Total hip arthroplasty (THA) is an effective surgery for treating hip osteoarthritis, but access is limited in sub-Saharan Africa due to multiple challenges. This article describes the implementation of a THA program at Monkole Hospital in the Democratic Republic of Congo, focusing on the technical challenges and surgical complications. The objective is to share our experience to assist other professionals and organizations in similar settings.
Materials and methodsEight THA surgery campaigns were conducted between July 2019 and February 2023. Most patients presented with femoral head necrosis secondary to sickle cell anemia. Demographic and surgical data, technical difficulties, and complications were prospectively collected, and follow-up was conducted by a local orthopedic surgeon.
ResultsSeventy-three surgeries were performed on 63 patients with a mean age of 34 years and an average follow-up of 24 months. Seventeen intraoperative technical incidents (23.2%) were observed. The postoperative complication rate was 9.5%, and three patients required revision surgery due to complications.
ConclusionsThe THA program at Monkole Hospital demonstrates that it is feasible to perform complex surgeries in developing countries and that it is a cost-effective procedure that improves patients’ quality of life, provided there are adequate hospital infrastructures, team training, availability of implants, and ensured proper care and follow-up. Training local surgeons and investing in resources are key to the sustainability of the program and the improvement of surgical care.
La artroplastia total de cadera (ATC) es una cirugía efectiva para tratar la osteoartritis de cadera, pero su acceso es limitado en África subsahariana debido a múltiples desafíos. Este artículo describe la implantación de un programa de ATC en el Hospital Monkole de la República Democrática del Congo (RDC), centrándose en los desafíos técnicos y las complicaciones quirúrgicas. El objetivo es compartir nuestra experiencia para ayudar a otros profesionales y organizaciones en entornos similares.
Material y métodosSe han realizado 8 campañas de cirugía de ATC entre julio del 2019 y febrero del 2023. La mayoría de los pacientes presentan necrosis de la cabeza femoral secundaria a anemia drepanocítica. Los datos demográficos, quirúrgicos, dificultades técnicos y complicaciones fueron recolectados de forma prospectiva y el seguimiento fue realizado por un traumatólogo local.
ResultadosSe han realizado 73 cirugías en 63 pacientes con una edad media de 34 años y un seguimiento medio de 24 meses. Se observaron 17 incidencias técnicas intraoperatorias. La tasa de complicaciones postoperatorias fue del 9,5% y 3 pacientes precisaron cirugía de revisión por complicaciones.
ConclusionesEl programa de ATC en el Hospital Monkole demuestra que es posible realizar cirugías complejas en países en desarrollo, y que es un procedimiento costo-efectivo que mejora la calidad de los pacientes. La formación de los cirujanos locales y la inversión en los recursos son claves para la sostenibilidad del programa y la mejora de la atención quirúrgica.
Total hip arthroplasty (THA) is a tremendously effective surgery to treat the pain and disability related to osteoarthritis of the hip.1 Despite the fact that it is one of the most widely performed surgeries in the world and having a high long-term implant survival rate associated with it, the number of procedures performed in sub-Saharan Africa is significantly lower than in other countries.2 This has to do with the many challenges, such as its expense, the lack of specific hospital resources, or the lack of training of healthcare professionals.3
Within this context, many cooperation organisations dedicated to orthopaedic surgery offer care to patients and training to professionals by means of periodic missions, although few are equipped to perform THA surgeries both safely and sustainably.4
The Democratic Republic of Congo (DRC) is a country that finds itself in a highly complex political and socioeconomic situation, characterised by high poverty rates, armed conflicts, and the lack of basic infrastructure. Implementing a THA programme faces a series of issues that include the lack of supplies and medical equipment, paucity of healthcare training, lack of medication, as well as the lack of affordable public health care, in addition to the logistical challenges for transportation with complicated geography and limited road infrastructure.
The purpose of this article is to share our experience in setting up a programme aimed at disseminating and analysing the technical hurdles and surgical complications. We trust that our experience can be of use to other professionals and organisations that work in similar settings.
Material and methodsAll of the interventions were carried out at Hospital Monkole, a referral hospital in Kinshasa, located in the Mont-Ngafula region. The hospital is equipped with 40 in-patient beds, four surgical theatres, sterilisation, a laboratory, radiodiagnosis suite, blood bank, and intensive care unit, all of which are necessary requirements to be able to perform join replacement surgeries safely. This study has undergone the assessment of the Monkole Hospital Institutional Ethics Committee.
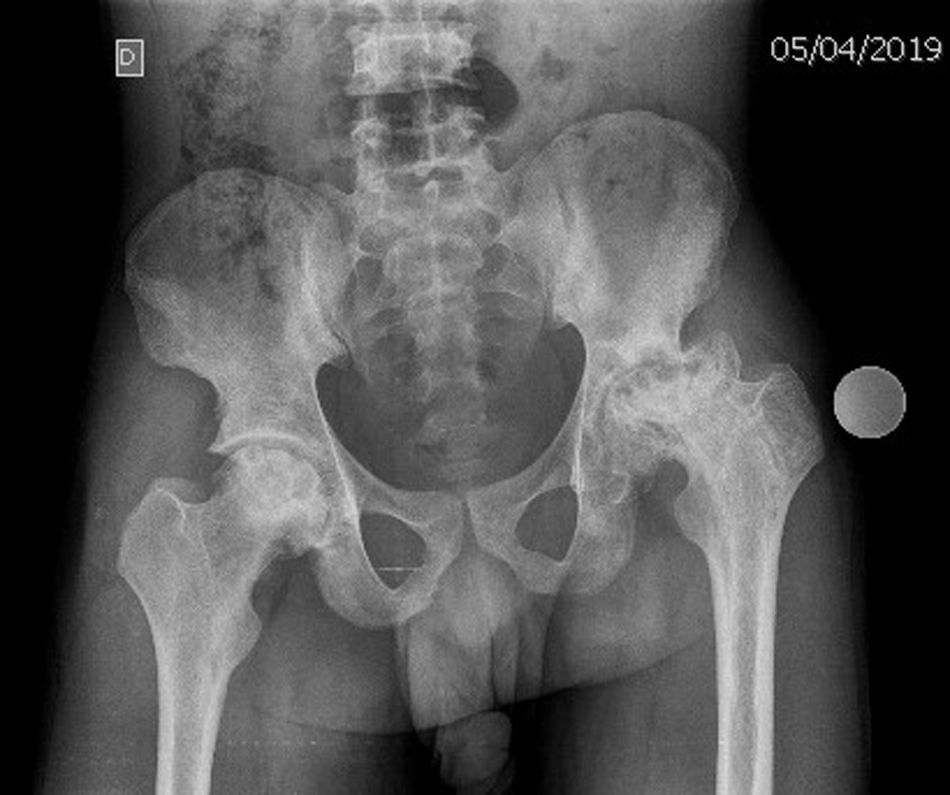
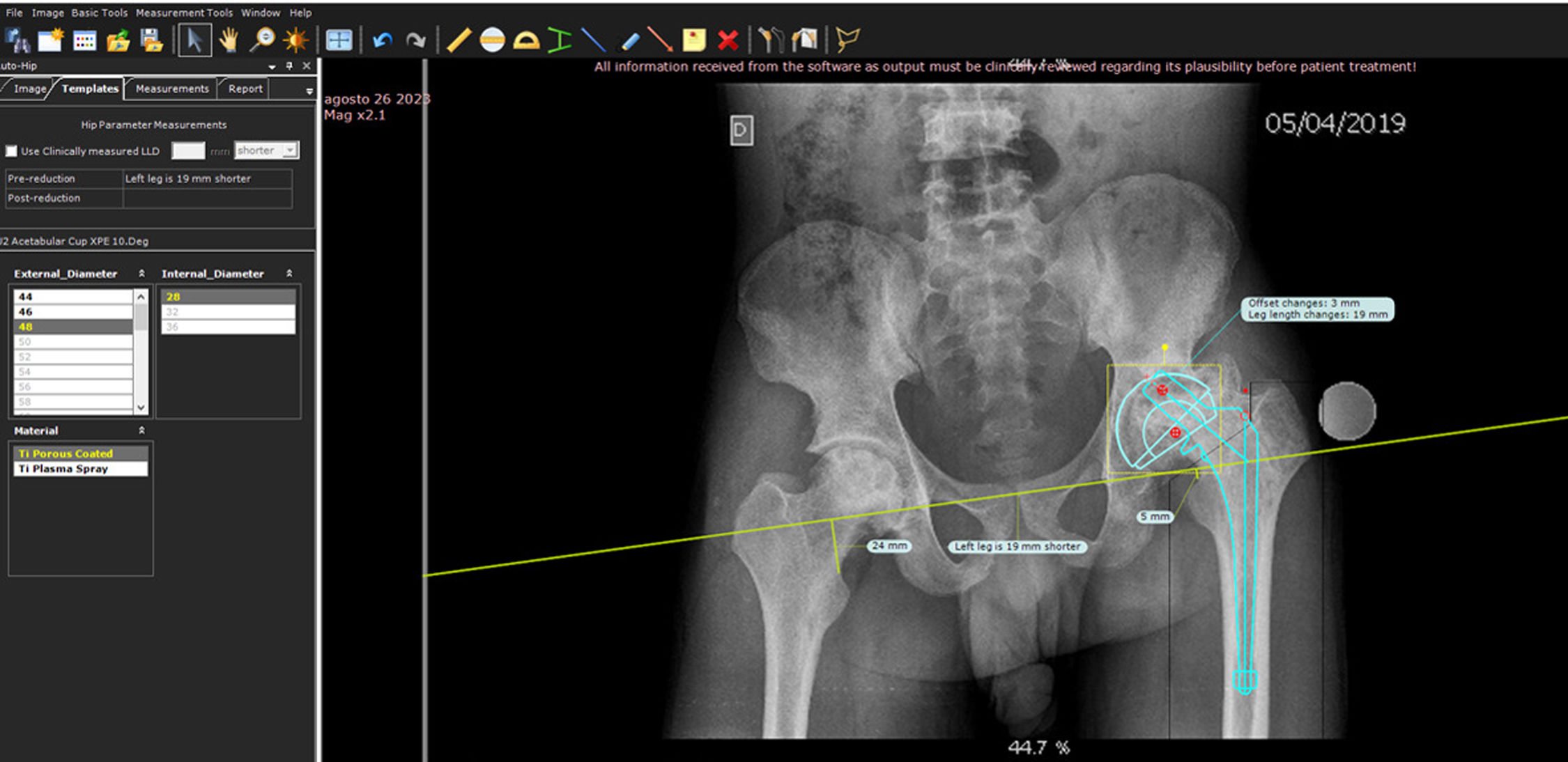
All of the patients were evaluated by one of the authors (JE) who works as an orthopaedist at the hospital since it was opened in 1991. Once the clinical history has been taken and physical examination performed, an AP radiograph of the pelvis with a 26mm is ordered (Fig. 1) and sent by e-mail to the team of surgeons who are specialised in hip surgery (JR and VB) in Spain. With the help of the TraumaCad® (Brainlab) software package, the cases are planned out digitally to choose the implants and anticipate any possible technical difficulties that may arise during the surgery (Fig. 2). Once the final cases have been suggested, the patients are assessed by the local anaesthesia team.
The surgeons (JR and VB) travel from Spain to DRC accompanied by an orthopaedic and traumatology surgical medical resident. All of the surgeries are performed under epidural anaesthesia. As for antibiotic prophylaxis, 2g of endovenous cefazoline/30min prior to skin incision, followed by 3 doses of 1g/every 8h. In those patients suffering from sickle cell anaemia, treatment with oral antibiotics (amoxicillin/clavulanic acid 875/125mg/every 8h) is continued until the day of discharge. As a preventive measure for thromboembolism, low molecular weight heparin 40mg subcutaneously/for 7 days is administered, followed by acetylsalicylic acid 100mg orally until 4 weeks of treatment have been completed. In cemented prostheses, cement with gentamicin and clindamycin is utilised.
Once surgery is completed and prior to transfer to the intensive care unit, an anteroposterior X-ray of the pelvis is performed. On the first postoperative day, patients begin full weight-bearing ambulation with crutches or a walker under the supervision and following the recommendations of the surgical team and without the need for routine physiotherapy. Patients are discharged from the hospital once proper pain management and correct ambulation with technical assistance have been achieved. Follow-up is carried out by JE. The first visit takes place at two weeks for surgical wound care; another one at four weeks for clinical assessment, and then a further consultation coinciding with the Spanish surgeons’ campaign. Any question or incident is notified immediately by means of messages or phone calls.
The demographic, surgical, technical difficulties, and complications were collected prospectively.
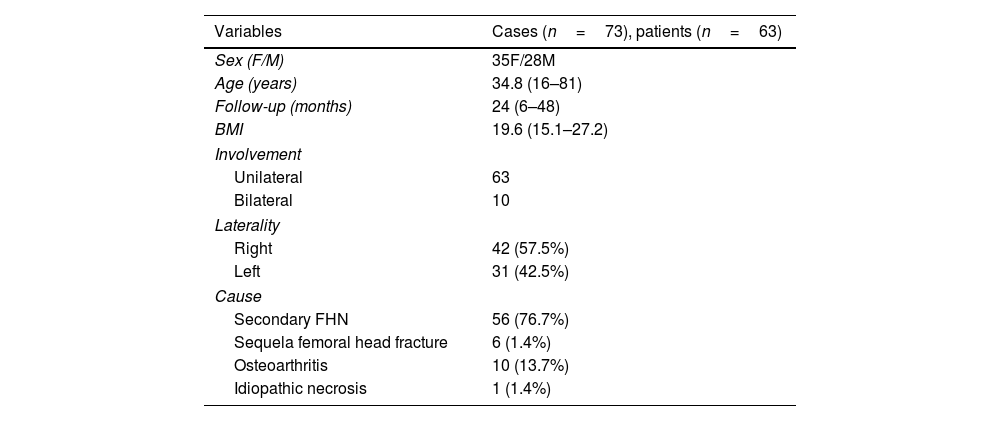
ResultsBetween July 2019 and February 2023, eight surgical campaigns were held at Monkole Hospital, consisting of two campaigns per year. During this period, 73 primary hip arthroplasties were performed in 63 patients, 35 females and 28 males, 10 of which were bilateral surgeries. The mean age of the participants was 34.8 years (16–81). The most common diagnosis was necrosis of the femoral head secondary to sickle cell anaemia. The rest of the demographic data can be seen in Table 1.
Patients’ demographic details and characteristics.
| Variables | Cases (n=73), patients (n=63) |
|---|---|
| Sex (F/M) | 35F/28M |
| Age (years) | 34.8 (16–81) |
| Follow-up (months) | 24 (6–48) |
| BMI | 19.6 (15.1–27.2) |
| Involvement | |
| Unilateral | 63 |
| Bilateral | 10 |
| Laterality | |
| Right | 42 (57.5%) |
| Left | 31 (42.5%) |
| Cause | |
| Secondary FHN | 56 (76.7%) |
| Sequela femoral head fracture | 6 (1.4%) |
| Osteoarthritis | 10 (13.7%) |
| Idiopathic necrosis | 1 (1.4%) |
BMI: body mass index; F: females; FHN: femoral head necrosis secondary to sickle cell anaemia; M: males.
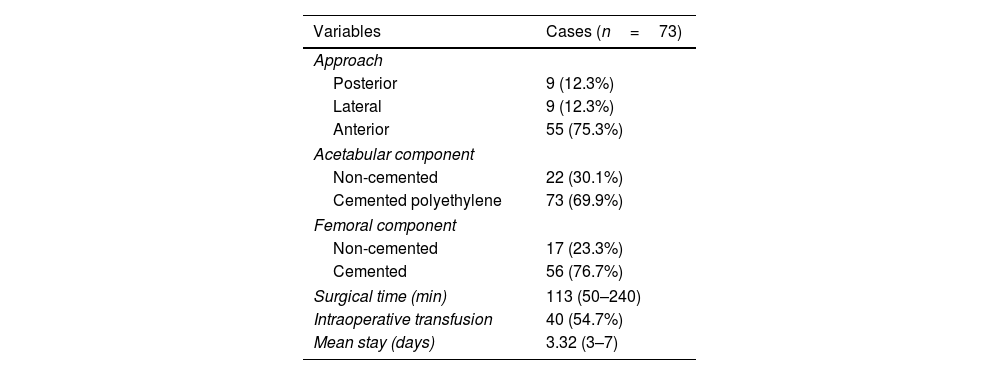
The mean follow-up of the patients was 24 months (6–48). The most commonly used approach was the direct anterior hip approach, performed in 55 patients (75.3%). As for the prostheses implanted. In 17 cases (23.3%) an uncemented stem (Inquileva/Wright) was implanted, while 56 (76.7%) received a cemented stem (UOC, Inquileva, Stryker). An uncemented acetabular component was selected in 22 patients (30.1%) and a cemented polyethylene, in 51 (69.9%). The 32mm femoral head was the most commonly used: 56.1% of cases. Surgical details are displayed in Table 2.
Surgical details.
| Variables | Cases (n=73) |
|---|---|
| Approach | |
| Posterior | 9 (12.3%) |
| Lateral | 9 (12.3%) |
| Anterior | 55 (75.3%) |
| Acetabular component | |
| Non-cemented | 22 (30.1%) |
| Cemented polyethylene | 73 (69.9%) |
| Femoral component | |
| Non-cemented | 17 (23.3%) |
| Cemented | 56 (76.7%) |
| Surgical time (min) | 113 (50–240) |
| Intraoperative transfusion | 40 (54.7%) |
| Mean stay (days) | 3.32 (3–7) |
Of the 63 people who underwent surgery, 3 died of medical causes; one 75-year-old patient died on the fourth postoperative day from heart failure, while the other 2, who had sickle cell anaemia, died of a haemolytic crisis at 6 months and 1 year, respectively.
A total of 17 intraoperative technical incidents (23.2%) were reported. In 14 individuals with sickle cell anaemia, the use of endomedullary burs was necessary because of stenosis secondary to sclerosis related to bone infarcts. Of these, the femoral canal was perforated during femoral canal preparation in 5 patients (6.8%), which was resolved by reorienting the endomedullary guide under fluoroscopic guidance. During acetabular preparation, the motor experienced technical failures in two patients; consequently, acetabular reaming was performed manually. In one patient with sickle cell anaemia, the reduction of the prosthesis (45min) was made difficult because of an error when inserting the stem into the femoral canal and required a tenotomy of the psoas tendon in the lesser trochanter to facilitate the reduction manoeuvre; there were no further complications or sequelae.
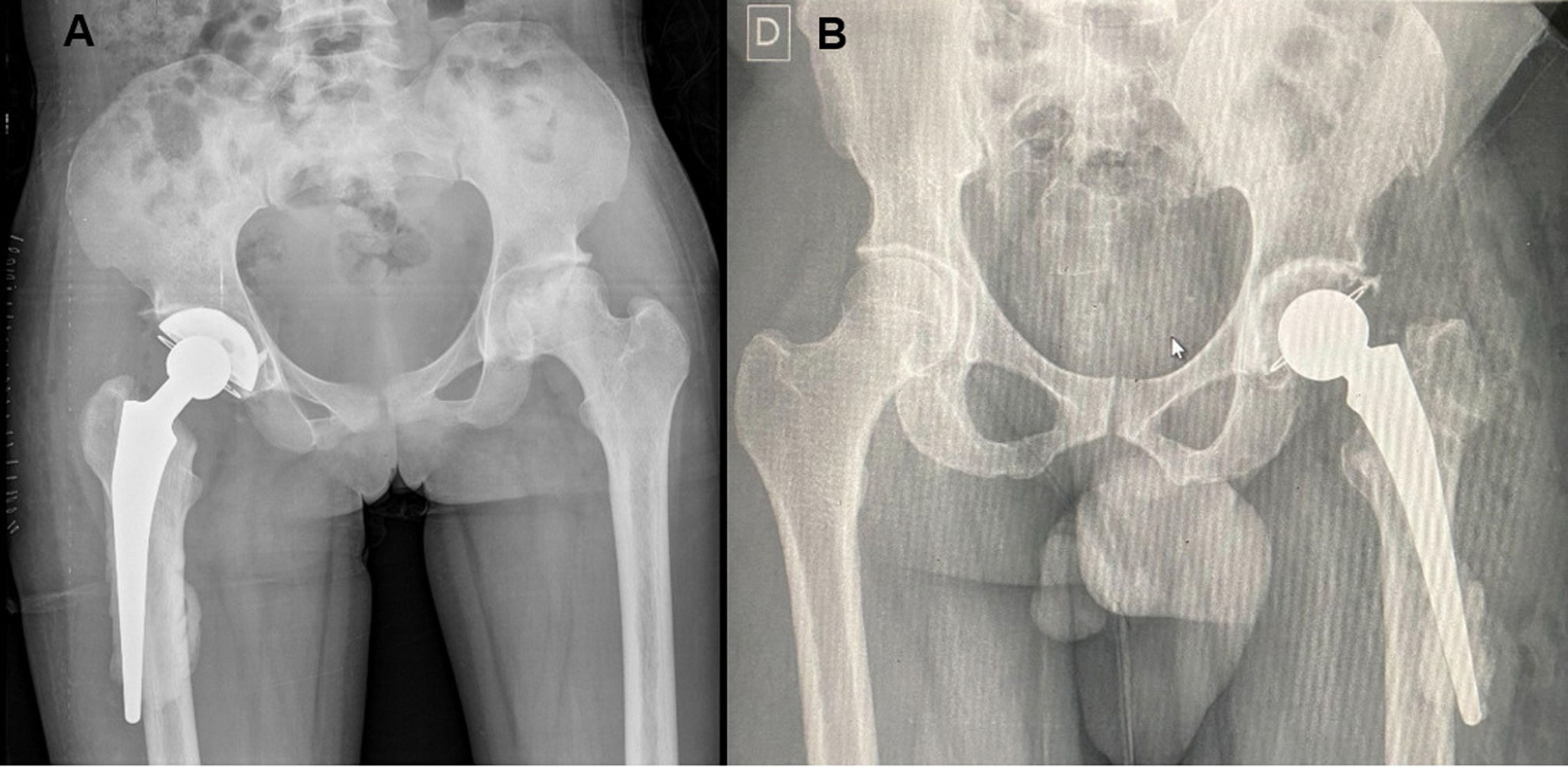
The postoperative complication rate was 9.5% (7/73). Two acute painful crises were reported in patients with sickle cell anaemia during the immediate postoperative phase and were treated with intravenous analgesia, hydration, and oxygen therapy with a favourable response. Two further individuals presented with malpositioning of the stem because of a false pathway (Fig. 3) which was diagnosed on the postoperative radiograph; both were treated conservatively and up and until the time this article was reviewed, they are progressing adequately.
(A) Twenty-six-year-old female patient with sickle cell anaemia who underwent a hybrid total hip arthroplasty of the right hip using a lateral approach. (B) Forty-three-year-old male patient who underwent total cemented arthroplasty of the left hip by means of a direct, anterior approach, due to failed osteosynthesis of the femoral head fracture. In both images, the perforation of the canal can be seen with leakage of the cement and a segment of the stem outside the endomedullary canal.
Three cases required revision surgery due to complications (4.1%). A 68-year-old patient who had undergone THA implantation following a femoral neck fracture developed a chronic periprosthetic infection that was treated by resection arthroplasty. A 24-year-old sickle cell patient with sickle cell anaemia who underwent bilateral hip arthroplasty required acetabular component replacement because of mobilisation at 4 weeks postoperatively (Fig. 4), in relation to a fall. Finally, another 25-year-old sickle cell female patient presented with a haematoma secondary to blunt trauma 12 days postoperatively and was treated by debridement and surgical cleaning; a favourable postoperative outcome was achieved.
DiscussionThis study represents meaningful progress in establishing specialised surgical care in DRC by presenting the first series of THA conducted in the country.
Despite an increase in the number of THA in sub-Saharan African countries in recent years, there is a paucity of bibliographic evidence. In 2007, Mulimba5 presented their vision of the THA in Kenya and the numerous stumbling blocks to be overcome and concluded that, despite the problems encountered, the future of THA surgery in that region is promising. Lubega et al.3 documented the establishment of an arthroplasty registry in Malawi, starting with 73 THA. They reported two cases of dislocation at six weeks after surgery and one revision for aseptic loosening six years following primary surgery. Lisenda et al.6 reported the outcomes of 41 THA performed while setting up an arthroplasty service in Botswana, with one case of subsequent dislocation and no periprosthetic infections or fractures. They concluded that THA can be performed safely in developing countries in selected patients. In another similar study, Mulla et al.7 reviewed the short-term results of arthroplasties carried out in a hospital in Zambia. Of 44 THA implanted, the authors noted two cases of dislocation and one case of revision due to infection. Dossche et al.8 instituted a similar initiative in Burkina Faso, where they carried out 155 THA in a county hospital between 2004 and 2011. They encountered numerous intraoperative technical difficulties including extensive fibrosis and tight femoral canals. The technical problems were linked to the inexpert assistants, leading to periprosthetic fractures, in particular in the early stage. Despite these challenges, the reported acceptable complication rates.
The demographic characteristics of our cohort of patients contrast with the several national arthroplasty registries, as well as with studies of THA in sub-Saharan Africa. The mean age of THAs in the UK registry of 20229 was 69 years of age, clearly older than both the Malawian and Zambian studies,3,7 which had a mean age of 52 and 58 years, respectively. The mean age of our study was 34.8 years, lower even than the Burkina Faso THA study which reported a mean age of 49 years.8 The indication for THA in the UK arthroplasty registry was osteoarthritis accounting for 91.2%,9 which is at the same level as the Botswana and Zambia studies that indicated THA for the same reason in 76 and 70.6%, respectively.6,7 Femoral head necrosis was the number one reason for THA indication in our study, representing 78.1%, results that are consistent with and even superior to those reported in the Malawi and Burkina Faso studies in which femoral head necrosis was also the indication for THA in 49% and 38%, respectively.3,8 The differences in both the mean age as well as the indication for THA can be primarily attributed to the high percentage of THA in individuals with sickle cell anaemia in our series (76.7%).
The high rate of intraoperative technical difficulties reported in our study is closely related to the inherent bone alterations derived from sickle cell disease. The crescent-shaped structural modification of the erythrocyte induces microvascular occlusion that disrupts the blood supply, thereby provoking bone infarction. These repeated vascular insults caused by the flare-ups lead to medullary sclerosis and obliteration of the endomedullary femoral canal.10 Following the recommendation of Dossche et al.,8 we included flexible endomedullary drills in the surgical instrumentation so as to be able to address this specific difficulty in patients with sickle cell anaemia. We also consider digital planning to be very useful, both to identify these cases ahead of time and to anticipate the need for special dysplastic stems. On the other hand, we believe that the use of intraoperative radioscopy in our series contributed to decreasing the risk of perforation and, in those cases in which it did occur, to being able to relocate the femoral canal and properly implant the endomedullary femoral component.
The high rate of intraoperative technical difficulties reported in our study is closely related to the inherent bone alterations derived from sickle cell disease. The crescent-shaped structural modification of the erythrocyte induces microvascular occlusion that disrupts the blood supply, thereby provoking bone infarction. These repeated vascular insults caused by the flare-ups lead to medullary sclerosis and obliteration of the endomedullary femoral canal.10 Following the recommendation of Dossche et al.,8 we included flexible endomedullary drills in the surgical instrumentation so as to be able to address this specific difficulty in patients with sickle cell anaemia. We also consider digital planning to be very useful, both to identify these cases ahead of time and to anticipate the need for special dysplastic stems. On the other hand, we believe that the use of intraoperative radioscopy in our series contributed to decreasing the risk of perforation and, in those cases in which it did occur, to being able to relocate the femoral canal and properly implant the endomedullary femoral component.
Insofar as the terms of the continuity of the programme are concerned, sustainability is clearly heavily dependent on funding, both to be able to purchase the prostheses and for the ongoing training of medical staff and the necessary infrastructure. Nevertheless, it is important to underscore that access to funding in DRC is limited, which hinders the establishment of long-term, sustainable programmes. Likewise, the shortage of companies that distribute medical equipment in the country is a problem that must be addressed in order to ensure access to prostheses and other necessary instruments.
This study has a number of limitations. First of all, patient follow-up is short; nonetheless, we believe that our initial experience with the implementation of the programme and short-term complications is relevant. We are fully aware that the outcome of THA should be appraised with a longer follow-up. Our intention is to follow as many subjects as possible also on a long-term basis, taking into account the possibility that some patients will be lost to follow-up due to travel difficulties and the long distances that some of them have to travel. Furthermore, despite the fact that the data have been collected prospectively, we have been unable to include functional assessment scales and we doubt that the variables probed by the various assessment tools can be extrapolated to the situation experienced by the subjects in this study.
In conclusion, our experience in instituting a THA programme at Monkole Hospital in the DRC has demonstrated that it is possible to perform complex surgeries in developing countries with limited resources. Despite the difficulties encountered, the outcomes of our series are encouraging and illustrate THA is a cost-effective surgery that can improve patients’ quality [of life]. Moreover, training of local surgeons and investing in resources are key to the long-term sustainability of this programme and to enhancing surgical care in the country. We hope that this study will serve as an example for other professionals and organisations interested in the development of orthopaedic surgery in countries with similar needs.
Level of evidenceLevel of evidence III.
Ethical considerationsThis study has been approved by the Institution's Ethical Committee.
FundingThis research has not received any specific grants from any public or commercial agency, or from non-profit organisation.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to offer their most sincere gratitude to friends at Monkole Hospital for their incalculable support and to Medcomtech for their altruistic help in the form of providing implants. Finally, Pablo Martínez, who has been essential to the success of these campaigns.