Proximal fibula malignant and locally aggressive benign bone tumors are uncommon and usually treat by surgery. Bloc resection of the knee can compromise knee stability due to the resection of the posterolateral ligament complex.
Material and methodsWe analyzed 28 consecutive patients treated for a proximal fibula bone tumor between 1980 and 2006 (osteosarcoma: 9, giant cell tumor: 9, Ewing sarcoma: 8 and chondrosarcoma: 2). Sixty-one percent were male and the median age was 21 years (range: 8–60). The mean follow-up was 86 months. The posterolateral complex was reinserted at tibial metaphyseal level. Patients were evaluated functionally using the Musculoskeletal Tumor Society scale (MSTS).
ResultsOverall survival rate was 89%, local recurrence rate was 11%, and secondary amputation rate was 6% at 7 years of median follow-up. The average MSTS score was 93%. Five patients had neurological complications. No patient experienced subjective instability or vascular insufficiency.
ConclusionsBloc resection of the proximal fibula for the treatment of aggressive or malignant primary bone tumors allowed us to obtain local tumor control, and overall survival rate for sarcomas of 89% at 7 years. The posterolateral ligament complex tibial reinsertion provided functional knee stability without major functional consequences in the medium term.
Los tumores óseos malignos o benignos localmente agresivos del tercio proximal del peroné son infrecuentes y generalmente su tratamiento es quirúrgico. Cuando se requiere una resección en bloque, la estabilidad de la rodilla puede comprometerse por afectación del complejo posterolateral.
Material y métodosSe analizaron 28 pacientes operados de manera consecutiva por un tumor óseo en el tercio proximal de peroné entre los años 1980 y 2006 (osteosarcoma: 9, TCG: 9, sarcoma de Ewing: 8 y condrosarcoma: 2). El 61% eran varones y la edad media fue de 21 años (rango: 8–60). El seguimiento promedio fue de 86 meses. El complejo posterolateral fue reinsertado a nivel de la metáfisis tibial. Los pacientes fueron evaluados funcionalmente con la escala Musculoskeletal Tumor Society (MSTS).
ResultadosLa supervivencia global fue del 89%, con un índice de recidiva local del 11% y un porcentaje de amputaciones secundarias del 6% a los 7 años de seguimiento promedio. El resultado promedio del MSTS fue del 93%. Cinco pacientes sufrieron secuelas neurológicas, 3 de tipo permanente. Ningún paciente sufrió inestabilidad subjetiva ni insuficiencia vascular.
ConclusionesLa resección en bloque del peroné proximal en el tratamiento de los tumores óseos agresivos o malignos depara un buen control local de la enfermedad y una supervivencia a los 7 años, en los casos malignos, del 89%. La reinserción del complejo posterolateral a nivel tibial supone una buena estabilidad de la rodilla, sin secuelas funcionales a largo plazo.
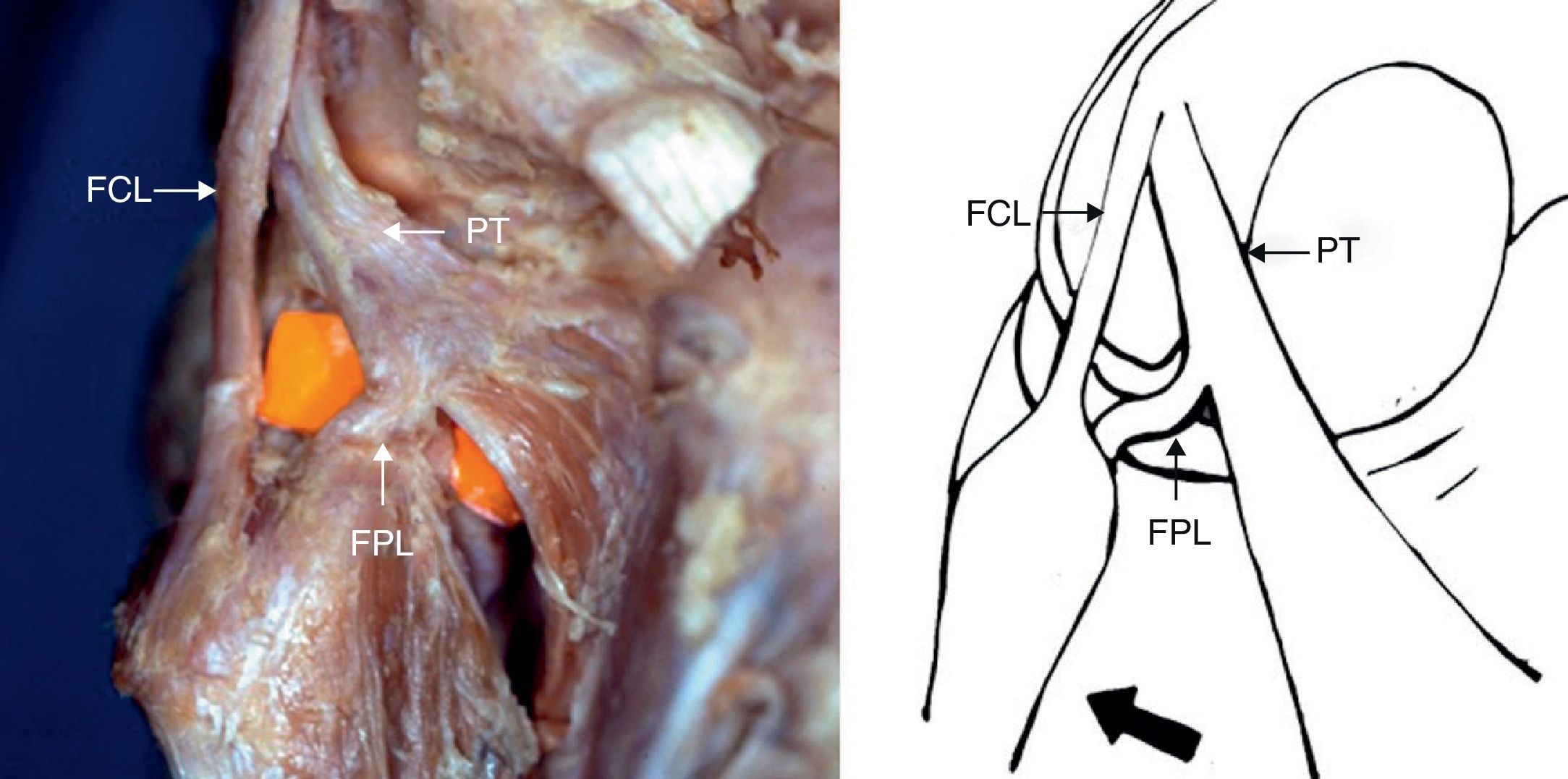
Primary bone tumors in the fibula are infrequent, representing only 2.5% of all bone tumors, with osteosarcoma being the most prevalent.1–4 Anatomically, the proximal end of the fibula is closely related to the posterolateral ligamentous complex, as well as the vascular-nervous elements of the knee. The structures which comprise the posterolateral complex play an important stabilizing role (Fig. 1), preventing posterior translation, varus deviation and external rotation of the tibia.5,6 The treatment of locally aggressive or malignant tumors of the proximal end of the fibula requires extensive or radical resections, in order to obtain adequate postoperative margins. This may compromise knee stability, vascularization and innervation of the affected limb. The published literature includes reports of a fibular nerve palsy index ranging between 20 and 57%.2,7 The aim of this study was to analyze the clinical and oncological evolution, as well as the function and stability of the knee, following block resection of aggressive and malignant primary bone tumors located in the proximal end of the fibula (Fig. 2).
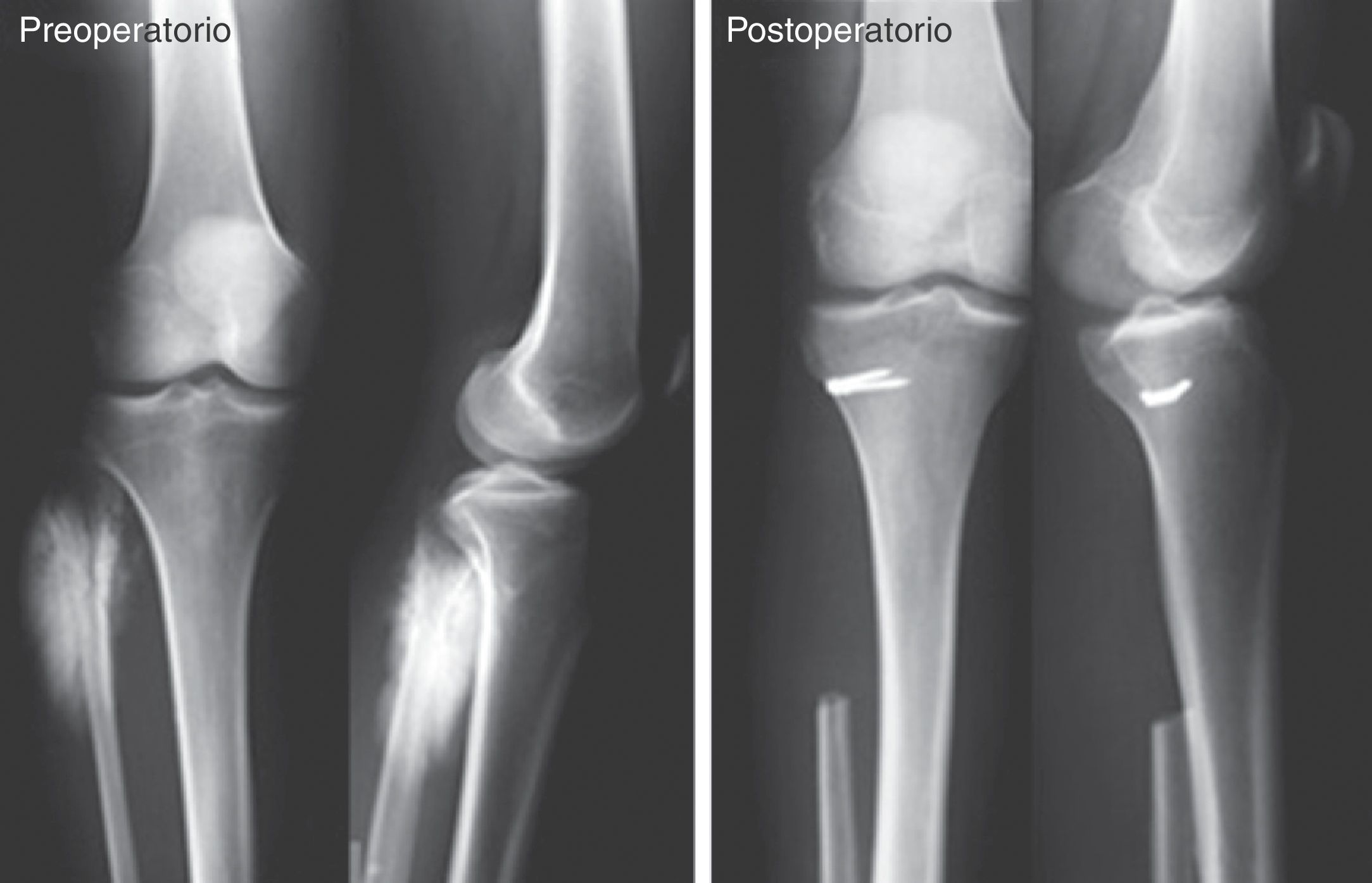
We performed a retrospective search in our oncology database based on prospective criteria between October 1980 and March 2006. We identified a total of 56 patients with primary bone tumors of the fibula. Of these, 28 affected the proximal third, were malignant or locally aggressive benign tumors and were treated through surgical block resection, so we included them in our analysis. A total of 17 patients (61%) were male and the mean age of the series at the time of diagnosis was 21 years (range: 4–60 years). The mean follow-up period was 86 months (range: 12–256 months) without any loss of patients. The surgical treatment performed in all cases involved block resection of the proximal fibula. A total of 11 cases underwent Malawer type 1 resections (marginal resections), whilst another 17 cases underwent type II resections (broad intracompartmental).7 The vascular-nervous and ligamentous elements were preserved, provided that there was no tumor involvement thereof. In cases were the posterolateral ligamentous complex was preserved, it was reinserted in the lateral side of the proximal tibial metaphysis using staples. Fixation was performed with the knee at 30° flexion.8
All patients were evaluated before surgery through knee radiographs in anteroposterior and lateral projections, and through computed tomography and magnetic resonance imaging from 1992. A preoperative puncture biopsy was performed in all cases and the diagnosis was confirmed by histopathological examination. The 28 tumors in the proximal third of the fibula included 9 osteosarcomas, 9 giant cell tumors, 8 Ewing sarcomas and 2 chondrosarcomas. The 19 bone sarcomas were staged according to the Enneking classification, with the following results: 1 grade 1A, 1 grade 1B and 17 grade 2B. For giant cell tumors we used the classification described by Campanacci, with 4 being grade 2 and 5 grade 3.9,10 A total of 8 patients diagnosed with osteosarcoma and 6 with Ewing sarcoma received preoperative and postoperative chemotherapy.
The use of an extension splint was indicated for 3 weeks and passive flexion and extension exercises were started from the second postoperative day. Therapy progressed to active movement from the third week and progressive load from the sixth.
A clinical and radiographic evaluation was performed every 3 months during the first 2 years and every 6 months after the second year. Knee stability was assessed through stress radiographs (in forced varus) in an anteroposterior projection and with the knee at 30° flexion. Instability was classified into 3 grades: grade 1: an opening of the joint between 1 and 5mm; grade 2: an opening between 5 and 11mm and grade 3: an opening greater than 11mm.11 All radiographs were assessed by an independent observer.
For the functional assessment we used the Musculoskeletal Tumor Society (MSTS) scale.12 The survival of patients with malignant tumors was determined according to the Kaplan–Meier method.13
ResultsThe mean survival of the 19 patients with malignant tumors at 7 years follow-up was 89±10% (±2 SD). A total of 3 patients presented distant disease at the time of death.
The incidence of local recurrences was 11% (n=3) and all cases were patients with a histological diagnosis of osteosarcoma (2 conventional central and 1 parosteal). Two patients underwent a new resection and the remaining patient a supracondylar amputation.
Postoperative stability was assessed in 22 patients (79%) of our total series, resulting in 11 (50%) stable knees, 9 (41%) unstable grade 1 and 2 (9%) unstable grade 2. Patients with grade 1 instability did not require treatment because their instability was subclinical, whereas those suffering grade 2 instability were treated conservatively with external orthoses.
A total of 26 out of the 28 patients in the series were assessed with the MSTS functional scale. Two cases were excluded from this assessment because they died from the disease before the control took place. The mean score was 28/30 points, with 20 excellent results, 4 regular and 2 poor. All presented a mobility range comparable to the contralateral knee, with no statistically significant differences being observed (P>.05).
We recorded 5 patients who suffered postoperative neurological complications, 3 permanent and 2 temporary. No patient suffered vascular insufficiency, despite 4 patients undergoing ligation of the anterior tibial artery. There were no cases of wound complications or infections. There were no reported episodes of postoperative deep vein thrombosis.
DiscussionThe incidence of primary bone tumors at the level of the fibula is low.1 Intracompartmental block resections of the proximal third with involvement of the posterolateral complex present a reconstructive challenge for oncological orthopedic surgeons.9 The results of anatomical studies indicate that the fibular collateral ligament, the popliteal-fibular ligament and the popliteal tendon are crucial for the posterolateral stability of the knee, so their repair is essential. However, the reconstruction of 2 of those 3 structures (fibular collateral ligament and popliteal-fibular ligament) is sufficient to restore stability, thus eliminating the need for extensive dissections at the level of the tibia to also reconstruct the distal insertion of the popliteal tendon.6 Although there is ample evidence regarding the results of the reconstruction of the posterolateral complex in trauma injuries, the number of publications referred to reconstruction after oncological resection is limited. In 2012, Matthew et al. presented a series of primary bone sarcomas of the proximal third of the fibula treated with wide resection and reconstruction of the posterolateral ligament complex, reporting good functional results and good stability of the knee.2
Both Bozkurt et al.14 and Aponte-Tinao6 have demonstrated the importance of the proximal tibiofibular joint and posterolateral complex for the stability of the knee joint in cadaver studies. Therefore, if the proximal fibula is resected, the ligamentous and tendinous structures must be reinserted in order to preserve that stability.15 Otherwise, the resulting instability would imply potential long-term degenerative changes in these patients, who are generally young at the time of treatment. In this series, the reconstruction technique used for the posterolateral complex has proven to be reproducible and provide good postoperative knee stability. The complications described and their impact were similar to those published in the literature with other reconstructive techniques, with neurological complications being the most prevalent.2,15 Moreover, the functional results obtained were very satisfactory, although the assessment scale used was designed for cancer patients so the parameters it evaluates are different from other scales used for knee surgery without tumor disease. We consider this to be one of the limitations of our study, along with the retrospective design and the number of patients. Nevertheless, it is a homogeneous series with an infrequent disease which is scarcely reported in the literature.12
In conclusion, block resection of the proximal fibula for the treatment of aggressive or malignant bone tumors offers good local disease control and survival at 7 years, reaching 89% in malignant cases. Reinsertion of the posterolateral complex at the level of the tibia provides good knee stability without long-term functional sequelae.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Farfalli GL, Albergo JI, Ayerza MA, Muscolo DL, Aponte-Tinao LA. Tratamiento quirúrgico de los tumores malignos y localmente agresivos del tercio proximal del peroné. Resultados oncológicos y evaluación funcional. Rev Esp Cir Ortop Traumatol. 2014;58:212–216.