Articular cartilage lesions have a direct effect on the success of surgical treatment. The aim of this study was to determine the prevalence rate, location, grade, and factors associated with acetabular rim articular cartilage lesions in patients undergoing hip arthroscopy.
Material and methodsA prospective study was conducted by analysing the intraoperative data of 152 hips in 122 patients treated with hip arthroscopy for femoroacetabular impingement from January 2011 to May 2016. The prevalence rate, location, and grade were calculated, as well as the pre-operative factors associated with acetabular rim articular cartilage lesions.
ResultsThe mean age of the patients was 38.6 years. The Tönnis grade was 0 in 103 hips, and 1 in 52 hips. Acetabular rim articular cartilage lesions were present in 109 (70.3%) hips. The location of the lesions was superior-anterior. Independent risk factors for the presence of acetabular rim articular cartilage lesions were an alpha-angle equal or greater than 55°, duration of symptoms equal or greater than 20 months, and Tegner activity scale level equal or greater than 6.
DiscussionAlthough patients were classified as Tönnis grade 0 and 1, and 3T MRI reported acetabular lesions in 1.3% of cases, there was a high frequency of acetabular rim cartilage lesions. Knowledge of the independent risk factors associated with acetabular rim articular cartilage lesions may assist the orthopaedic surgeon with the decision to perform hip arthroscopy.
La presencia de lesión cartilaginosa condiciona en gran medida el resultado funcional de cualquier articulación tras el tratamiento quirúrgico. Nuestro objetivo fue determinar la prevalencia, localización, grado y factores preoperatorios asociados a la lesión cartilaginosa del reborde acetabular en pacientes intervenidos mediante cirugía artroscópica de cadera.
Material y métodosEstudio prospectivo de los hallazgos intraoperatorios en 152 caderas de 122 pacientes consecutivos intervenidos mediante cirugía artroscópica de cadera por choque femoroacetabular entre enero de 2011 y mayo de 2016. Se determinó la prevalencia, localización, grado, y factores preoperatorios asociados a la lesión cartilaginosa del reborde acetabular.
ResultadosLa edad media de los pacientes fue de 36,8 años. El grado de degeneración articular era Tönnis 0 en 103 caderas y Tönnis 1 en 52 caderas. En 109 caderas (70,3%) se detectó lesión cartilaginosa del reborde acetabular. La localización de las lesiones fue superior y anterior. El análisis estadístico estableció como factores preoperatorios independientes para la presencia de lesión cartilaginosa del reborde acetabular un ángulo alfa igual o mayor de 55°, un tiempo de evolución de los síntomas hasta la artroscopia igual o mayor de 20 meses, y un nivel de actividad física en la escala de Tegner igual o mayor de 6.
DiscusiónA pesar de que los pacientes se clasificaron como Tönnis 0 y 1, y que la resonancia nuclear magnética de 3tesla informó de la presencia de lesión cartilaginosa en el 1,3% de los casos, existía una alta frecuencia de lesiones cartilaginosas del reborde acetabular. El conocimiento de los factores predictores preoperatorios asociados a la lesión cartilaginosa del reborde acetabular puede ayudar al cirujano ortopédico sobre la indicación de la cirugía artroscópica de cadera.
Cartilage lesions greatly influence the functional outcome of any joint, since they rarely heal spontaneously, regardless of whether they are acute or chronic.1,2 In the hip, an articular cartilage lesion at chondrolabral level is considered an initial part of early coxofemoral joint degeneration. And if it progress to a full thickness lesion with exposed bone, the cartilage lesion will increase in size and result in articular degeneration.3
Magnetic resonance imaging (MRI) is the test of choice to determine changes in the hip at intra-articular level.4,5 However, its sensitivity and specificity is low for diagnosing chondral lesions, even when using 3T MRI scanners. Therefore, other techniques are recommended with increased diagnostic precision, such as MR arthrography or MIR with traction.6,7 And some authors consider arthroscopic hip surgery (AHS) the benchmark technique for detecting acetabular cartilage lesions.8
The main objective of our work was to study the frequency, location, grade and preoperative factors associated with the presence of an acetabular rim cartilage lesion in a single series of Tönnis stage 0 and 1 patients operated using AHS.
Material and methodsA study was performed from our prospective database of patients who underwent AHS during the period between January 2011 and May 2016. The patients that met the following inclusion criteria were selected: aged less than 50 years, diagnosis of femoroacetabular impingement (FAI), and Tönnis grade 0–1. Patients with hip dysplasia determined by a centre-edge angle of less than 25°, Legg-Calve-Perthes disease, previous hip surgery, avascular necrosis, and aged less than 18 years, were excluded from the study.
All the patients gave their informed consent for inclusion in the study, and the study was approved by our institution's Clinical Research Ethics Committee (CREC).
The modified Harris hip score (mHHs)9 was used for the preoperative clinical assessment, hip assessment questionnaires with the activities of daily living (HOS-ADL) and sports (HOS-SSS)subscales,10 translated into Spanish and validated,11 and questionnaire IHOT12.12 The clinical assessments were performed by 2 surgeons who had not taken part in the surgery.
The level of preoperative physical activity was determined using the Tegner activity scale, with 11 different activity levels from low to high (0–10).13
A standing anteroposterior projection radiograph of the pelvis was requested and axial Dunn projection to establish the presence of a Cam or Pincer-type lesion,1 height of the articular interline on the load area,14 alpha angle1 and extent of articular degeneration according to the Tönnis score.15 Digitalised radiological studies were analysed by 2 surgeons who did not know the name of the patient or the result of the clinical assessment questionnaires. A conventional 3T MRI scan was requested for all patients to determine the presence of an associated intra-articular lesion.
The surgery was performed with spinal anaesthesia, and employing the surgical procedure as described earlier.16
The articular cartilage lesions were classified according to the recommendations of the Multicenter Arthroscopic Hip Outcome Research Network (MAHORN) for acetabular rim cartilage lesions,17 which sets 7 categories: chondromalacia or softening of cartilage, focal defect, extensive lesion, cartilage detachment from the acetabular bone with intact periphery (bubble), cartilage detachment with one open edge of the lesion (pocket), cartilage detachment with more than one open edge (flap), and exposed bone. The geographic method described by Ilizaliturri et al.18 was used to locate the lesion.
SSPS software, version 15.0 (SPSS Inc., Chicago, USA), was used for the statistical analysis. For better statistical management of the data, the time of evolution of symptoms until surgery was classified as less, equal to, and more than 20 months; the alpha angle as less, equal and greater than 55°; the level of physical activity as less, equal and greater than level 6; and the cartilage lesions, with or without cartilage pocket. p values equal or greater than 0.05 were considered significant. The Kolmogorov–Smirnov test was used for normal distribution. The Student's t-test or Mann–Whitney test were used to compare continuous variables, and for categorical variables, the chi-square test for normal distribution variables or the Mantel-Haenszel test for non-parametric data. The relative risk was calculated with its 95% confidence interval in the significant preoperative categorical variables associated with the presence of an acetabular rim cartilage lesion. Multivariate analysis determined the independent factors associated with the presence of an acetabular rim cartilage lesion.
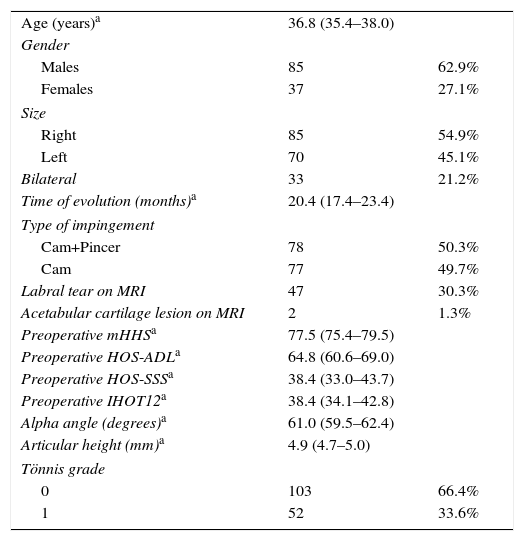
ResultsOver the period of study, 155 hips in 122 patients met the inclusion criteria for the study. The general data of the series are shown in Table 1.
General data of the series.
| Age (years)a | 36.8 (35.4–38.0) | |
| Gender | ||
| Males | 85 | 62.9% |
| Females | 37 | 27.1% |
| Size | ||
| Right | 85 | 54.9% |
| Left | 70 | 45.1% |
| Bilateral | 33 | 21.2% |
| Time of evolution (months)a | 20.4 (17.4–23.4) | |
| Type of impingement | ||
| Cam+Pincer | 78 | 50.3% |
| Cam | 77 | 49.7% |
| Labral tear on MRI | 47 | 30.3% |
| Acetabular cartilage lesion on MRI | 2 | 1.3% |
| Preoperative mHHSa | 77.5 (75.4–79.5) | |
| Preoperative HOS-ADLa | 64.8 (60.6–69.0) | |
| Preoperative HOS-SSSa | 38.4 (33.0–43.7) | |
| Preoperative IHOT12a | 38.4 (34.1–42.8) | |
| Alpha angle (degrees)a | 61.0 (59.5–62.4) | |
| Articular height (mm)a | 4.9 (4.7–5.0) | |
| Tönnis grade | ||
| 0 | 103 | 66.4% |
| 1 | 52 | 33.6% |
ADL: activities of daily living; HOS: Hip Outcome Score; IHOT: International Hip Outcome Tool; mHHS: modified Harris Hip Scores; MRI: magnetic resonance imaging; SSS: Sports Specific Subscale.
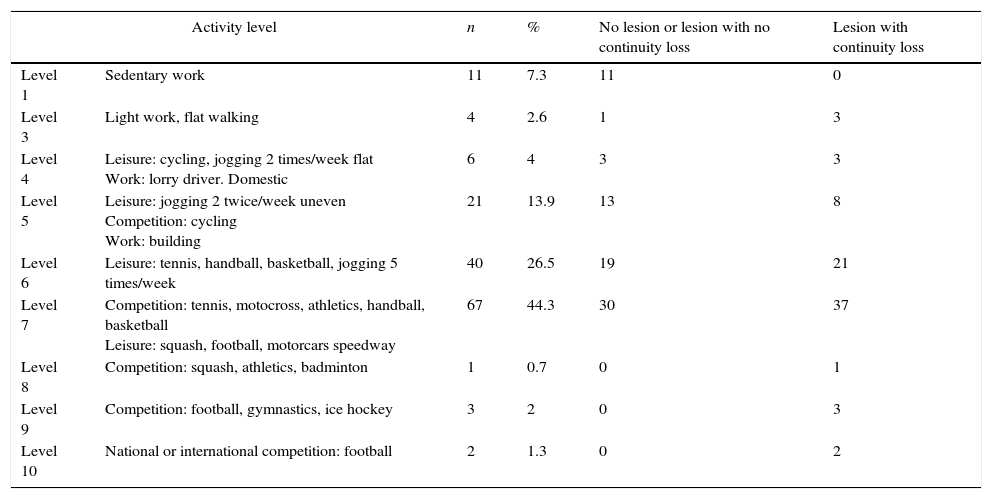
Most of the patients’ physical activity was equal or greater than 6, according to the Tegner activity scale (Table 2).
Preoperative level of physical activity and acetabular rim cartilage lesion.
| Activity level | n | % | No lesion or lesion with no continuity loss | Lesion with continuity loss | |
|---|---|---|---|---|---|
| Level 1 | Sedentary work | 11 | 7.3 | 11 | 0 |
| Level 3 | Light work, flat walking | 4 | 2.6 | 1 | 3 |
| Level 4 | Leisure: cycling, jogging 2 times/week flat Work: lorry driver. Domestic | 6 | 4 | 3 | 3 |
| Level 5 | Leisure: jogging 2 twice/week uneven Competition: cycling Work: building | 21 | 13.9 | 13 | 8 |
| Level 6 | Leisure: tennis, handball, basketball, jogging 5 times/week | 40 | 26.5 | 19 | 21 |
| Level 7 | Competition: tennis, motocross, athletics, handball, basketball Leisure: squash, football, motorcars speedway | 67 | 44.3 | 30 | 37 |
| Level 8 | Competition: squash, athletics, badminton | 1 | 0.7 | 0 | 1 |
| Level 9 | Competition: football, gymnastics, ice hockey | 3 | 2 | 0 | 3 |
| Level 10 | National or international competition: football | 2 | 1.3 | 0 | 2 |
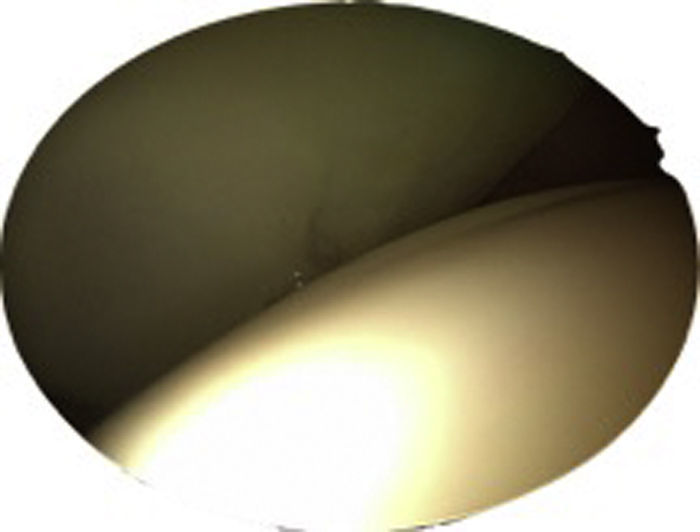
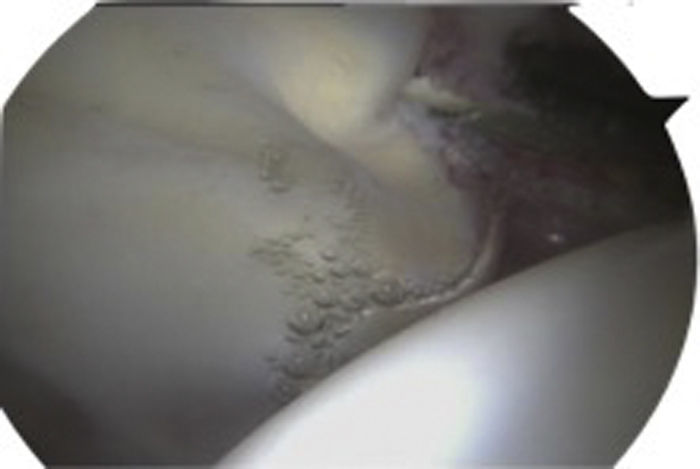
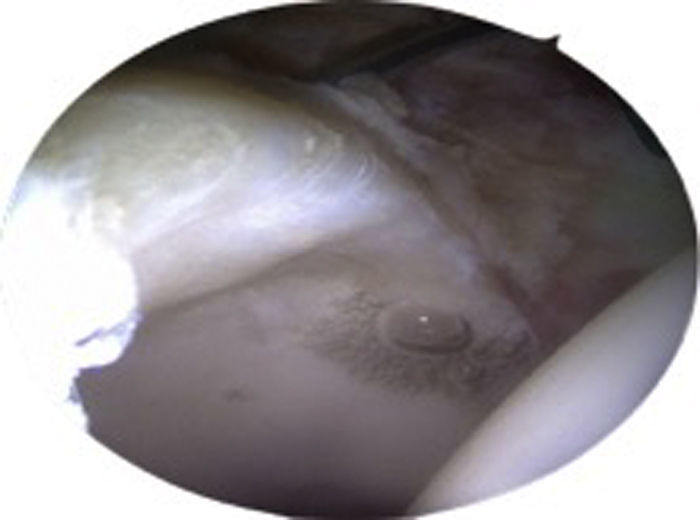
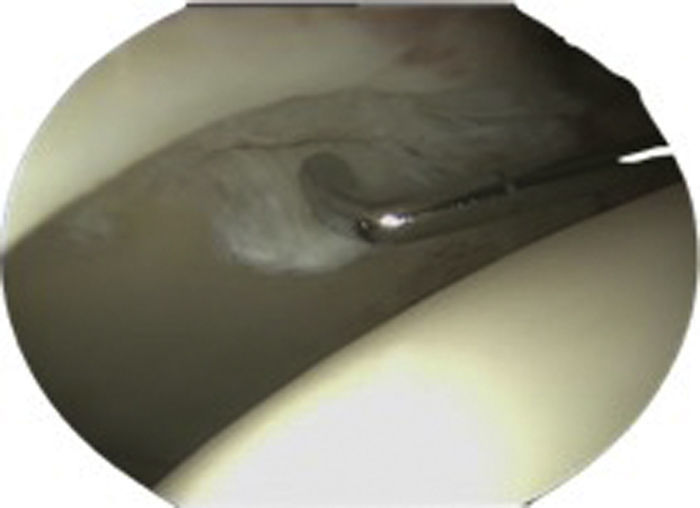
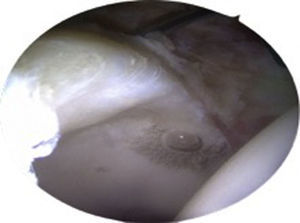
Arthroscopically, there were no acetabular rim cartilage lesions in 46 hips (29.6%) (Fig. 1) whereas in 109 hips (70.3%), some extent of cartilage lesion was detected. Of those, there was softening of cartilage in 13 (8.3%) (Fig. 2); bubble in 18 (11.6%), (Fig. 3); pocket in 33 (21.2%), (Fig. 4); flap in 23 (14.8%) (Fig. 5), and in 22 (14.5%) there was exposed bone (Fig. 6). The cartilage lesion had no open edges in 31 hips (28.4%), while 78 did (71.6%). The cartilage lesions were located in areas 2 and 3. No cartilage lesions were detected in the femoral head.
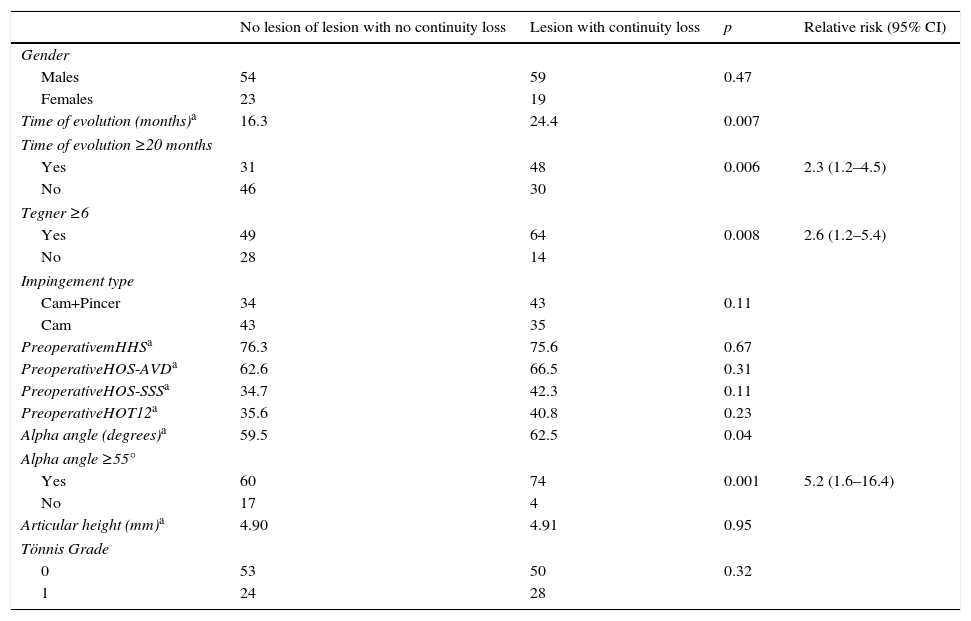
In the univariate analysis, the mean time from onset of symptoms until surgery was longer for the patients with acetabular cartilage lesions and open edges, than that of the patients with no cartilage lesions or with cartilage lesions but no open edges. The differences were significant (p=0.007 and p=0.04, respectively). When categorising the variables into evolution time equal or greater than 20 months, Tegner activity level equal or greater than 6, and alpha angle equal or greater than 55°, the differences with respect to the presence of a cartilage lesion with open edges were significant (p=0.006, p=0.008, and p=0.001, respectively) (Table 3).
Univariate analysis with regard to acetabular cartilage lesion.
| No lesion of lesion with no continuity loss | Lesion with continuity loss | p | Relative risk (95% CI) | |
|---|---|---|---|---|
| Gender | ||||
| Males | 54 | 59 | 0.47 | |
| Females | 23 | 19 | ||
| Time of evolution (months)a | 16.3 | 24.4 | 0.007 | |
| Time of evolution ≥20 months | ||||
| Yes | 31 | 48 | 0.006 | 2.3 (1.2–4.5) |
| No | 46 | 30 | ||
| Tegner ≥6 | ||||
| Yes | 49 | 64 | 0.008 | 2.6 (1.2–5.4) |
| No | 28 | 14 | ||
| Impingement type | ||||
| Cam+Pincer | 34 | 43 | 0.11 | |
| Cam | 43 | 35 | ||
| PreoperativemHHSa | 76.3 | 75.6 | 0.67 | |
| PreoperativeHOS-AVDa | 62.6 | 66.5 | 0.31 | |
| PreoperativeHOS-SSSa | 34.7 | 42.3 | 0.11 | |
| PreoperativeHOT12a | 35.6 | 40.8 | 0.23 | |
| Alpha angle (degrees)a | 59.5 | 62.5 | 0.04 | |
| Alpha angle ≥55° | ||||
| Yes | 60 | 74 | 0.001 | 5.2 (1.6–16.4) |
| No | 17 | 4 | ||
| Articular height (mm)a | 4.90 | 4.91 | 0.95 | |
| Tönnis Grade | ||||
| 0 | 53 | 50 | 0.32 | |
| 1 | 24 | 28 | ||
ADL: activities of daily living; HOS: Hip Outcome Score; CI: confidence interval; IHOT: International Hip Outcome Tool; mHHS: modified Harris Hip Scores; MRI: magnetic resonance imaging; SSS: Sports Specific Subscale.
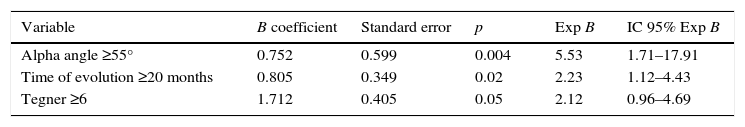
Binary logistic regression with acetabular rim cartilage lesion as an independent variable established that an alpha angle equal or greater than 55°, a time of evolution of symptoms until surgery equal or greater than 20 months, and a physical activity level equal or greater than 6 were predictive factors associated with the presence of an acetabular rim cartilage lesion (Table 4).
Binary logistics regression with acetabular rim cartilage lesion as independent variable.
| Variable | B coefficient | Standard error | p | Exp B | IC 95% Exp B |
|---|---|---|---|---|---|
| Alpha angle ≥55° | 0.752 | 0.599 | 0.004 | 5.53 | 1.71–17.91 |
| Time of evolution ≥20 months | 0.805 | 0.349 | 0.02 | 2.23 | 1.12–4.43 |
| Tegner ≥6 | 1.712 | 0.405 | 0.05 | 2.12 | 0.96–4.69 |
CI: confidence level. Exp B: odds ratio.
The most important findings in our study were: (1) the prevalence of acetabular rim cartilage lesions in a series of patients aged less than 50 years with a diagnosis of FAI and Tönnis 0 and 1 radiological study was 70.3%; and of those, 71.6% were lesions with open edges; (2) the alpha angle, evolution time from the onset of symptoms until arthroscopic surgery, and physical activity level were predictive factors of acetabular rim cartilage lesion.
The development of hip preservation surgical techniques has enabled cartilage lesions to be identified with greater accuracy. Anderson et al.19 report 44% chondrolabral lesions in 64 hips with a diagnosis of FAI treated by safe dislocation. McCarthy and Lee20 published the presence of 59% acetabular cartilage lesions in an anterior location, 24% in a superior location, and 25% in a posterior location, in 457 hip arthroscopies. Fontana et al.21 report 96.1% acetabular cartilage lesions in their series of 359 hip arthroscopies—all cases were Tönnis grade 0–1—of which 246 were operated with a diagnosis of FAI. And Bhatia et al.,22 reported 80.9% full thickness cartilage lesions in 308 hip arthroscopies. In our series, some degree of acetabular rim cartilage damage was found in 70.3% of the hip arthroscopies undertaken.
The sensitivity and specificity of conventional MRI scanning in diagnosing acetabular cartilage lesions is low.4,5 According to our results, acetabular cartilage lesion was reported in 2 hips only (1.3%). Arthro-MRI detects chondral lesions earlier. Keeney et al.23 report a 62.7% correlation between arthroscopic and arthro-MRI findings. However, other authors indicate that it has technical limitations,24,25 its diagnostic performance is improved if used with traction.7 Schmaranzer et al.6 report a diagnostic precision of 83–91% for acetabular chondropathy with this technique. Based on the current literature, and given the need to detect acetabular cartilage damage preoperatively, arthro-MRI with traction is recommended.
Outerbridge26 has classified cartilaginous lesions historically. In 2003, the International Cartilage Repair Society (ICRS) proposed a classification based on that of Outerbridge, but with subgroups for better definition of the lesion, which has achieved broad international consensus for its use.27 In the hip, the pathophysiology of FAI causes a labral tear associated with acetabular rim cartilage lesion in the area adjacent to the tear. These lesions are often associated with the presence of Cam-type FAI, as described previously by Ganz et al.28 In order to classify these combined lesions, in 2005 Ranawat and Kelly described the Acetabular Labrum Articular Disruption (ALAD) classification.29 And the MAHORN group proposed a classification for the different types of labral tears, another for acetabular cartilage lesions excluding the acetabular rim, and a third specific classification for acetabular rim cartilage lesions.17
The concave surface of the acetabulum is more exposed to shearing forces than the femoral head, and the cartilage thickness is less, which would explain the greater frequency of acetabular cartilage lesions compared to femoral cartilage lesions.30,31 In our series, we found no femoral cartilage lesion, unlike Fontana et al.21 who report 68% femoral cartilage lesions, always associated with acetabular cartilage lesions; and Bhatia et al.,22 report 39.3% cartilage lesions of the femoral head, although only 49.1% associated with acetabular cartilage lesions.
The most frequent location for acetabular cartilage lesions is anterosuperior, as reported by Anderson et al.,19 Fontana et al.,21 and Bhatia et al.22; and this coincides with our results in areas 2 and 3 according to the method of Ilizaliturri et al.18 This pattern of cartilage lesion is associated with Cam-type FAI, in which the altered morphology of the femoral head impacts the anterosuperior acetabular area in flexion movements of the hip, causing the initial chondral delamination, and over time, full thickness chondral lesion.30,31 All the hips In our series presented Cam-type FAI to a greater or lesser extent.
Detection of acetabular cartilage lesion on hip arthroscopy has been associated with a time of evolution of symptoms until surgery equal or greater than 20 months, an alpha angle equal or greater than 55°, and a physical activity level equal or greater than 6. Bhatia et al.22 find an association of full thickness cartilage lesion with being older than 45 years, male, mean time of evolution of symptoms until surgery greater than 30 months, alpha angle greater than 55°; but not with type of sports activity, or body mass index (BMI). Anderson et al.19 indicate that acetabular chondral delamination is associated with the male gender and Cam-type FAI. And Johnston et al.31 report that the greater the alpha angle, the more severe the chondral lesion of the acetabular rim.
There are authors who argue the case for mini-open surgery of FAI without exploring the central compartment. Chiron et al.32 report 118 cases of FAI in their series—of whom 22.4% were aged over 40 years and 27.2% presented Tönnis grade 2–3—a significant improvement in the assessment questionnaires after mini-open surgery without exploring the central compartment, and suturing the labrum in only one case; but with a mean follow-up of 2.2 years. Other authors also report good outcomes with mini-open surgery but combine the procedure with arthroscopy to assess and treat central compartment pathology.33,34 Longer term studies relate cartilage lesion with poor clinical outcomes after FAI,35–37 therefore, the current recommendation should be that they are diagnosed and treated.
Our study has limitations. Our patients attended our consultations to obtain information on hip arthroscopy, which could be a bias to be taken into account. Furthermore, we did not establish other variables reported in the literature which influence cartilage damage such as acetabular cover and BMI. And neither did we analyse the outcome of treatment carried out according to the factors studied.
Strengths of the study worth noting are that it was performed by multiple observers, who did not know the data on the study sections in which they did not participate. Another strength is the use of relative risks as a very useful tool for decision-making in daily clinical practice with regard to the type of surgical treatment and the time it is indicated.
ConclusionAcetabular cartilage lesions detected on hip arthroscopy are associated with the time of evolution of symptoms until surgery, the alpha angle value, and a high level of physical activity.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of humans and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Más Martínez J, Sanz-Reig J, Verdú Román CM, Bustamante Suárez de Puga D, Morales Santías M, Martínez Giménez E. Lesión cartilaginosa del reborde acetabular en estadios Tönnis 0 y 1: incidencia, grado, localización y factores preoperatorios asociados. Rev Esp Cir Ortop Traumatol. 2017;61:154–161.