Periprosthetic humerus fractures are infrequent and sometimes difficult to treat. There is limited literature and no consensus on the handling of these fractures. The objective of this study was to compare our results with those published in the literature, in order to improve our care and propose a management algorithm.
Material and methodObservational study of 10 cases of periprosthetic humerus fractures with a mean follow-up of the patients of 23 months. An analysis of sociodemographic, radiological and surgical variables was performed. They were reviewed clinically and by telephone using the UCLA Shoulder Score and Quick-DASH scales. A systematic search was made in Pubmed for periprosthetic humerus fractures, for a literature review with which to compare our series.
ResultsWe analysed 10 patients with an average age of 69.4 years (37–91). Of the patients, 90% underwent surgery through open reduction and internal fixation. Nine of the ten patients consolidated in a mean time of 6.2 months (range 5–12), the remaining suffered a new fracture 5 months after the intervention, who were reoperated and a new osteosynthesis performed with bone allograft. In the UCLA scale there was a decrease of 10.66 points, and an increase of 27.3 points in the Quick-DASH, at the end of the follow-up.
ConclusionsIn our series of cases we found similarities in the literature, in relation to demographic aspects and obtaining good radiographic results, which do not correspond to the functional outcome of patients.
Las fracturas periprotésicas de húmero son infrecuentes y su manejo, difícil. La bibliografía es limitada y no existe consenso sobre su tratamiento.
Material y métodoHemos realizado un estudio observacional retrospectivo de 10pacientes con fractura periprotésica de húmero con un seguimiento de 25,1meses (6-87). Valoramos los resultados clínicos, radiológicos y funcionales, como las complicaciones. Utilizamos el cuestionario Quick-DASH y UCLA Shoulder Score (UCLASS). Realizamos una búsqueda sistemática para comparar la serie presentada y los protocolos de tratamiento publicados.
ResultadosDiez pacientes con una media de edad de 69,4años (37-91) fueron intervenidos quirúrgicamente: 8 mediante reducción abierta y fijación interna (RAFI), en otro se realizó un recambio protésico colocando una nueva prótesis con un vástago más largo, y en el último se retiró la prótesis y se realizó una osteosíntesis con un clavo endomedular. Nueve de 10 pacientes consolidaron en un tiempo de 6,2meses (rango 5-12); el restante sufrió una nueva fractura 5meses después, siendo reintervenido, realizándole una nueva osteosíntesis, con aporte de aloinjerto óseo, que consolidó a los 8meses de la última fractura. En relación con la situación previa a la fractura, los pacientes tenían como promedio un descenso notable de la función, que era de 10,66puntos en el test de UCLASS y un ascenso de 27,3 puntos en el cuestionario Quick-DASH.
ConclusionesNuestra serie tiene similitudes con las publicadas en relación con los aspectos demográficos, las complicaciones y el tiempo de consolidación. Sin embargo, en otros aspectos, como el dolor y los resultados funcionales, encontramos gran variabilidad.
In recent years there has been an increase in the surgical treatment of proximal humerus fractures, and with it the indication for shoulder prostheses. The same has occurred in the treatment of degenerative shoulder pathologies.1 Thus, it is more than possible that an increase in the incidence of periprosthetic humerus fractures will be observed in the coming years. Periprosthetic humerus fractures are currently rare, with a prevalence in the literature of 0.6%–2%,2,3 although their incidence varies according to the published series, which even reaches 11% if those that occur during surgery and those occurring post-operatively are included.4
The little experience in the treatment of this type of fracture, together with their complexity, requires studies to be conducted in which the results obtained with the different treatments are published, along with the complications that occurred and how they were resolved.
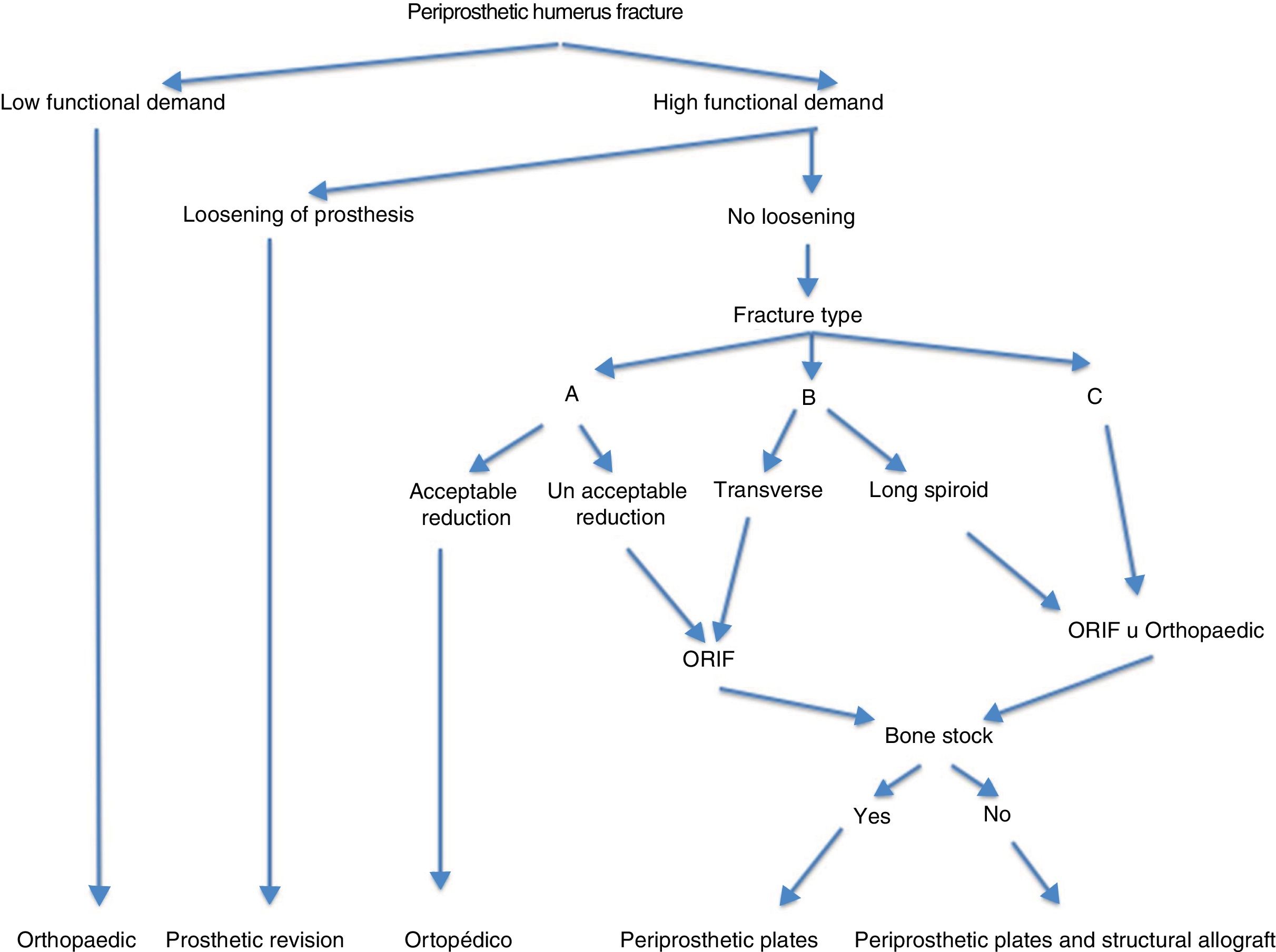
With this paper we seek to evaluate the results obtained with the surgical treatment of periprosthetic humerus fractures treated in our department and to carry out a review of the literature on these fractures, with a view to proposing a treatment algorithm.
Material and methodFollowing approval by the centre's ethics committee, a review was carried out of all patients who had undergone surgery following a periprosthetic humerus fracture during the period from January 2009 to December 2016.
We included all patients who presented with a periprosthetic humerus fracture who had a prosthesis at the proximal end of the humerus. We collected the following sociodemographic and surgical variables: age, sex, Charlson comorbidity index,5 fracture type according to Wright and Cofield's6 classification, type of arthroplasty, surgical technique, surgical delay, time from arthroplasty to fracture, readmissions and complications. Intraoperative and conservatively treated fractures were excluded, as well as the patients lost to follow-up.
Clinical and radiological assessmentA clinical and radiographic assessment was made throughout the follow-up, and at the end of the follow-up the clinical situation of the patient was evaluated, with special interest in their degree of pain and mobility. The clinical assessment was performed using the UCLA Shoulder Score (UCLASS)7 and the Quick-DASH8 questionnaires, through a specific clinical interview and using the data recorded in the patient's medical history.
Statistical analysisA descriptive statistical analysis was performed using SPSS v22 (IBM Chicago, IL, USA) statistical software, obtaining measures of central tendency and dispersion for the quantitative variables, and measures of frequency distribution for the qualitative variables. Due to the limited sample size, no statistical hypothesis tests were performed.
Literature reviewFinally, a search was conducted on Pubmed with the terms “periprosthetic humeral fractures”, which yielded a total of 106 articles. After the review and after applying inclusion criteria (series with more than 3 patients, follow-up of more than 1 year, and patients wearing either a partial, total or inverted shoulder prosthesis), we were left with 12 articles. Some of these papers included patients with both intra-operative and post-operative fractures. In this study we only analysed the fractures that occurred after surgery.
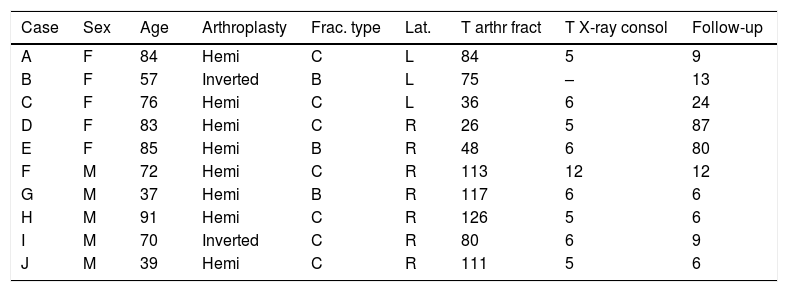
ResultsSociodemographic resultsTen patients presenting with a postoperative periprosthetic fracture of the humerus were assessed. The mean age of the sample at the time of the fracture, was 69.4 years (range 37–91 years); 5 patients were male and 5 female. With respect to laterality, 7 of the 10 fractures affected the right humerus and the other 3 the left.
In all the patients the mechanism of production was low energy after an accidental fall from their own height.
In 8 cases (80%) the patients had an implanted shoulder hemiarthroplasty and the other 2 (20%) had an inverted arthroplasty. The type of fracture according to Wright and Cofield's classification was 7 type C cases (70%), and type B in the remaining 3 (30%). The mean follow-up time was 25.1 months (6–87).
Regarding fracture consolidation, 9 cases (90%) consolidated without incident, while one patient presented a new fracture 5 months following osteosynthesis, requiring a further intervention, which consolidated 8 months later. The average time of consolidation of the 9 cases was 6.2 months (range 5–12 months). We decided not to include the case of refracture, since it modified the results of this parameter in an anomalous way.
The data for each patient are detailed in Table 1.
Series of patients with periprosthetic fracture.
| Case | Sex | Age | Arthroplasty | Frac. type | Lat. | T arthr fract | T X-ray consol | Follow-up |
|---|---|---|---|---|---|---|---|---|
| A | F | 84 | Hemi | C | L | 84 | 5 | 9 |
| B | F | 57 | Inverted | B | L | 75 | – | 13 |
| C | F | 76 | Hemi | C | L | 36 | 6 | 24 |
| D | F | 83 | Hemi | C | R | 26 | 5 | 87 |
| E | F | 85 | Hemi | B | R | 48 | 6 | 80 |
| F | M | 72 | Hemi | C | R | 113 | 12 | 12 |
| G | M | 37 | Hemi | B | R | 117 | 6 | 6 |
| H | M | 91 | Hemi | C | R | 126 | 5 | 6 |
| I | M | 70 | Inverted | C | R | 80 | 6 | 9 |
| J | M | 39 | Hemi | C | R | 111 | 5 | 6 |
R: right; F: female; Hemi: hemiarthroplasty of the shoulder; L: left; Inverted: inverted shoulder prosthesis; Lat: laterality; M: male; Follow-up: in months; T arthr fract: time from arthroplasty surgery to fracture in months; T X-ray consol: time from intervention to radiological consolidation in months; Frac type: type of fracture according to the Wright and Cofield classification.
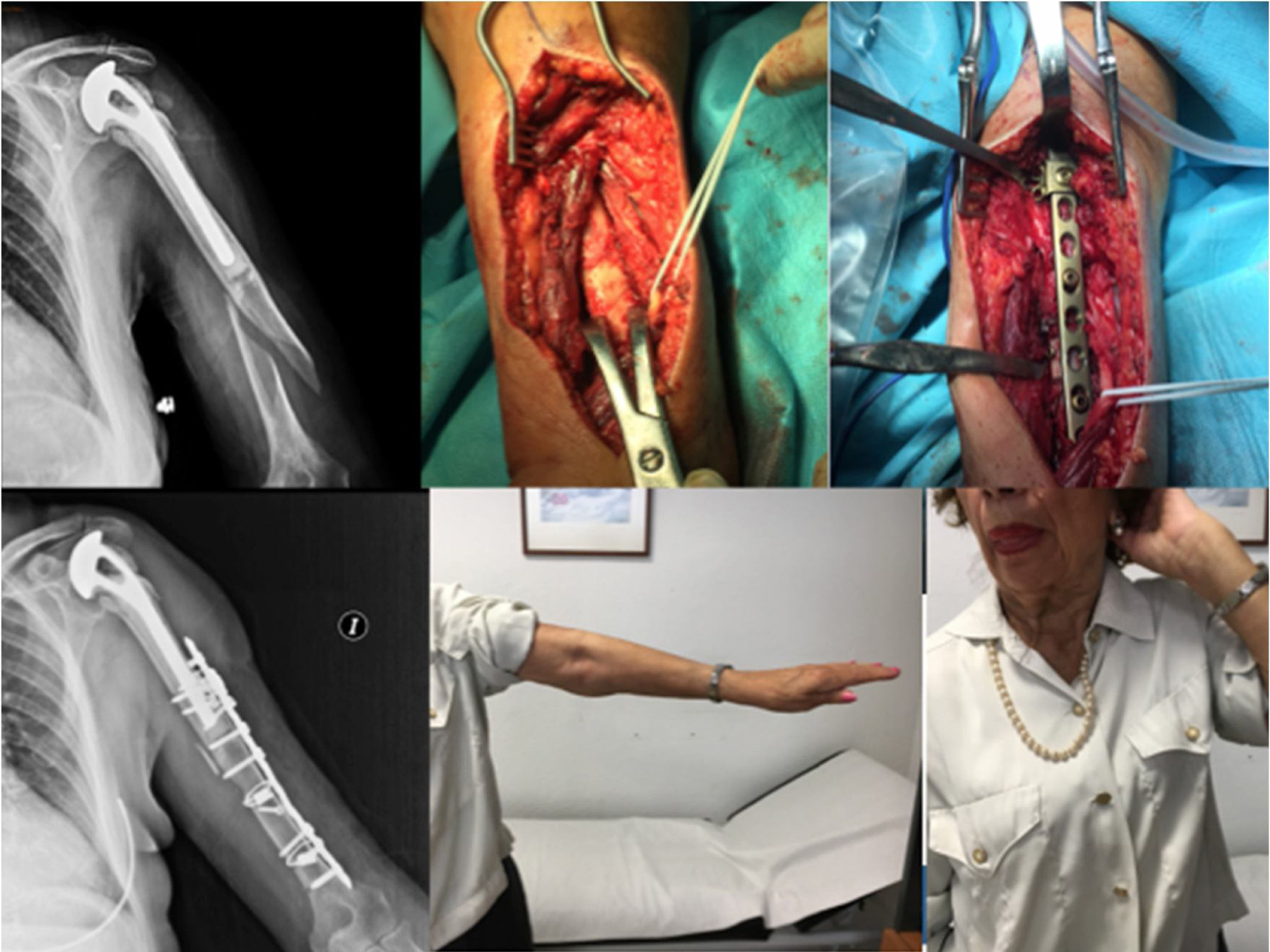
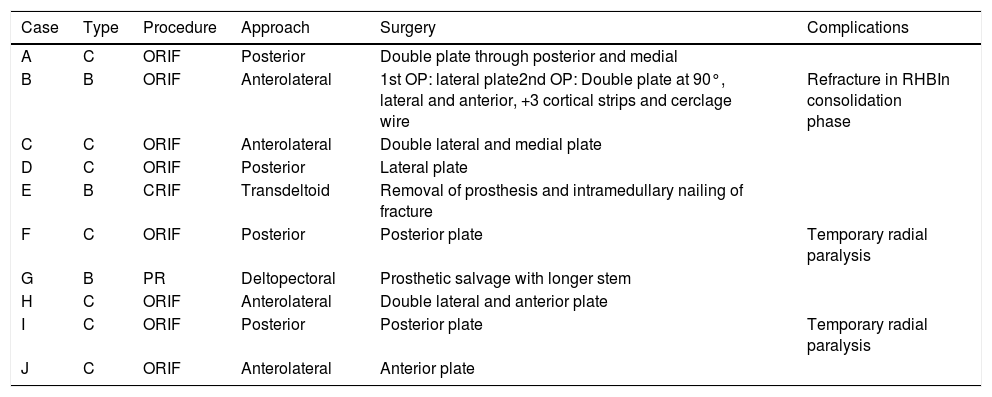
Surgical treatment was performed in all the patients in the series. Eight (80%) were operated by open reduction and internal fixation (ORIF) with LC-DCP or screwed LCP plate, while in one patient replacement of the arthroplasty was chosen, with a longer stem, and in the other case the prosthesis was removed and the fracture fixed with an intramedullary nail. The reason for treating one periprosthetic fracture by removing the prosthesis and performing an intramedullary nailing was due to the patient's high comorbidity and the low mobility of her limb; in addition, she had seriously deteriorated due to advanced Alzheimer's disease.
Four posterior approaches were performed, all of them to treat distal fractures at the tip of the stem, type C. In all of them we performed an osteosynthesis with plate and screws in the most distal part, while in the proximal part it was only possible to perform the osteosynthesis with screws in 2 cases, while in the other 2 we performed a mixed assembly with screws and cerclage wires to achieve correct fixation. Two patients had radial nerve paralysis, which recovered spontaneously in a few months, two neuroapraxias. Both patients had undergone a posterior approach, one of them was treated with a mixed system of cerclage wires and screws, while in the other only screws were used in the osteosynthesis
In the 4 remaining patients who were treated with osteosynthesis, an anterolateral approach to the arm was used, following the lateral edge of the biceps as a reference; in 3 of these patients osteosynthesis was performed with a plate and screws, and cerclage wires needed to be used in the remaining patient for correct reduction and osteosynthesis.
As for the two patients not treated with osteosynthesis, a deltopectoral approach was used in the first to then replace the prosthesis placing a longer stem, since the first had loosened. In the remaining patient, as mentioned above, given their precarious situation, the prosthesis was removed, and the fracture was fixed with an intramedullary nail.
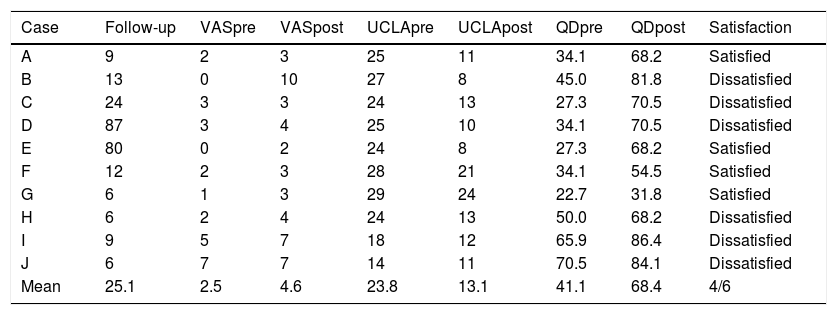
Functional testsWe performed a functional assessment prior to the fracture by assessing the clinical history data and through a clinical interview with the patient. The final assessment was obtained on completion of the follow-up; the results obtained in the pre and final assessment were compared with the shoulder functionality tests.
With regard to joint balance, the degrees of mobility recorded before the fracture and at the end of the follow-up were assessed. We observed a decrease in average joint balance of 23° in flexion, 21° in abduction, 13° in internal rotation and 16° in external rotation.
With regard to functionality, we observed a worsening in all the parameters measured, both in relation to pain and in the functional tests. Baseline pain increased on average by 2.1 (1–10) points on the VAS scale. UCLASS worsened by 10.7 (3–19) points and Quick-Dash worsened by 27.3 (9.1–40.9) points.
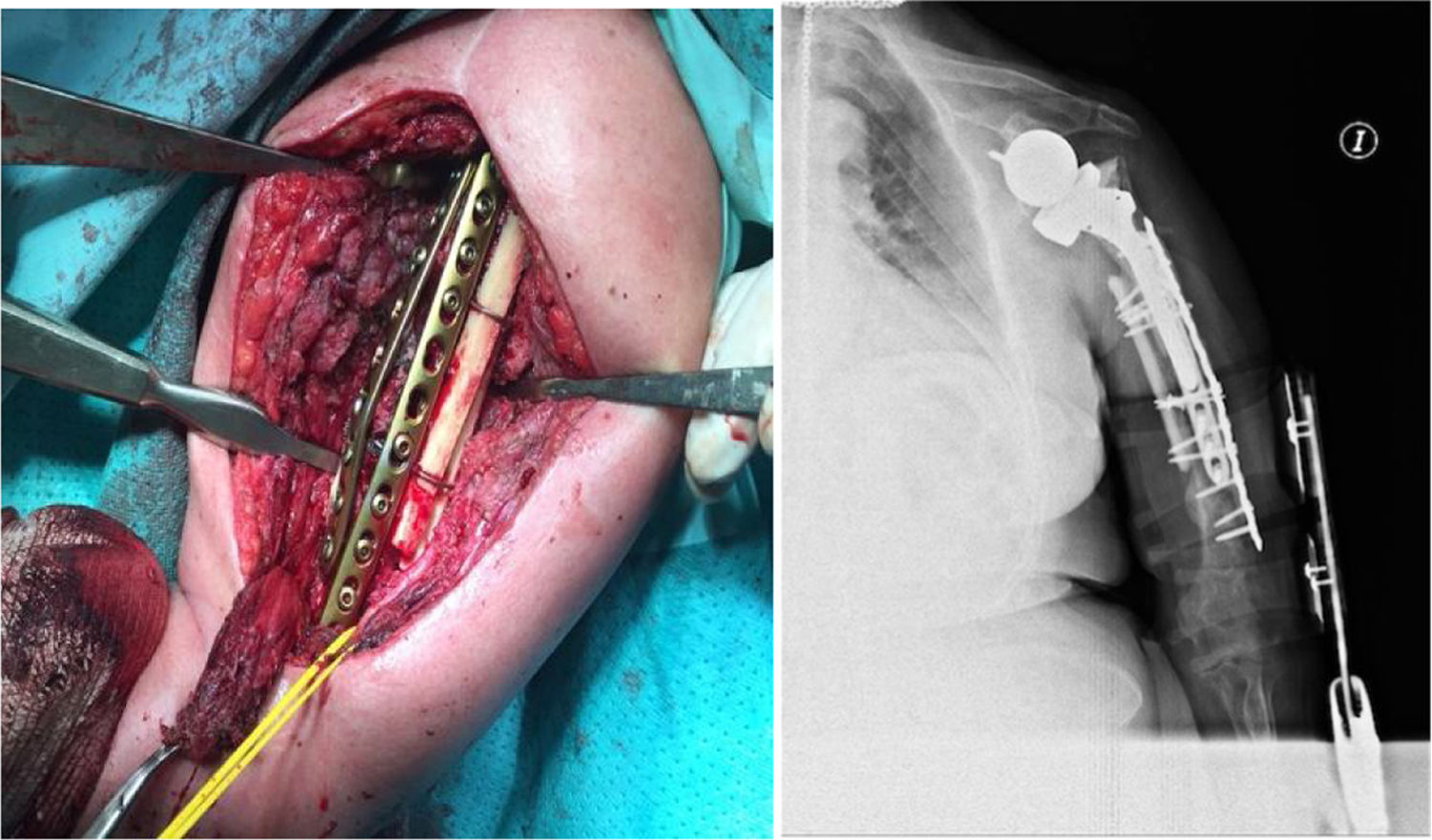
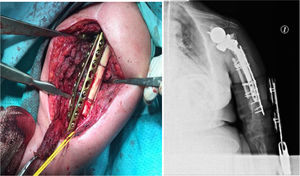
ComplicationsThree patients (30%) suffered some kind of complication (30%). Two patients, as mentioned above, presented postoperative neuroapraxia of the radial nerve, and completely recovered 6 months later. A third patient presented a new fracture (Fig. 1) during a rehabilitation session, for which he was again operated performing an open reduction and internal fixation (Fig. 2). No other complications were reported, such as infection, thrombosis or movement of the osteosynthesis material. Table 2 shows a summary of the approach, the osteosynthesis method and complications of the series.
Management of the periprosthetic fractures of the series.
| Case | Type | Procedure | Approach | Surgery | Complications |
|---|---|---|---|---|---|
| A | C | ORIF | Posterior | Double plate through posterior and medial | |
| B | B | ORIF | Anterolateral | 1st OP: lateral plate2nd OP: Double plate at 90°, lateral and anterior, +3 cortical strips and cerclage wire | Refracture in RHBIn consolidation phase |
| C | C | ORIF | Anterolateral | Double lateral and medial plate | |
| D | C | ORIF | Posterior | Lateral plate | |
| E | B | CRIF | Transdeltoid | Removal of prosthesis and intramedullary nailing of fracture | |
| F | C | ORIF | Posterior | Posterior plate | Temporary radial paralysis |
| G | B | PR | Deltopectoral | Prosthetic salvage with longer stem | |
| H | C | ORIF | Anterolateral | Double lateral and anterior plate | |
| I | C | ORIF | Posterior | Posterior plate | Temporary radial paralysis |
| J | C | ORIF | Anterolateral | Anterior plate |
ORIF: open reduction and internal fixation; CRIF: closed reduction and internal fixation; PR: prosthetic revision.
Periprosthetic humeral fracture is a rare condition, and we found limited evidence in the current literature on treatment. The therapeutic options depend on several factors, such as the location of the fracture, the stability of the prosthesis, bone quality, previous functional status and the different associated comorbidities. Generally, displaced periprosthetic fractures and loosened prostheses should be treated surgically.2,3,6,9–16 If the periprosthetic fracture is stable, minimally displaced and does not compromise the stability of the prosthesis, conservative treatment could be indicated.17–20
There has been an increase in recent years in the indications for partial or total shoulder arthroplasty, either as a result of a complex fracture of the proximal humerus or as a treatment for a degenerative condition.1
There are other factors that may be affecting the increase in the incidence of periprosthetic fractures, such ageing of the population and the greater functional demands of these patients. Thus, an increase in periprosthetic fractures in general is to be expected, and therefore also in those affecting the proximal humerus.1,21
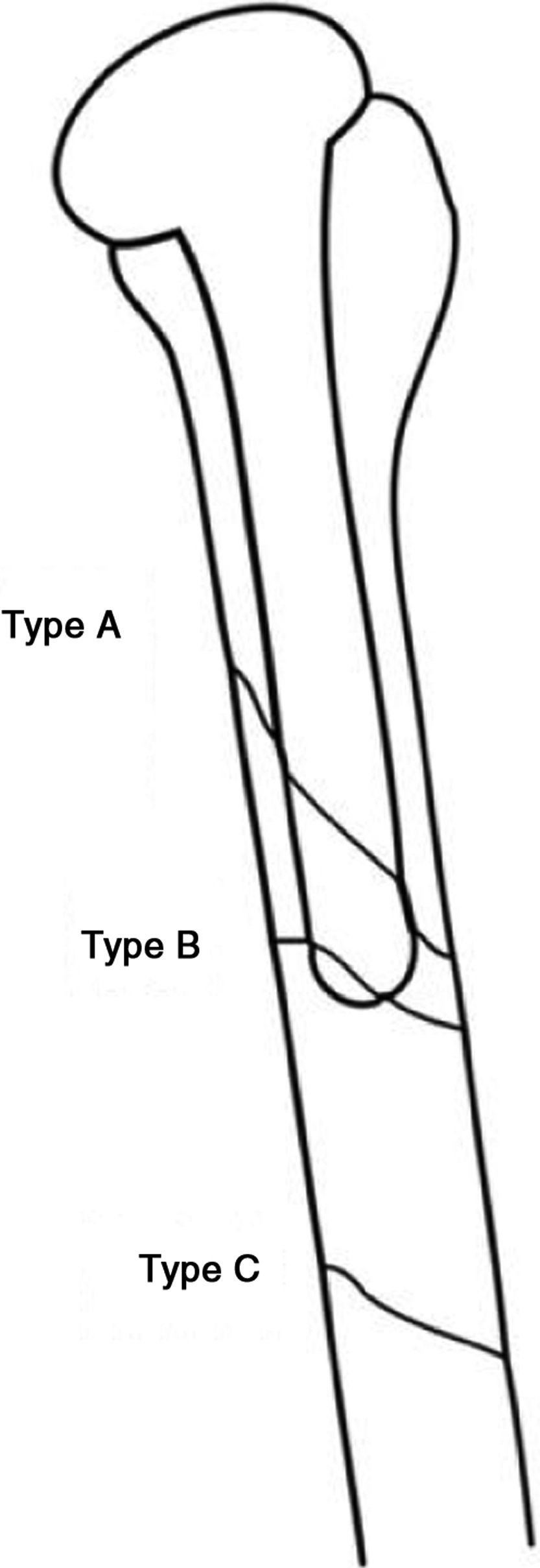
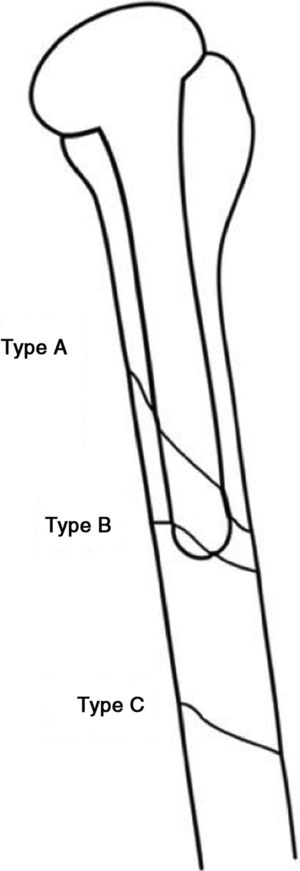
Periprosthetic fractures of the proximal humerus were classified in 1995 by Wright and Cofield6 into 3 types, as shown in Fig. 3.
Diagram of the types of periprosthetic fractures according to Wright and Cofield.6
The treatment of these types of fractures is a challenge for the orthopaedic surgeon. When making a therapeutic decision for these patients it is necessary to assess the type of fracture, functional demand, previous pain, the patient's comorbidity, the stability of the prosthesis and the bone stock.
Orthogonal projection radiography is necessary to determine the characteristics of the fracture line and type, as well as to assess possible loosening of the prosthesis. Therefore, it is advisable to compare them with previous X-rays to search for signs of loosening. It may occasionally be necessary to perform computerised tomography (CT) to identify fracture lines that are not visible on X-ray.
Depending on the variables mentioned above, orthopaedic treatment, osteosynthesis by open reduction (ORIF) or minimally invasive plate osteosynthesis (MIPO) or revision of the arthroplasty may be indicated.
Orthopaedic treatment would be indicated in patients with high comorbidity and low functional demand, in whom the surgical risk would outweigh the benefit of the intervention. In stable fractures, conservative treatment by means of brace type orthosis and sling is indicated.18,19,22 Weekly follow-up is recommended in the first month with clinical and radiographic evaluation. After the first month, follow-up can be monthly.
There is no consensus in the literature on the approach to be taken for this type of fracture. The most used approaches both in the literature and in our series were the posterior and the extended deltopectoral (anterolateral).
In our series, for type-B fractures, fractures at the tip of the stem, we chose to place the patient in a beach chair position to perform an extended deltopectoral approach, which allows visualisation of the fracture site; if necessary, the approach can be extended distally to locate the radial nerve and avoid damage. For type-B fractures, fractures distal to the stem tip and therefore more distal to the humerus, we always use posterior approaches, which allow us good reduction of the fracture with good control of the radial and ulnar nerve.
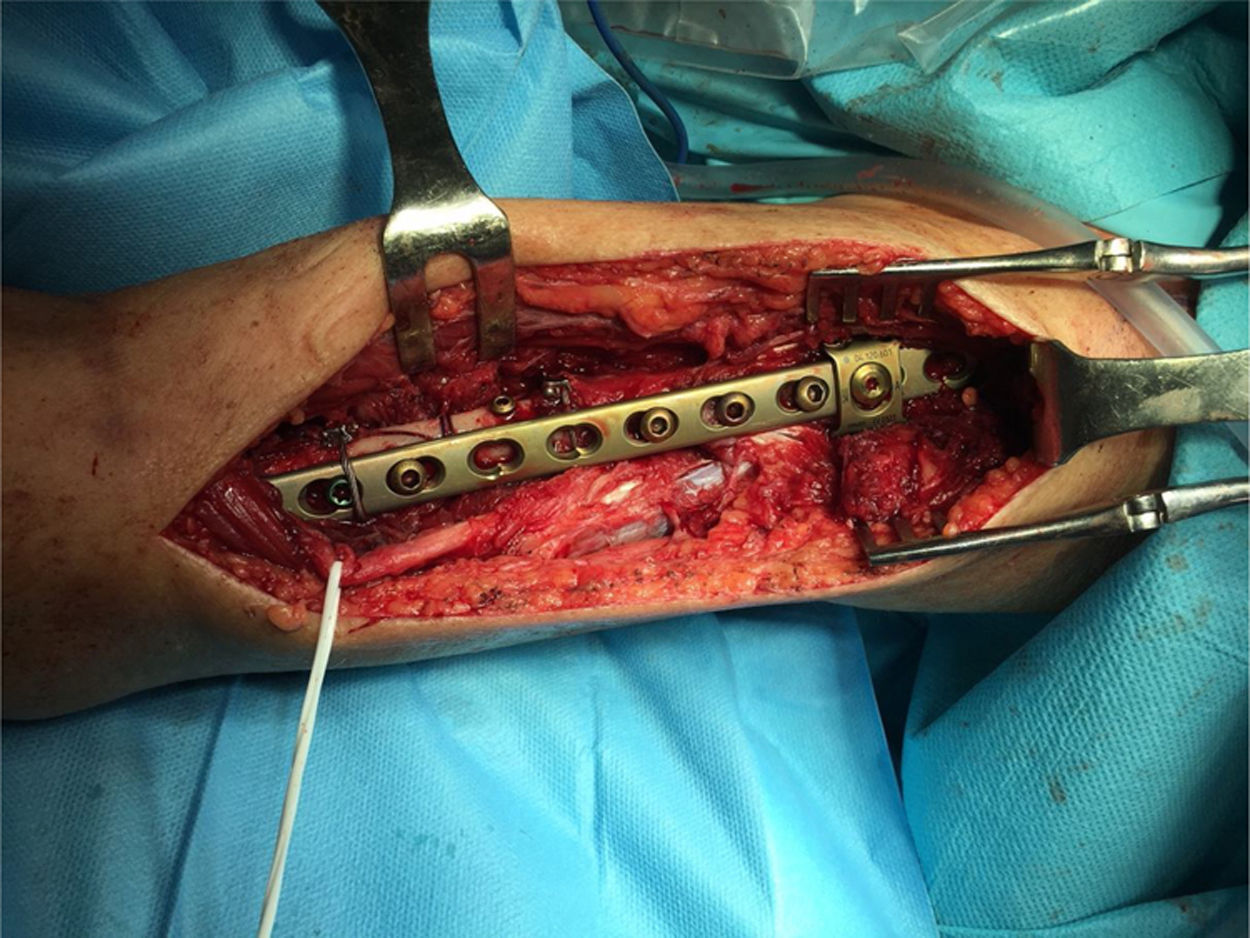
With regard to ORIF, there are different therapeutic options: screwed plates of 4.5mm in the most distal portion and fixed with cerclage wires in the proximal portion, plates fixed with unicortical screws in the proximal region, blocked plates or plates specifically designed for use in periprosthetic fractures, which allow the placement of screws at different degrees of angulation, thus avoiding the stem of the prosthesis. The use of interfragmentary screws can assist in reduction and subsequent fixation with the plate. It is recommended that osteosynthesis be performed with a sufficient number of cortices on each side of the fracture; in the humerus, at least 6 cortices are recommended, but this is not always possible, so we sometimes increase stability with cerclage wires, or with plates and screws specifically designed for this type of fracture.
The literature advocates osteosynthesis with a plate screwed distally with 4.5mm bicortical screws and mixed fixation with cerclage wires, unicortical screws and/or, if the plate allows it, variable angle screws to avoid the stem (Figs. 4 and 5).
The quality of the bone will be assessed intraoperatively. In the event that the patient presents marked osteopenia or insufficient bone stock, it may be necessary to provide a cortical structural allograft to improve the stability of the osteosynthesis.16
Kurowicki et al.16 describe a series of 5 patients with type B periprosthetic fractures who were treated with ORIF using the extended deltopectoral approach, performing osteosynthesis using a bicortical screwed plate at the distal level and mixed fixation at the proximal level with cerclage wires and unicortical screws at the proximal level, with excellent results (100% union); only one patient presented a complication: surgical wound infection.
Cerclage wires can damage periosteal vascularisation, bearing in mind that endosteal vascularisation is already impaired by the placement of the prosthesis, and therefore their use in periprosthetic fractures should only be as strictly necessary. They are often necessary as a provisional method of stabilisation, and if possible, it is recommended that they be removed after osteosynthesis with plate, if stability is not affected. In addition, cerclage wires may increase the risk of iatrogenic neurovascular injury. There is considerable controversy in the current literature about the use of braces in this type of fracture.23
One of the most relevant data in the series we describe is that the patients experienced a worsening of limb function, measured on 2 scales: the UCLASS and the Quick-DASH. A decrease of 10.7 points was observed on the UCLASS and an increase of 27.3 points on the Quick-DASH, comparing the situation before the fracture and the situation at the end of follow-up (Table 3). In addition, an increase in pain of 2.1 points on the VAS scale was confirmed. We observed a decrease in shoulder joint balance, with a loss of 23° in anterior flexion, 21° in abduction, 13° in internal rotation and 16° in external rotation. However, these results are not consistent with those published, which may be due to the fact that most patients (8 out of 10) underwent the arthroplasty as a consequence of a complex fracture of the proximal humerus, while in the other series there were a greater number of patients with rheumatic and arthritic processes in whom a total or inverted arthroplasty had been placed. On the other hand, these studies included intraoperative fractures, which often have little displacement and may have a better prognosis. In any case, it is difficult to justify that limb function does not suffer after a periprosthetic fracture in an older patient who is likely to fail to complete the rehabilitative treatment needed to obtain the best possible result.
Data from the periprosthetic fracture series.
| Case | Follow-up | VASpre | VASpost | UCLApre | UCLApost | QDpre | QDpost | Satisfaction |
|---|---|---|---|---|---|---|---|---|
| A | 9 | 2 | 3 | 25 | 11 | 34.1 | 68.2 | Satisfied |
| B | 13 | 0 | 10 | 27 | 8 | 45.0 | 81.8 | Dissatisfied |
| C | 24 | 3 | 3 | 24 | 13 | 27.3 | 70.5 | Dissatisfied |
| D | 87 | 3 | 4 | 25 | 10 | 34.1 | 70.5 | Dissatisfied |
| E | 80 | 0 | 2 | 24 | 8 | 27.3 | 68.2 | Satisfied |
| F | 12 | 2 | 3 | 28 | 21 | 34.1 | 54.5 | Satisfied |
| G | 6 | 1 | 3 | 29 | 24 | 22.7 | 31.8 | Satisfied |
| H | 6 | 2 | 4 | 24 | 13 | 50.0 | 68.2 | Dissatisfied |
| I | 9 | 5 | 7 | 18 | 12 | 65.9 | 86.4 | Dissatisfied |
| J | 6 | 7 | 7 | 14 | 11 | 70.5 | 84.1 | Dissatisfied |
| Mean | 25.1 | 2.5 | 4.6 | 23.8 | 13.1 | 41.1 | 68.4 | 4/6 |
VASpost: visual analogue scale at the end of follow-up; VASpre: visual analogue scale prior to the fracture; QDpost: Quick-Dash at the end of follow-up; QDpre: Quick-Dash score prior to the fracture; Follow-up in months; UCLApost: UCLA Shoulder Score at the end of follow-up; UCLApre: UCLA Shoulder Score prior to the fracture.
Of the 12 papers on periprosthetic fractures reviewed, only 4 (Wright y Cofield,6 Worland et al.,24 Kumar et al.3 and Sewell et al.25) describe a loss of joint balance after the fracture, and 3 other publications (Campbell et al.22, Andersen et al.11, García-Fernández et al.9) do not refer to the final joint balance situation after treating the fracture. The rest of the papers refer to shoulder joint balance results similar to those presented by the patients prior to the fracture.
In 6 articles the patients were given functional tests after treatment of the fracture, but none of them compare it with the patients’ situation before the fracture, and therefore there is no possibility of establishing any type of comparison.
With regard to pain, only 5 articles reported that the situation was similar to that before the fracture: few patients presented pain, and when they did, it was mild. These data are not comparable with those of this study, in which the 10 patients presented pain: 5 mild, 4 moderate and one patient with severe pain. The latter is the patient who suffered 2 fractures in the same humerus with an interval of 5 months and who underwent 2 surgeries in a short period of time, his situation is therefore exceptional.
In total, 138 periprosthetic fractures were recorded in the 12 papers: 109 were treated surgically and 29 orthopaedically. The average radiographic consolidation time, for both treatments, was similar: 6.5 months for those treated orthopaedically and 6.1 months for those treated surgically. The patients in our series achieved a similar consolidation time: an average of 6.2 months after the operation. The main data from the articles of the systematic review are presented in Tables 4 and 5.
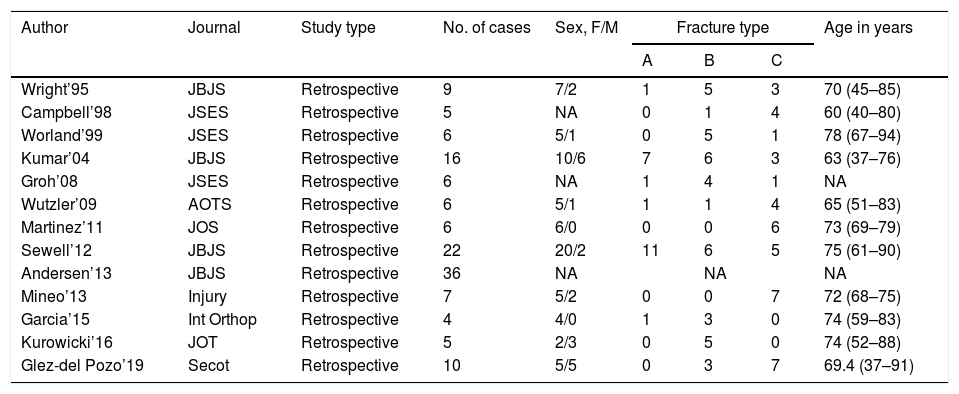
Data from the literature review.
| Author | Journal | Study type | No. of cases | Sex, F/M | Fracture type | Age in years | ||
|---|---|---|---|---|---|---|---|---|
| A | B | C | ||||||
| Wright’95 | JBJS | Retrospective | 9 | 7/2 | 1 | 5 | 3 | 70 (45–85) |
| Campbell’98 | JSES | Retrospective | 5 | NA | 0 | 1 | 4 | 60 (40–80) |
| Worland’99 | JSES | Retrospective | 6 | 5/1 | 0 | 5 | 1 | 78 (67–94) |
| Kumar’04 | JBJS | Retrospective | 16 | 10/6 | 7 | 6 | 3 | 63 (37–76) |
| Groh’08 | JSES | Retrospective | 6 | NA | 1 | 4 | 1 | NA |
| Wutzler’09 | AOTS | Retrospective | 6 | 5/1 | 1 | 1 | 4 | 65 (51–83) |
| Martinez’11 | JOS | Retrospective | 6 | 6/0 | 0 | 0 | 6 | 73 (69–79) |
| Sewell’12 | JBJS | Retrospective | 22 | 20/2 | 11 | 6 | 5 | 75 (61–90) |
| Andersen’13 | JBJS | Retrospective | 36 | NA | NA | NA | ||
| Mineo’13 | Injury | Retrospective | 7 | 5/2 | 0 | 0 | 7 | 72 (68–75) |
| Garcia’15 | Int Orthop | Retrospective | 4 | 4/0 | 1 | 3 | 0 | 74 (59–83) |
| Kurowicki’16 | JOT | Retrospective | 5 | 2/3 | 0 | 5 | 0 | 74 (52–88) |
| Glez-del Pozo’19 | Secot | Retrospective | 10 | 5/5 | 0 | 3 | 7 | 69.4 (37–91) |
AOTS: Archives of Orthopaedic and Trauma Surgery; Int Orthop: International Orthopaedics journal; JBJS: The Journal of Bone and Joint Surgery; JOS: Journal of Orthopaedic Surgery; JOT: Journal of Orthopaedic Trauma; JSES: Journal of Shoulder and Elbow Surgery; NA: not available.
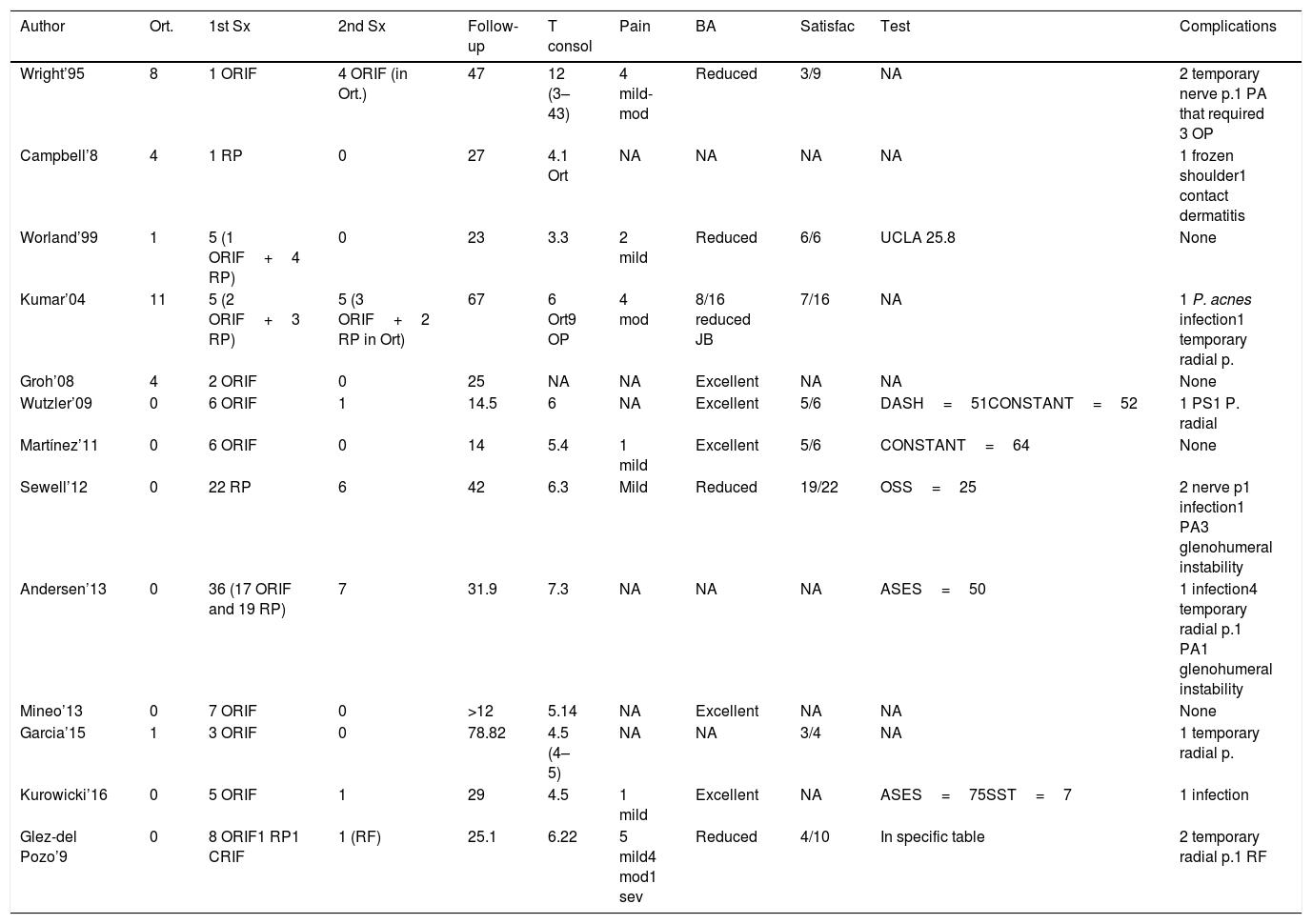
Summary of the literature on the management of periprosthetic humerus fracture.
| Author | Ort. | 1st Sx | 2nd Sx | Follow-up | T consol | Pain | BA | Satisfac | Test | Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| Wright’95 | 8 | 1 ORIF | 4 ORIF (in Ort.) | 47 | 12 (3–43) | 4 mild-mod | Reduced | 3/9 | NA | 2 temporary nerve p.1 PA that required 3 OP |
| Campbell’8 | 4 | 1 RP | 0 | 27 | 4.1 Ort | NA | NA | NA | NA | 1 frozen shoulder1 contact dermatitis |
| Worland’99 | 1 | 5 (1 ORIF+4 RP) | 0 | 23 | 3.3 | 2 mild | Reduced | 6/6 | UCLA 25.8 | None |
| Kumar’04 | 11 | 5 (2 ORIF+3 RP) | 5 (3 ORIF+2 RP in Ort) | 67 | 6 Ort9 OP | 4 mod | 8/16 reduced JB | 7/16 | NA | 1 P. acnes infection1 temporary radial p. |
| Groh’08 | 4 | 2 ORIF | 0 | 25 | NA | NA | Excellent | NA | NA | None |
| Wutzler’09 | 0 | 6 ORIF | 1 | 14.5 | 6 | NA | Excellent | 5/6 | DASH=51CONSTANT=52 | 1 PS1 P. radial |
| Martínez’11 | 0 | 6 ORIF | 0 | 14 | 5.4 | 1 mild | Excellent | 5/6 | CONSTANT=64 | None |
| Sewell’12 | 0 | 22 RP | 6 | 42 | 6.3 | Mild | Reduced | 19/22 | OSS=25 | 2 nerve p1 infection1 PA3 glenohumeral instability |
| Andersen’13 | 0 | 36 (17 ORIF and 19 RP) | 7 | 31.9 | 7.3 | NA | NA | NA | ASES=50 | 1 infection4 temporary radial p.1 PA1 glenohumeral instability |
| Mineo’13 | 0 | 7 ORIF | 0 | >12 | 5.14 | NA | Excellent | NA | NA | None |
| Garcia’15 | 1 | 3 ORIF | 0 | 78.82 | 4.5 (4–5) | NA | NA | 3/4 | NA | 1 temporary radial p. |
| Kurowicki’16 | 0 | 5 ORIF | 1 | 29 | 4.5 | 1 mild | Excellent | NA | ASES=75SST=7 | 1 infection |
| Glez-del Pozo’9 | 0 | 8 ORIF1 RP1 CRIF | 1 (RF) | 25.1 | 6.22 | 5 mild4 mod1 sev | Reduced | 4/10 | In specific table | 2 temporary radial p.1 RF |
ASES: American Shoulder and Elbow Score; JB: shoulder joint balance; Pain: number of patients with pain and grade of pain (mild, moderate and severe); NA: information not available; Ort: orthopaedic treatment; OSS: Oxford Shoulder Score; PA: pseudo-osteoarthritis; ORIF: open reduction and internal fixation; RF: refracture; RP: revision of prosthesis; Satisfac: number of satisfied patients of the total patients in the study; SST: Simple Shoulder Test; T consol: consolidation time in months; 1st Sx: first surgical treatment; 2nd Sx: secondary surgical treatment.
Of the 29 patients treated conservatively in the literature, 9 had to be operated subsequently, with delayed consolidation and misalignment being the main causes. This means that 31% of the patients initially treated conservatively had to be operated to achieve acceptable consolidation. On the other hand, of the 109 patients initially treated surgically, 16 cases had to be reoperated, which is 14%. In this series, only one patient (10%) had to be operated for a new fracture that occurred while they were doing their rehabilitation exercises.
Of the patients undergoing primary surgery, according to the literature, approximately 20% had complications. Neurological injury was the most frequent complication, in a total of 9 cases (8.2%). On 7 occasions they presented radial nerve paralysis and in 2 cases, axillary nerve paralysis. The second most frequent complication was glenohumeral instability in 4 patients (3.6%). Four cases of surgical wound infection were also described, comprising 3.6% of the total.
In the series presented, the most frequent complication was also radial nerve paralysis in 2 patients (20%), who had fully recovered by the end of the follow-up.
The other complication suffered by one patient was a new fracture that occurred while undergoing rehabilitation, 5 months after the surgery, which required a new intervention.
No cases of infection or glenohumeral instability occurred in our series, although in one case the option was to remove the prosthesis and place an intramedullary nail as treatment for the periprosthetic fracture. We opted for this solution since this was an elderly patient with Alzheimer's disease, great comorbidity and poor limb function.
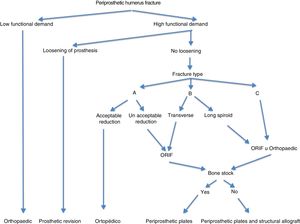
In light of the results and the surgical experience gained, we propose the algorithm shown in Fig. 6 to facilitate the management of periprosthetic humerus fractures.
ConclusionsProvided that the patient does not have excessive comorbidity, the data collected in the literature indicate that faced with a displaced periprosthetic fracture of the humerus with a non-loosened stem, the recommended treatment is to perform an osteosynthesis with a screwed plate of 4.5mm, either locked or otherwise. On the other hand, if the prosthesis has loosened, the indication is replacement of the prosthesis and placing a longer stem. Conservative treatment would be indicated in stable periprosthetic fractures that are not displaced or in more complex patients with comorbidities, for whom surgery is not indicated.
Periprosthetic humerus fractures are a rare entity and their management has not been standardised in routine practice.
Periprosthetic humerus fracture is a rare, serious complication that substantially worsens the patient's quality of life. Following a periprosthetic fracture, patients tend to have more pain, less mobility and poorer functionality of the limb.
FundingThe authors have received no financial payments or other benefits from any commercial entity in relation to the subject of this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: González del Pozo J, Andrés-Cano P, Belascoain Benítez E, Giráldez Sánchez MA, Cano-Luis P, Moreno Domínguez R, et al. Tratamiento quirúrgico de las fracturas periprotésicas de húmero y algoritmo de actuación. Rev Esp Cir Ortop Traumatol. 2020;64:213–222.