Hip fracture usually occurs in frail elderly patients and is associated with an important morbi-mortality in the first year. The objective of the study is to describe the prognostic factors that would allow maintaining functionality at 12 months.
MethodFrom June 1, 2010 to May 31, 2013, all patients older than 69 years with hip fracture due to bone fragility admitted to the Geriatric Acute Unit of our hospital were included. We define as functional maintenance those patients who have lost between 0 and 15 points in the Barthel Index with respect to the previous to the fracture. Prospective study of bivariate data analysis for related and multivariate prognostic factors for predictive predictors.
Results271 patients were included, of them, 146 (54.8%), maintained functionality at 12 months and 122 (45.2%) no. Patients who maintain functional status are younger: average age 83.4 vs 85.80 years (p=.002); with better scores in the indexes of: Lawton prior to fracture 4.42 vs 2.40 (p<.001) and Barthel at discharge 34.2 vs. 27.1 (p=.002). There are also differences in the score of the “Geriatric Dementia Scale” 2.59 vs. 3.13 (p=.009), in the score of the “American Society Anesthesiologist”<II 62.2% vs 37.8% (p=.006) and have presented less delirium during hospitalisation 4.7% vs 35.3% (p=.002). In the multivariate analysis they maintained statistical significance, age OR: 1.044 (95% CI: 1.002-1.088) (p=.04) and the Lawton Index OR: 0.869 (95% CI: 0.804-0.940) (p<.001).
ConclusionsPrognostic factors of functional maintenance at 12 months are age and the ability to perform instrumental activities of daily life.
La fractura de cadera suele ocurrir en pacientes frágiles de edad avanzada y va asociada a una importante morbimortalidad al al primer año. El objetivo del estudio es describir los factores pronósticos que permitirían mantener la funcionalidad a los 12 meses.
MétodoDesde el 1 de junio de 2010 hasta el 31 de mayo de 2013 se han incluido a todos los pacientes mayores de 69 años con fractura de cadera por fragilidad ósea ingresados en la Unidad Geriátrica de Agudos de nuestro hospital. Definimos como mantenimiento funcional a aquellos pacientes que han perdido entre 0-15 puntos en el índice de Barthel respecto al previo a la fractura. Estudio prospectivo de análisis de datos bivariado para los factores pronósticos relacionados y multivariado para los factores pronósticos predictores.
ResultadosSe incluyen 271 pacientes, de ellos, 146 (54,8%), mantienen funcionalidad a los 12 meses y 122 (45,2%) no. Los pacientes que mantienen el estado funcional son más jóvenes: edad media 83,4 vs. 85,80 años (p=0,002); con mejores puntaciones en los índices de: Lawton previo a la fractura 4,42 vs. 2,40 (p<0,001) y Barthel al alta 34,2 vs. 27,1 (p=0,002). También hay diferencias en la puntuación de la «Geriatric Dementia Scale» 2,59 vs. 3,13 (p=0,009), en la puntuación de la «American Society Anesthesiologist»<II 62,2 vs. 37,8% (p=0,006) y han presentado menos delirium durante la hospitalización 4,7 vs. 35,3% (p=0,002). En el análisis multivariado han mantenido significación estadística, la edad OR: 1,044 (IC 95%: 1,002-1,088) (p=0,04) y el índice de Lawton OR: 0,869 (IC 95%: 0,804-0,940) (p<0,001).
ConclusionesLos factores pronósticos de mantenimiento funcional a los 12 meses son la edad y la capacidad de realizar actividades instrumentales de la vida diaria.
Hip fractures are the fragility fractures with the greatest impact on patients and constitute some of the most important socio-health problems in Western countries.1 Of all osteoporotic fractures, approximately 20% are located in the femur. They usually occur in the later stages of life, 80 being the average age of onset. Hip fractures have an in-hospital mortality rate of 4%-8%.2,3 After one year this mortality can reach 25%, and even increase to 40% in the following 2 years.4–9 In addition, hip fracture is a determining factor of functional impairment which often precipitates hospitalisation of these patients and entails high economic costs.4,5 One of the objectives of orthogeriatrics is to ensure that patients, following a fracture of the femur, are able to return to their habitual home and preserve the maximum degree of physical and cognitive independence for as long as possible.
For this reason, the objective of our study was to identify the prognostic factors that allow functional maintenance at 12 months after a hip fracture due to bone fragility (HFBF), after these patients have been attended in an acute geriatric unit.
Materials and methodsStudy design and participantsThis is a prospective study performed in the Hospital de Igualada, with a catchment area of 118467 inhabitants corresponding to the Region of la Anoia (Barcelona). The inclusion criteria were: patients over 69 years of age admitted from home, admitted to the acute geriatric unit from the emergency department within a period of 36 months, and who gave their informed consent (in the event of dementia, that of the responsible relative and/or guardian) to participate in this study.
The patients in the sample, recruited prospectively, received an intervention for which the care management of the entire process is the responsibility of the interdisciplinary geriatric team. This intervention is framed within the Therapeutic Hip Fracture Guideline of the Hospital de Igualada, which has been described previously10 and has now been updated in relation to the references; the most relevant aspects have not changed with respect to the reference of Duaso et al.10 such as: emergency department stay <3h, surgical intervention before 48h and direct admission from the emergency department to the acute geriatric unit, among others.
The following variables were collected: demographic (sex, age, marital status, place from which they were admitted, destination on discharge), functionality prior to admission and on discharge (Barthel index [BI],11 Lawton and Brody index,12 gait pattern prior to admission and on discharge (Functional Ambulation Classification),13 cognitive status (Geriatric Dementia Scale (GDS)14; Charlson comorbidity index,15 biochemical parameters (kidney function, TSH, calcium, proteins, albumin). And data on surgical waiting time, fracture site, anaesthetic risk (American Society Anesthesiologist classification [ASA])16; length of hospital stay, presence or otherwise of delirium during admission, complications during admission (infections, anaemia with transfusion requirement, hydroelectrolytic disturbances, cardiovascular decompensation), sensory disturbances, and the presence of medications potentially associated with falls.
To determine the prognostic factors for maintaining functionality at 12 months, we divided the sample into 2 groups; a first group of functional maintenance at 12 months that we considered to be the patients who lost between 0 and 15 points on the BI before the fracture, and a second group termed functional loss at 12 months: patients who had lost 20 or more points on the BI compared to their BI prior to the fracture.
This study was approved by the Bellvitge Hospital Ethics Committee (PR197/13).
Statistical analysisA bivariate statistical analysis was carried out to identify the factors related to the variables studied. In this analysis, the Mann-Whitney U test was used to study the relationship between a numerical and a categorical variable. The Chi-square test was used to study the relationship between categorical variables, with the correction of the Fisher test. The variables that showed a statistically significant relationship in the bivariate analysis were included in a multivariate analysis model of binary logistic regression, and the variables that did not show statistical significance were eliminated (provided they were not confounding factors) to obtain an optimal prediction model of the variables studied. The discriminatory capacity of the model was evaluated with the area under the curve and the calibration of the model with the Hasmer-Lemeshow test. In all the analyses, p values ≤.05 were considered statistically significant.
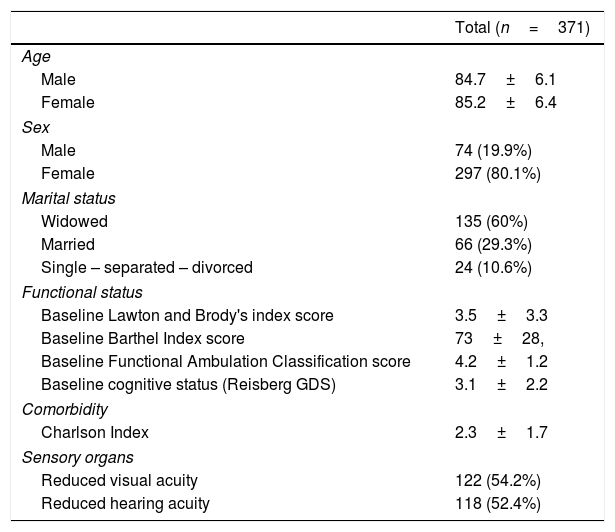
ResultsDuring the study period, 371 patients were admitted with a diagnosis of HFBF; of whom 5 (1.3%) died during hospital admission. A total of 366 patients discharged from the acute geriatric unit were analysed. The 95 (25.9%) deaths that occurred in the 12-month follow-up were excluded. The initial general characteristics of the 371 patients, finally included in the initial study population, can be found in Table 1.
Baseline characteristics.
| Total (n=371) | |
|---|---|
| Age | |
| Male | 84.7±6.1 |
| Female | 85.2±6.4 |
| Sex | |
| Male | 74 (19.9%) |
| Female | 297 (80.1%) |
| Marital status | |
| Widowed | 135 (60%) |
| Married | 66 (29.3%) |
| Single – separated – divorced | 24 (10.6%) |
| Functional status | |
| Baseline Lawton and Brody's index score | 3.5±3.3 |
| Baseline Barthel Index score | 73±28, |
| Baseline Functional Ambulation Classification score | 4.2±1.2 |
| Baseline cognitive status (Reisberg GDS) | 3.1±2.2 |
| Comorbidity | |
| Charlson Index | 2.3±1.7 |
| Sensory organs | |
| Reduced visual acuity | 122 (54.2%) |
| Reduced hearing acuity | 118 (52.4%) |
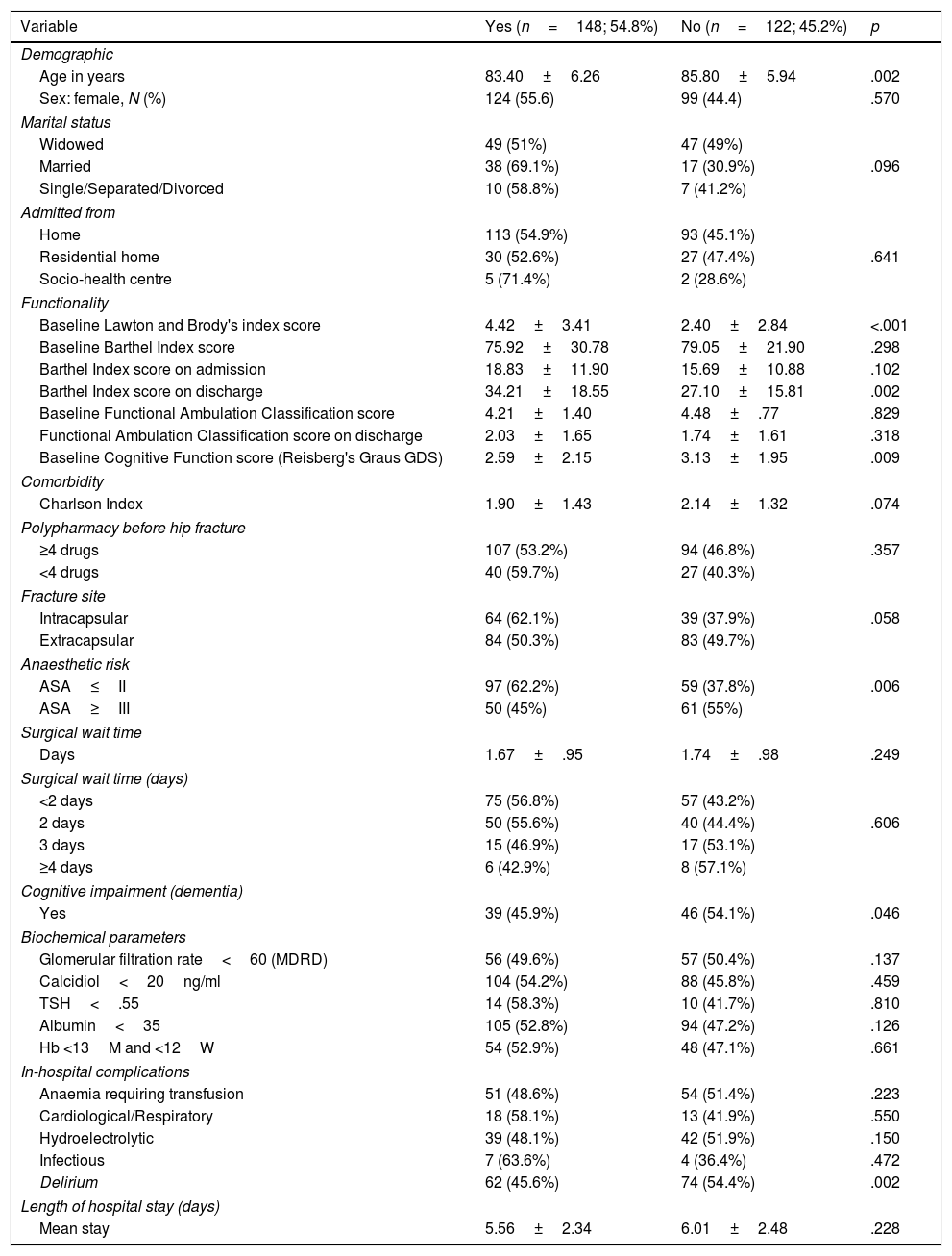
Functionality was maintained in 148 (54.8%) patients with a mean age of 83.40 years and a 55.6% proportion of females, conversely, it was not maintained in 122 patients (45.2%) with a mean age of 85.80 years and a proportion of females of 44.4%. The comparison of the 2 groups is shown in Table 2. Factors related to maintenance of functionality at 12 months include lower age (p=.002); a better Lawton and Brody index score (p<.001); a better BI score (p=.002); an improved GDS score (p=.009); lower surgical risk according to the ASA classification (p=.006); no delirium during admission (p=.002) and no diagnosis of dementia prior to fracture (p=.046).
Factors related to maintenance of functionality at 12 months.
| Variable | Yes (n=148; 54.8%) | No (n=122; 45.2%) | p |
|---|---|---|---|
| Demographic | |||
| Age in years | 83.40±6.26 | 85.80±5.94 | .002 |
| Sex: female, N (%) | 124 (55.6) | 99 (44.4) | .570 |
| Marital status | |||
| Widowed | 49 (51%) | 47 (49%) | |
| Married | 38 (69.1%) | 17 (30.9%) | .096 |
| Single/Separated/Divorced | 10 (58.8%) | 7 (41.2%) | |
| Admitted from | |||
| Home | 113 (54.9%) | 93 (45.1%) | |
| Residential home | 30 (52.6%) | 27 (47.4%) | .641 |
| Socio-health centre | 5 (71.4%) | 2 (28.6%) | |
| Functionality | |||
| Baseline Lawton and Brody's index score | 4.42±3.41 | 2.40±2.84 | <.001 |
| Baseline Barthel Index score | 75.92±30.78 | 79.05±21.90 | .298 |
| Barthel Index score on admission | 18.83±11.90 | 15.69±10.88 | .102 |
| Barthel Index score on discharge | 34.21±18.55 | 27.10±15.81 | .002 |
| Baseline Functional Ambulation Classification score | 4.21±1.40 | 4.48±.77 | .829 |
| Functional Ambulation Classification score on discharge | 2.03±1.65 | 1.74±1.61 | .318 |
| Baseline Cognitive Function score (Reisberg's Graus GDS) | 2.59±2.15 | 3.13±1.95 | .009 |
| Comorbidity | |||
| Charlson Index | 1.90±1.43 | 2.14±1.32 | .074 |
| Polypharmacy before hip fracture | |||
| ≥4 drugs | 107 (53.2%) | 94 (46.8%) | .357 |
| <4 drugs | 40 (59.7%) | 27 (40.3%) | |
| Fracture site | |||
| Intracapsular | 64 (62.1%) | 39 (37.9%) | .058 |
| Extracapsular | 84 (50.3%) | 83 (49.7%) | |
| Anaesthetic risk | |||
| ASA≤II | 97 (62.2%) | 59 (37.8%) | .006 |
| ASA≥III | 50 (45%) | 61 (55%) | |
| Surgical wait time | |||
| Days | 1.67±.95 | 1.74±.98 | .249 |
| Surgical wait time (days) | |||
| <2 days | 75 (56.8%) | 57 (43.2%) | |
| 2 days | 50 (55.6%) | 40 (44.4%) | .606 |
| 3 days | 15 (46.9%) | 17 (53.1%) | |
| ≥4 days | 6 (42.9%) | 8 (57.1%) | |
| Cognitive impairment (dementia) | |||
| Yes | 39 (45.9%) | 46 (54.1%) | .046 |
| Biochemical parameters | |||
| Glomerular filtration rate<60 (MDRD) | 56 (49.6%) | 57 (50.4%) | .137 |
| Calcidiol<20ng/ml | 104 (54.2%) | 88 (45.8%) | .459 |
| TSH<.55 | 14 (58.3%) | 10 (41.7%) | .810 |
| Albumin<35 | 105 (52.8%) | 94 (47.2%) | .126 |
| Hb <13M and <12W | 54 (52.9%) | 48 (47.1%) | .661 |
| In-hospital complications | |||
| Anaemia requiring transfusion | 51 (48.6%) | 54 (51.4%) | .223 |
| Cardiological/Respiratory | 18 (58.1%) | 13 (41.9%) | .550 |
| Hydroelectrolytic | 39 (48.1%) | 42 (51.9%) | .150 |
| Infectious | 7 (63.6%) | 4 (36.4%) | .472 |
| Delirium | 62 (45.6%) | 74 (54.4%) | .002 |
| Length of hospital stay (days) | |||
| Mean stay | 5.56±2.34 | 6.01±2.48 | .228 |
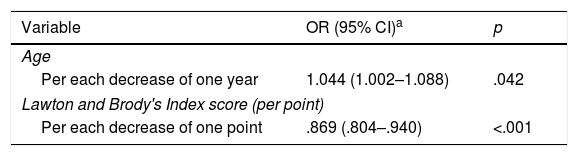
The variables that maintained their statistical significance in the multivariate analysis are younger age OR: 1.044 (95% CI: 1.002–1.088) (p=.042) and increased Lawton and Brody index score OR: .869 (95% CI: .804–.940) (p<.001), with a discrimination capacity of the AUC model (±95% CI): .658 (Table 3).
Predictive factors with maintenance of functionality at 12 months.
| Variable | OR (95% CI)a | p |
|---|---|---|
| Age | ||
| Per each decrease of one year | 1.044 (1.002–1.088) | .042 |
| Lawton and Brody's Index score (per point) | ||
| Per each decrease of one point | .869 (.804–.940) | <.001 |
CI: Confidence Interval; OR: Odds Ratio.
Discrimination capacity of the model, AUC (±95% CI): .658 (.594–.723).
Calibration of the model, Hosmer–Lemeshow test: p=.182.
The different studies of patients with HFBF use diverse and heterogeneous measures to determine functional maintenance. In addition, in these studies, functionality is not assessed over the same periods of time after the fracture, and neither are the same levels of previous functionality.17,18 This evidences a disparity of data and outcomes in relation to the maintenance of functionality. It has been considered that variations of 20 points on the BI relate to different health outcomes; including functional capacity.19,20 This is why we decided to choose this value as a benchmark when measuring the maintenance of functionality at 12 months following the HFBF, in the 271 patients studied overall.
It is important to highlight that functional maintenance is very largely due to an appropriate process of functional recovery after the fracture, where rehabilitation programmes, either in rehabilitation units or in home rehabilitation programmes, have proven effective.21–23 Irrespective of this, our objective was to identify the prognostic factors that, together with rehabilitation, would be involved in functional maintenance, 12 months after the HFBF, of the 271 patients studied; they had good, medium or bad functionality prior to the HFBF in relation to the activities of daily living
Of patients who survive an HFBF, less than 80%, with good previous functionality,17 maintain functionality one year on. In our study, 54.8% maintained previous functionality. This is a very good result, as in this case all the patients alive at 12 months following the HFBF had good, medium or poor previous functionality.
As in other similar studies,17,20,24–28 the prognostic factors related to functional maintenance at 12 months following an HFBF, in addition to a younger age, are those that relate to good health status prior to the fracture. Thus the results of this study are in accordance with the study carried out by Fukui et al.,24 with similarities with respect to age, prior health status and greater independence in activities of daily living.
With regard to undertaking activities of daily living, although Fukui et al.24 highlight independence in the bathroom as a strong predictor of functional maintenance. This item is included in the BI, in our case we evaluate the BI overall.
With reference to dementia, the diagnostic criteria (DSM-5 and NIA-AA)29,30 include dependence in activities of daily living. Thus, a diagnosis of dementia, knowing that its prevalence31,32 and degree of severity increase with age, is a factor associated with functional loss after an HFBF.18,25,28 In this study, the absence of dementia in the younger patients is related to functional maintenance during follow-up.
With reference to delirium, Vochteloo et al.26 report that about 50% of patients with an HFBF do not maintain their mobility at one year of follow-up. In their model, delirium and dependence for basic activities of daily living are predictors of not maintaining the mobility prior to the HFBF. In our model, the absence of delirium (geriatric syndrome associated with poor prognosis)33,34 and independence for activities of daily living were a highly relevant factor associated with maintenance of functionality at 12 months following an HFBF.
Finally, in our multidisciplinary care model, a short surgical waiting time, together with early initiation of physiotherapy and occupational therapy, are possibly determining factors for the degree of functional recovery on discharge, which in turn were one of the factors associated with maintenance of functionality at 12 months. It is important to note that patients with greater independence in activities of daily living on discharge achieve better results at 12 months follow-up; this result is similar to that observed in the systematic review conducted by Lim et al.18
It is possible that the promotion and attainment of a higher level of independence in the activities of daily living on discharge, together with the prevention and early detection of delirium are the only factors that could be considered modifiable.
The results obtained in this study support the current recommendations for the care of older patients with HFBF, and show how pre- and post-operative management of these patients, in orthogeriatric units, improves short and medium-term care outcomes.4,35–44
The strengths of our study are: it was conducted in an acute geriatric unit; the sample is a clear representation of geriatric patients, specifically those who require most intervention in specialist units adapted to their needs. We also point out the study's observational and single-centre design as its main limitations. Other limitations could be the lack of face-to-face follow-up and not having collected intermediate events during the follow-up.
ConclusionsIn our model we found that the predictive factors for functional maintenance at 12 months following an HFBF are younger age and better ability to perform the instrumental activities of daily living.
Our results are particularly relevant, since they enable us to identify patients at possible risk of loss of functionality and, thus, be able to intervene in factors that can be modified.
Conducting a multi-centre randomised clinical trial would allow the results of this study and others to be validated, and endorse the favourable outcomes of orthogeriatric units, as a validated model for the comprehensive care of elderly patients following an HFBF.
Level of evidenceLevel of evidence III.
FundingThis research study has received no specific grants from public sector, commercial or not-for-profit agencies.
Conflict of interestsThe authors have no conflict of interests to declare.
To Professor Ramón Miralles for his invaluable devotion to managing this study and to Sr. Sergi Mojal for preparing the statistical study.
Please cite this article as: Gamboa-Arango A, Duaso E, Formiga F, Marimón P, Sandiumenge M, Salgado MT, et al. Factores pronósticos de buena funcionalidad a los 12 meses, de una fractura de cadera. Estudio Maluc Anoia. Rev Esp Cir Ortop Traumatol. 2020;64:57–63.