinal deformity with a Cobb angle greater than 45°). The main objective of surgery is to safely correct the spinal deformity and prevent its future progression by achieving a solid spinal fusion, while minimising or avoiding complications.
Surgical correction is associated with risks, adverse events, and complications.7 The incidence of complications varies depending on the underlying aetiology of the spinal deformity and the specific surgical procedure.8,9 The overall incidence of complications associated with surgical correction in patients with adolescent idiopathic scoliosis has been reported to range from 5% to 23%. For neuromuscular scoliosis, the incidence is 35%, and for congenital scoliosis it is 14%.10,11 It is important to understand the true incidence and causes of complications after spinal surgery for shared decision-making between the surgeon, patients, and their families.
This study aimed to evaluate the complication rates associated with the surgical treatment of paediatric scoliosis, and to examine how the type of scoliosis influences the occurrence of complications over a 30-year period in patients operated on by the same medical team in a single hospital. By gathering information through this study, we aim to improve preoperative planning, provide patients and their parents with advice about possible complications, and highlight relevant preventive measures. Our ultimate goal is to help patients with spinal deformities achieve the best possible quality of life.
Material and methodsThe information was extracted from a database containing prospectively collected patient data. Established at the hospital in 1991, this registry includes paediatric patients diagnosed with spinal deformities who were treated with spinal fusion surgery due to severe scoliosis.
This study is a retrospective cohort with prospectively collected data, covering all patients treated with surgery for scoliosis between 1991 and 2021. Patients under the age of 21 with a primary diagnosis of severe scoliosis who underwent either posterior spinal fusion or anterior spinal fusion, and had undergone at least 2 years of follow-up, were included in the study. Deformities caused by cancer, infection, or sequelae of trauma were excluded.
The collected variables included demographic data (gender and age at the time of surgery), follow-up time, preoperative diagnosis and complications, and their treatment. Patients were classified according to their diagnosis: adolescent idiopathic scoliosis (AIS), neuromuscular scoliosis (NS), or congenital scoliosis (CS).
Operative and perioperative complications, defined as those occurring within 90 days of surgery, were recorded. The occurrence of fatal and non-fatal complications, new neurological lesions and infections was assessed. For new neurological deficits, the type (nerve root, cauda equina, or partial/complete spinal cord) and degree of improvement (none, partial or complete) were analysed. For infections, the type, bacteria, duration of treatment, and outcome were recorded, with data only recorded for infections occurring within the first 90 days after surgery.
Other complications were also evaluated, including spinal implant failure (defined as any alteration to the stability of the fixation system, such as breakage of the implant, loosening of the screws, or detachment of the anchors), medical complications and others. All complications occurring within the first 90 days after surgery were included. The treatment of these complications was also detailed, including whether further surgery was required, how long it was between the primary surgery and the complication occurring, and whether the complication was completely or partially resolved.
All surgeries were performed by the same surgical team and information was collected retrospectively from electronic medical records by two researchers (PD and MRL).
Statistical analysisDescriptive statisticsQuantitative variables are presented as the mean and standard deviation, or the median and interquartile range, depending on the observed distribution. Categorical variables are presented as proportions, and 95% confidence intervals calculated for each estimator. Pearson's χ2 test is used to compare the distributions of the categorical variables.
ResultsA total of 779 cases met the inclusion criteria. These cases were classified into three main subtypes: idiopathic scoliosis, congenital scoliosis, and neuromuscular scoliosis. Of these, 536 (68.8%) were diagnosed with idiopathic scoliosis, while 186 (23.8%) were diagnosed with neuromuscular scoliosis. Within the neuromuscular cases, those related to cerebral palsy (72/186, 38.7%), myelodysplasia (50/186, 26.8%), and other causes (64/186, 34.4%) were distinguished. Additionally, 57 patients (7.3%) with congenital scoliosis were recorded.
Spinal fixation was performed using pedicle screws in all patients. No anterior releases or osteotomies were performed to increase flexibility for any of the deformities. For patients with thoracic lordosis and the most severe curves, posterior releases of the interspinous and yellow ligaments were performed at the apex of the deformity.
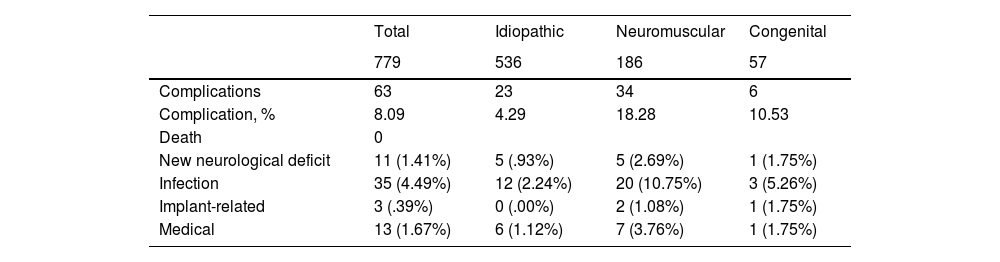
A total of 63 complications (8.08%) were reported and are detailed in Table 1 according to the type of scoliosis. The total complication rates varied significantly among the three most common types of scoliosis (idiopathic, congenital, and neuromuscular), with a p-value <.001. The highest overall complication rate was seen in patients with neuromuscular scoliosis (34/186 or 23.8%), followed by those with congenital scoliosis (6/57 or 10.5%) and idiopathic scoliosis (23/536 or 4.2%).
Detailing all complications found with their percentage for each type of scoliosis.
| Total | Idiopathic | Neuromuscular | Congenital | |
|---|---|---|---|---|
| 779 | 536 | 186 | 57 | |
| Complications | 63 | 23 | 34 | 6 |
| Complication, % | 8.09 | 4.29 | 18.28 | 10.53 |
| Death | 0 | |||
| New neurological deficit | 11 (1.41%) | 5 (.93%) | 5 (2.69%) | 1 (1.75%) |
| Infection | 35 (4.49%) | 12 (2.24%) | 20 (10.75%) | 3 (5.26%) |
| Implant-related | 3 (.39%) | 0 (.00%) | 2 (1.08%) | 1 (1.75%) |
| Medical | 13 (1.67%) | 6 (1.12%) | 7 (3.76%) | 1 (1.75%) |
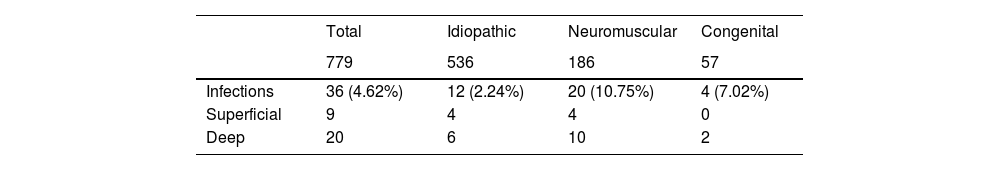
The most common complication was infection, with an incidence rate of 4.4%. The highest infection rate was found in patients with neuromuscular scoliosis, at 10.7%, followed by patients with congenital scoliosis at 5.2%, and patients with idiopathic scoliosis at 2.2%. Within the neuromuscular scoliosis subgroup, patients with myelomeningocele had the highest infection rate at 26% (13/50), followed by patients with cerebral palsy at 7% (5/72), and 3.1% (2/64) in the remaining neuromuscular scoliosis patients, as shown in Table 2. The most frequently cultured bacterial organisms were all Gram-negative, with species such as Escherichia coli, Pseudomonas aeruginosa, and Enterococcus standing out.
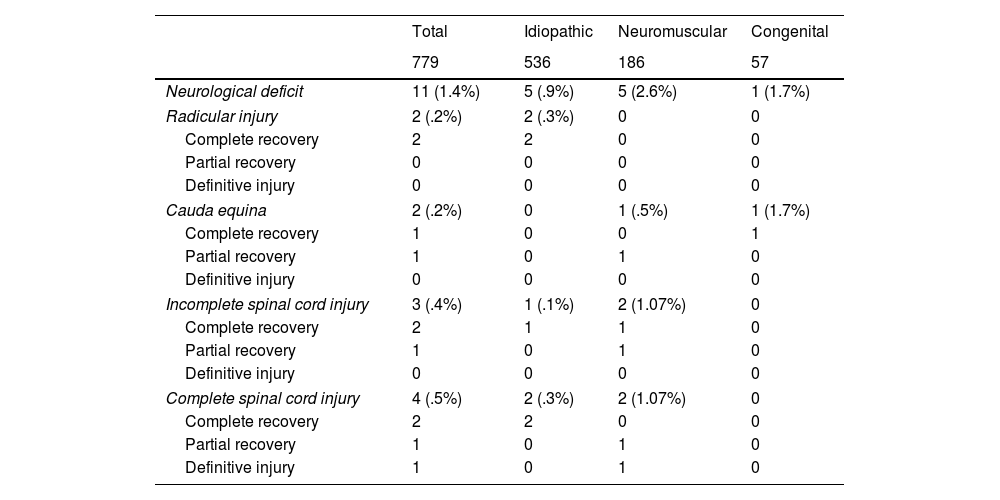
Neurological complications occurred in 11 cases (1.41%), as detailed in Table 3. The incidence of neurological deficits varied significantly according to the aetiology of the scoliosis (p<.001): the highest rate was observed in cases of neuromuscular scoliosis (2.69%), followed by congenital cases (1.75%), then idiopathic scoliosis (.93%). The most common neurological deficits were complete spinal cord injury (4/779 or .5%) and incomplete spinal cord injury (3/779 or .4%), while radicular injury (2/779, or .2%) and cauda equina (2/779, or .2%) were also recorded (Table 3). Complete recovery was observed in cases of nerve root deficit (55/83 or 66%). In the other patients with neurological deficits, recovery varied according to the type of scoliosis. Complete recovery was recorded in cases of idiopathic scoliosis (5/536 or .93%), and the case of incomplete spinal cord injury (1/536 or .1%) occurred within 3 months postoperatively. Patients with complete spinal cord injuries (2/536 or .3%) achieved complete recovery at 6 months. Only one patient with congenital scoliosis (1/57 or 1.75%) had a neurological complication, specifically a cauda equina deficit, which recovered completely within 2 months of surgery. Patients with neuromuscular scoliosis experienced the highest incidence of neurological complications at 2.69% (5/186). Of these patients, only one with cauda equina achieved complete recovery. There was one patient with cauda equina syndrome, another with partial spinal cord injury, and one more with complete spinal cord injury who experienced partial recovery. However, of those with complete spinal cord injury, only one showed no improvement in their condition (Table 3).
Description of neurological complications and outcomes.
| Total | Idiopathic | Neuromuscular | Congenital | |
|---|---|---|---|---|
| 779 | 536 | 186 | 57 | |
| Neurological deficit | 11 (1.4%) | 5 (.9%) | 5 (2.6%) | 1 (1.7%) |
| Radicular injury | 2 (.2%) | 2 (.3%) | 0 | 0 |
| Complete recovery | 2 | 2 | 0 | 0 |
| Partial recovery | 0 | 0 | 0 | 0 |
| Definitive injury | 0 | 0 | 0 | 0 |
| Cauda equina | 2 (.2%) | 0 | 1 (.5%) | 1 (1.7%) |
| Complete recovery | 1 | 0 | 0 | 1 |
| Partial recovery | 1 | 0 | 1 | 0 |
| Definitive injury | 0 | 0 | 0 | 0 |
| Incomplete spinal cord injury | 3 (.4%) | 1 (.1%) | 2 (1.07%) | 0 |
| Complete recovery | 2 | 1 | 1 | 0 |
| Partial recovery | 1 | 0 | 1 | 0 |
| Definitive injury | 0 | 0 | 0 | 0 |
| Complete spinal cord injury | 4 (.5%) | 2 (.3%) | 2 (1.07%) | 0 |
| Complete recovery | 2 | 2 | 0 | 0 |
| Partial recovery | 1 | 0 | 1 | 0 |
| Definitive injury | 1 | 0 | 1 | 0 |
Differences in the incidence of other complications were observed between scoliosis subtypes. Neuromuscular and congenital scoliosis had the highest rates of clinical complications at 3.76% (7/186) and 1.75% (1/57), respectively, followed by idiopathic scoliosis at 1.12% (6/536). The most frequent clinical complication in the case of neuromuscular scoliosis was respiratory-related, with two cases of respiratory failure requiring prolonged respiratory support and tracheostomy. A further two cases of urinary tract infection and three cases of ventriculoperitoneal shunt failure were observed. Conversely, the most common clinical complication in idiopathic scoliosis was superior mesenteric artery syndrome, with three cases reported. There were also two cases of clinical decompensation and one case of acute pulmonary oedema. In the case of congenital scoliosis, one case of malignant hyperthermia was reported.
DiscussionSpinal deformities are a common reason for consultation in the paediatric population, with scoliosis being the most common type. The most common type of spinal deformity is adolescent idiopathic scoliosis (AIS) (2). Less frequently than AIS, there are also neuromuscular and congenital scoliosis.12 Treatment varies depending on the type of scoliosis, the age of the patient, the extent of the spinal deformity, and the remaining growth potential. When surgery is chosen, posterior spinal fusion is the preferred method for correcting spinal deformity. The main goals of surgical treatment are to prevent the progression of scoliosis, restore coronal and sagittal balance, reduce pain, and improve respiratory and cardiac capacity, and achieve solid spinal fusion while minimising or avoiding complications.
This paper critically evaluates the results obtained, their clinical relevance, and their implications for medical practice. Immediate and postoperative complications in paediatric scoliosis were evaluated over a 30-year period in a single hospital by the same medical team. This gives us a unique, detailed view of complication rates and enables us to make a more thorough assessment of the risks involved in operating on children and adolescents with scoliosis.
In our current series of idiopathic scoliosis surgeries, the overall complication rate was 4.2%, with a mortality rate of 0%. The most frequently observed complication was infection. These results are comparable to those reported by Coe et al.,13 in a study of 6332 cases of AIS recorded between 2001 and 2003. In this study, the respective rates were 5.2% and .03%. Reames et al. report a complication rate of 6.3% and a mortality rate of .02%, based on 19,360 cases obtained from the Scoliosis Research Society (SRS) morbidity and mortality database.11 Kwan et al.14 published a more extensive study of 84,320 AIS patients, evaluating complications after spinal surgery. They found complication and mortality rates of 1.5% and .001%, respectively. Hariharan et al. conducted a prospective study of complications in AIS patients over 10 years, reporting a complication rate of 9.9%, with infection being the most frequent complication.15
The overall complication rate for surgery on congenital scoliosis in this series was 10.5%, with a mortality rate of 0%. In the case review presented by Reames et al., the incidence of complications in this patient group was 10.6%, with a mortality rate of .3%. The most common complication was neurological deficit. There are few published studies available for comparison; Reames et al. reported the largest series of cases. It is important to note that no deaths were reported in previous studies, probably due to the small number of patients and the relatively rare occurrence of mortality in such cases.
In this series, surgery to treat neuromuscular scoliosis had the highest complication rate, at 18.2%. This is consistent with the findings of Reames et al., who based their study on the SRS database. They reported a complication rate of 17.9% in 4657 patients, with a mortality rate of .3%. Cognetti et al. report the highest number of patients undergoing surgery for neuromuscular scoliosis, also based on the SRS database, evaluating 29,019 cases and reporting a complication rate of 6.3%. They report that the differences in their results are due to under-reporting of medical complications.16 Sharma et al. published a systematic review and meta-analysis of 68 cohort and case-control studies, with a total of 15,218 patients in whom the most frequent complications were reported. The most frequently reported were pulmonary complications (22.7%), followed by implant failure (12.9%) and infections (10.9%). Patients with myelomeningocele had the highest incidence of infectious complications.17
In our series, the incidence rate of new neurological deficits associated with scoliosis surgery was 1.4% (11/779). MacEwen et al. were the first to evaluate this complication following the introduction of instrumentation for scoliosis correction. They reported a neurological complication rate of .72% across all diagnoses (idiopathic, congenital, and neuromuscular).18 Coe et al. reported a neurological injury rate associated with scoliosis surgery of .5%.13 Diab et al.19 found a rate of .6% of neurological complications in their review of the surgical treatment of 1301 cases of adolescent idiopathic scoliosis (AIS), and Qiu et al.20 reported a rate of new postoperative neurological deficits of 1.06% in AIS (8/756), 2.89% in congenital scoliosis (11/381), and 3.05% in neuromuscular scoliosis (4/131). Reames et al. reported a rate of 1% (199/19,360) of new neurological deficits, with congenital scoliosis being the condition most commonly associated with this complication.
This study has several strengths. The most notable of these is the large number of cases of the most common subtypes of paediatric scoliosis that were treated in a single hospital by the same surgical team. However, the study also has some limitations. Firstly, the study design and analysis were retrospective. Additionally, the database was primarily designed to capture surgical complications and significant medical morbidity, so it does not record parameters that may also be of interest, such as the magnitude of the deformity and the number of levels instrumented. It should be noted that, although no previous releases or osteotomies were performed on these patients, posterior ligament releases were performed. However, these were not included in the analysis. Further studies will specifically evaluate the latter according to the scoliosis subtype, the long-term results of the correction achieved, the effects on the final instrumented levels, and patient comfort and functional well-being in relation to their usual activities.21,22
ConclusionWe observed an overall complication rate of 8.09% after surgery for paediatric scoliosis. Although neuromuscular scoliosis presented the highest morbidity rate, relatively high complication rates were observed in all groups. These data provide morbidity and mortality rates for paediatric scoliosis surgery that may be useful for surgical planning, patient counselling, and improving patient safety.
Level of evidenceLevel of evidence III.
Ethical considerationsThis study was approved by the Research Ethics Committee of the Italian hospital. The study was conducted in accordance with global and local ethical standards.
FundingNo funding was received for this paper.
Conflict of interestsThe authors have no conflict of interests to declare.