Currently, there is no stablished pre-operative model that helps the orthopaedic surgeon predict the final graft diameter in anterior cruciate ligament reconstruction (ACLR). The purpose of this study was to determine whether there is a correlation between semitendinosus (ST) and gracilis (GT) cross-sectional area (CSA) evaluated pre-operatively in mm2 using magnetic resonance imaging (MRI) and the final intra-operative ST–GT autograft diameter in mm2.
MethodsA retrospective study was designed, 89 patients undergoing ACLR with hamstring autograft participated. We analysed ST-CSA (mm2) and GT-CSA (mm2) using pre-operative MRI, intra-operative autograft diameter, age, sex, side of the injury, weight, height and body mass index (BMI).
ResultsA moderate–strong correlation was identified between final autograft diameter and ST–GT CSA in MRI (Pearson correlation coefficient .6911 p<.001). We observed that, if the combination of ST-CSA and GT-STA is at least 19mm2, the probability of obtaining an autograft with a diameter greater than or equal to 8mm is 91.8% or more. The ROC curve analysis demonstrated, in this model, that this predictive method on MRI correctly discriminates in over 95.6% of cases between achieving or otherwise an autograft greater than or equal to 8mm during surgery. Intra and interobserver concordance of the MRI measurements were excellent, as shown in the intraobserver intraclass correlation coefficient (CCI) of .79 and the interobserver CCI of .84 and .77 for the ST and GT respectively.
ConclusionsPreoperative determinations of ST-CSA and GT-CSA (mm2) using MRI correlate with the final autograft diameter. This method represents a reliable and reproducible model to predict the hamstring autograft diameter in ACLR.
Level of evidenceRetrospective cohort study, level IV.
Clinical relevanceA review of the available literature reveals a higher risk of ACL failure or re-rupture if the graft is smaller than 8mm in diameter. Despite being an important factor there is no established pre-operative model that predicts the final graft diameter. Knowing beforehand the possibilities of obtaining a hamstring autograft with a diameter greater than or equal to 8mm would help the orthopaedic surgeon to better plan the surgery and to anticipate the need for other graft options (such as bone-patellar-tendon-bone autograft or allografts, amongst other alternatives).
Actualmente no existe un modelo establecido en la práctica clínica que permita predecir de forma fiable este parámetro. El objetivo del estudio fue valorar si existe correlación entre el área total sumada de los tendones recto interno (TRI) y semitendinoso (ST) en estudios preoperatorios de resonancia magnética (RM) y el diámetro intraoperatorio de la plastia.
MétodosEstudio retrospectivo que analizó 89 pacientes intervenidos de reconstrucción de ligamento cruzado anterior con plastia autóloga de isquiotibiales. Las variables analizadas fueron: área en mm2 de ST y TRI en estudio preoperatorio de RM, diámetro intraoperatorio de plastia, edad, sexo, lateralidad de intervención, peso, talla e índice de masa corporal.
ResultadosSe halló una correlación fuerte-moderada entre el diámetro final de la plastia y el sumatorio del área total del ST y del TRI (Índice de correlación de Pearson 0,6911; p<0,001). También se observó que, si la combinación de las áreas mencionadas es de 19mm2 o más, la probabilidad de tener una plastia de diámetro mayor o igual a 8mm es de al menos 91,8%. El análisis de la curva ROC demostró que este método predictivo discrimina correctamente en más del 95,6% de las ocasiones entre obtener una plastia de diámetro mayor o igual de 8mm o no tenerla. La concordancia inter e intraobservador de las mediciones realizadas en RM fue excelente en ambos casos con índices de correlación intraclase intraobservador (CCI) de 0,79 y CCI interobservador de 0,84, CCI 0,77 para tendón ST y TRI respectivamente.
ConclusionesEl área total de los tendones ST y TRI (mm2), medida preoperatoriamente en el estudio de RM, se correlaciona con el diámetro final de la plastia y constituye un método fiable y reproducible para predecir el grosor de la plastia autóloga de isquiotibiales.
Nivel de evidenciaCohortes retrospectivo, nivel de evidencia iv.
Relevancia clínicaEn la literatura revisada se establece que una plastia menor de 8mm de diámetro se asocia a una mayor probabilidad de rerotura y/o fallo. Pese a ser un factor determinante actualmente no existe un modelo establecido en la práctica clínica que permita predecir de forma fiable el diámetro final de la plastia. Conocer de antemano las probabilidades de que la plastia autóloga de isquiotibiales alcance un diámetro suficiente (igual o mayor a 8mm) permitiría al cirujano ortopédico planificar mejor la intervención y anticipar cuándo se van a tener que utilizar otras alternativas de injerto (utilización de autoinjerto tipo HTH o de aloinjerto, entre otras opciones).
Rupture of the anterior cruciate ligament (ACL) is one of the most common ligament lesions of the knee.1,2 In Young patients with an ACL lesion and with clinical symptoms of failure or instability, surgical reconstruction is the treatment of choice.3–6
There are different options when choosing technique and tissues to be used, with autologous hamstring graft being one of the most used alternatives.6–13 One of the technical aspects with the highest repercussions on reconstruction outcome is the final diameter of the graft.14 In the revised literature a graft under 8mm diameter was associated with a higher probability of renewed rupture and/or graft failure.15,16
Unlike other graft options if the hamstring tendons are used it is unknown preoperatively what the final diameter of the graft will be.6 When during surgery the orthopaedic surgeon finds there is insufficient diameter in the graft several options are then available: to extract a new graft from the patient (bone-patellar-tendon-bone type allograft or autograft, quadriceps tendon, contra-lateral leg hamstring tendon, etc.), change the surgical technique (for example, retrograde drilling technique, with which the length of the femoral tunnel can be changed and therefore the conformation and thickness of the graft), or, if available, use an allograft from the tissue bank. None of these options are exempt from risks and on occasions, they are alternatives that have not been discussed with the patient prior to the operation, or alter the normal course of procedures for the surgical team.
Most patients who will undergo a reconstruction of the anterior cruciate ligament have had a preoperative magnetic resonance study to confirm diagnosis. Being able to use this imaging test to predict the diameter of the graft would mean that the problem of an insufficient graft could be anticipated and the risk-benefit of alternatives could be assessed with the patient.
The aim of the study was as follows: to assess whether there was any correlation between the total area of the semitendinosus and gracilis tendons in MR imaging and the intraoperative diameter of the graft, and also to determine with what probability we can obtain a graft greater than or equal to 8mm. The secondary study aim was to study the relationship between anthropometric variables and final graft diameter.
Material and methodsA retrospective, observational study was conducted, which included all patients who had undergone ACL reconstruction between January 2012 and December 2017 by the same orthopaedic surgeon. Inclusion criteria were: reconstruction with autologous quadrupled semitendinosus and gracilis tendons; preoperative MRI study included in the clinical file and complete description of the technique and graft in the surgical report. Patients with previous surgery on the same knee and altered measurement by imaging were excluded, as were patients with allogenous or mixed graft and patients whose clinical history or surgical report did not match one of the study variables.
Information was collected on 397 patients who underwent ACL reconstruction carried out during this time interval. Eighty nine patients met with all the inclusion criteria. Excluded cases were those where the magnetic resonance study had been carried out in a different centre from that of the surgery, and as a result the images for making the measurements were not recovered. In other cases the graft information was incomplete in the surgical report (type of conformation, type of graft used, final diameter of the graft, etc.) or the graft used was a BTB autograft type or an allograft. The variables collected and analysed were: semitendinosus (mm2) and gracilis (mm2) areas measured through preoperative MRI, age, sex, side of injury, weight, height and body mass index.
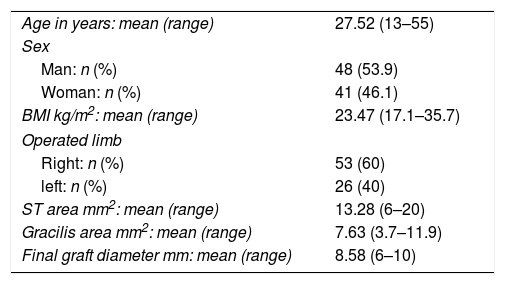
Demographic dataThere were 89 participants in the study, 53.9% (n=48) of whom were men and 46.1% (n=41) women. Mean age was 27.52 years (range 13–55), mean weight was 69.42kg, mean height was 1.71m and average BMI was 23.47kg/m2 (range 17.1–35.7). 60% (n=53) of ACL reconstructions were on the right side and the remaining 40% (n=26) on the left (Table 1).
Demographic variables and measurements in magnetic resonance.
| Age in years: mean (range) | 27.52 (13–55) |
| Sex | |
| Man: n (%) | 48 (53.9) |
| Woman: n (%) | 41 (46.1) |
| BMI kg/m2: mean (range) | 23.47 (17.1–35.7) |
| Operated limb | |
| Right: n (%) | 53 (60) |
| left: n (%) | 26 (40) |
| ST area mm2: mean (range) | 13.28 (6–20) |
| Gracilis area mm2: mean (range) | 7.63 (3.7–11.9) |
| Final graft diameter mm: mean (range) | 8.58 (6–10) |
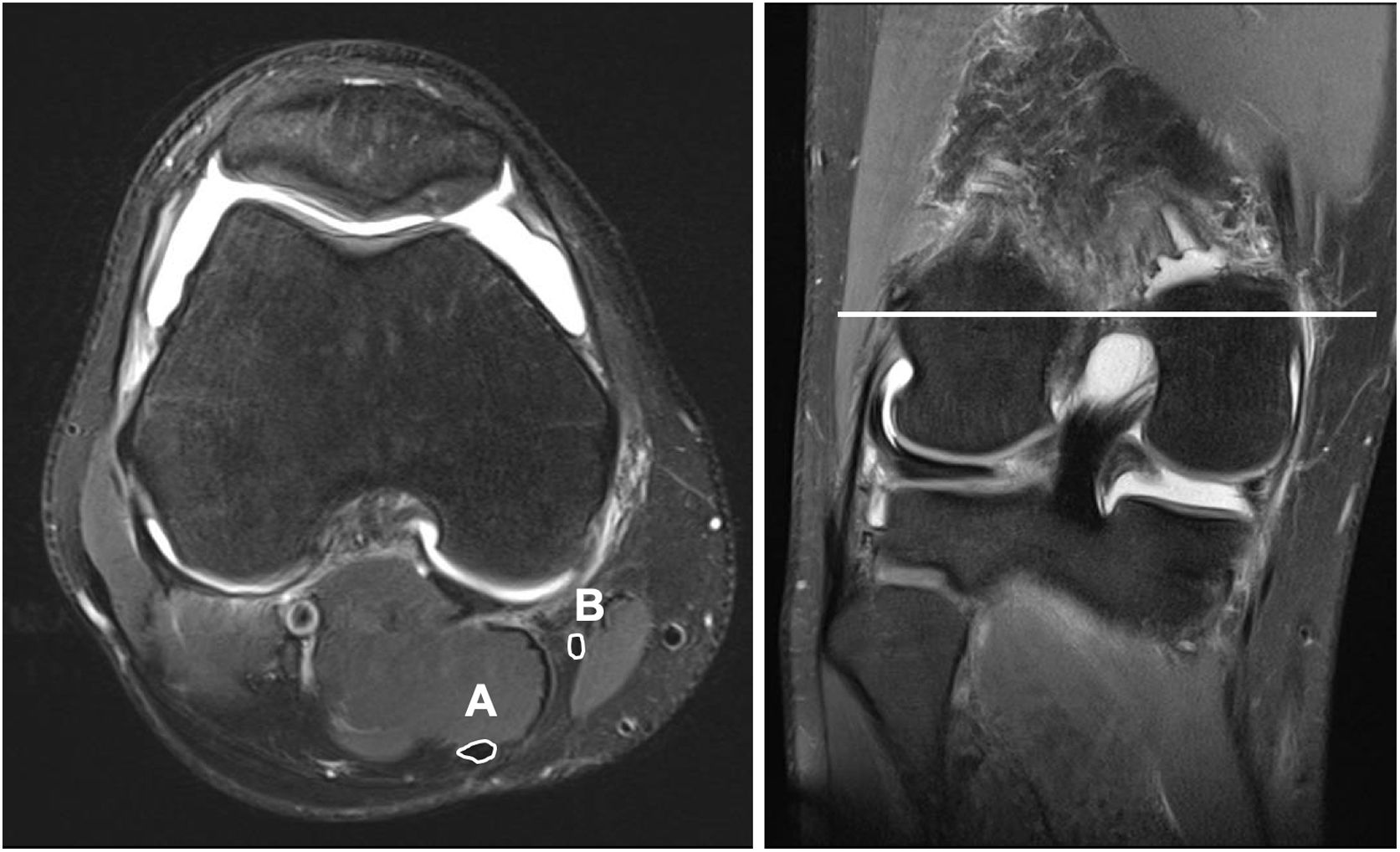
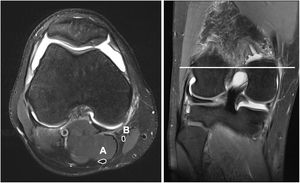
The same magnetic resonance imaging was used in all patients (SKYRA 3 Teslas, Siemens, Erlangen, Germany). Coronal, sagittal and axial plane sections were obtained every 3mm with a knee coil. During the study the patients held a standardised consistent supine position, with hip extension and 30° knee flexion. To do so pillows were used which helped the patient to maintain the before-mentioned posture. The semitendinosus and gracilis tendon areas were calculated with the Carestream (Carestream Health, Toronto, Canada) programme. The cross-sectioning from which the area of the tendons was measured was obtained by identifying the widest region of the medial femoral condyl in a coronal cross-section. Once this point had been recognised, we identified its corresponding axial section. A manual measuring tool was used to measure the perimeter of the gracilis and semitendinosus tendons. After tracing the programme automatically calculated the area in mm2 corresponding to the surface area drawn (Fig. 1). To minimise possible intraobserver variability this measurement was made on 3 occasions in each patient, with the mean of the 3 evaluations being recorded as the final value. All the measurements were made by 2 people who were unaware of the final graft diameter for each patient.
The same surgical technique of ACL reconstruction was used in all patients using autologous tendons (semitendinosus and gracilis). Once the tendons had been obtained and the adjacent muscle tissue removed a new ligament was reconstructed with quadrupled graft. This new ligament was attached in the femur using a 15mm XO Button fixation device (ConMed, Linvatec Int); tibial attachment was made with Matrix (ConMed, Linvatec Int) cannulated interference screw.
The final graft diameter was measured intraoperatively with graft sizer (increase of .5mm between orifices), the lower diameter being defined as that through which the graft was able to pass completely.
Statistical analysisAn analysis of the intraclass correlation coefficient (ICC) was performed to quantify the reliability of the measurements made in magnetic resonance imaging and determine the intraobserver and interobserver concordance. The Pearson correlation coefficient was calculated to determine the relationship between the different variables studied (area of semitendinosus and gracilis tendon in mm2, age, sex, weight, height, BMI, side of injury) and the final diameter of the graft. Logistic regression was also used to describe the probability that the measurement of the semitendinosus and gracilis tendon area in MRI, in the specific axial cross-section corresponded to a graft greater than or equal to 8mm in diameter. To do this the different results were dichotomised in the graft greater than or equal to 8mm (sufficient graft) or under 8mm (insufficient graft). To determine the capacity of model discrimination a ROC curve was performed. A probability level of .05 was accepted as being statistically significant for all statistical tests. Confidence intervals were calculated, whenever possible, for a 95% confidence level. All statistical determinations were performed using Stata (version 12.0; Stata, College Station, TX).
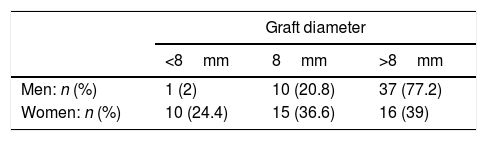
ResultsThe mean area of the semitendinosus tendon in axial cross-sections of MRI was 13.28mm2 (range 6–20), whilst the mean area of the gracilis tendon was 7.63mm2 (range 3.7–7.9). Intraobserver concordance of measurements made in the magnetic resonance imaging was excellent, with a CCI of .79. Interobserver concordance was also excellent, both for the semitendinosus tendon and the gracilis tendon measurement (CCI=.84, CCI=.77, respectively). The average of the whole semitendinosus and gracilis area for each patient was 20.91mm2 (range 10–29.4). Mean diameter of the grafts measured intraoperatively was 8.6mm (range 6–10) (Table 1). In 11 out of 89 patients operated on a graft of under 8mm diameter was obtained (Table 2).
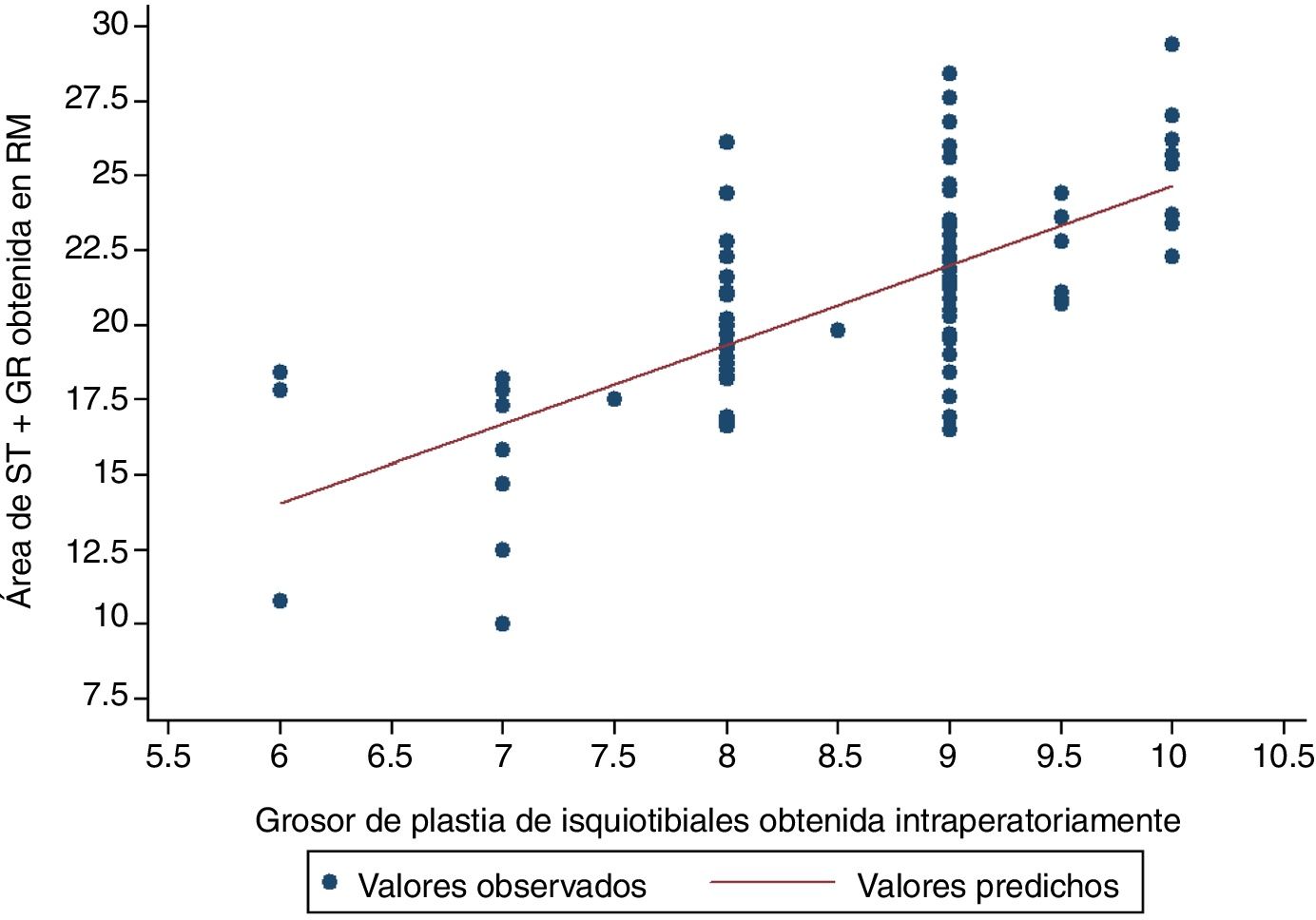
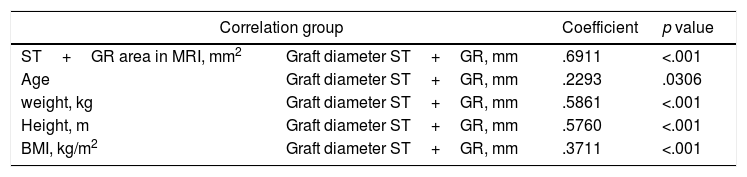
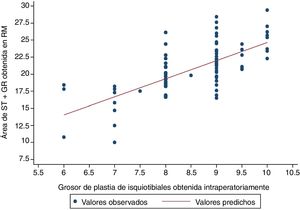
The variable which most correlated with the final diameter of the graft was the total area in the MRI of the semintendinosus tendon and the gracilis tendon, presenting a Pearson correlation coefficient of .6911; p<.0001 (Table 3 and Fig. 2).
Pearson correlation.
| Correlation group | Coefficient | p value | |
|---|---|---|---|
| ST+GR area in MRI, mm2 | Graft diameter ST+GR, mm | .6911 | <.001 |
| Age | Graft diameter ST+GR, mm | .2293 | .0306 |
| weight, kg | Graft diameter ST+GR, mm | .5861 | <.001 |
| Height, m | Graft diameter ST+GR, mm | .5760 | <.001 |
| BMI, kg/m2 | Graft diameter ST+GR, mm | .3711 | <.001 |
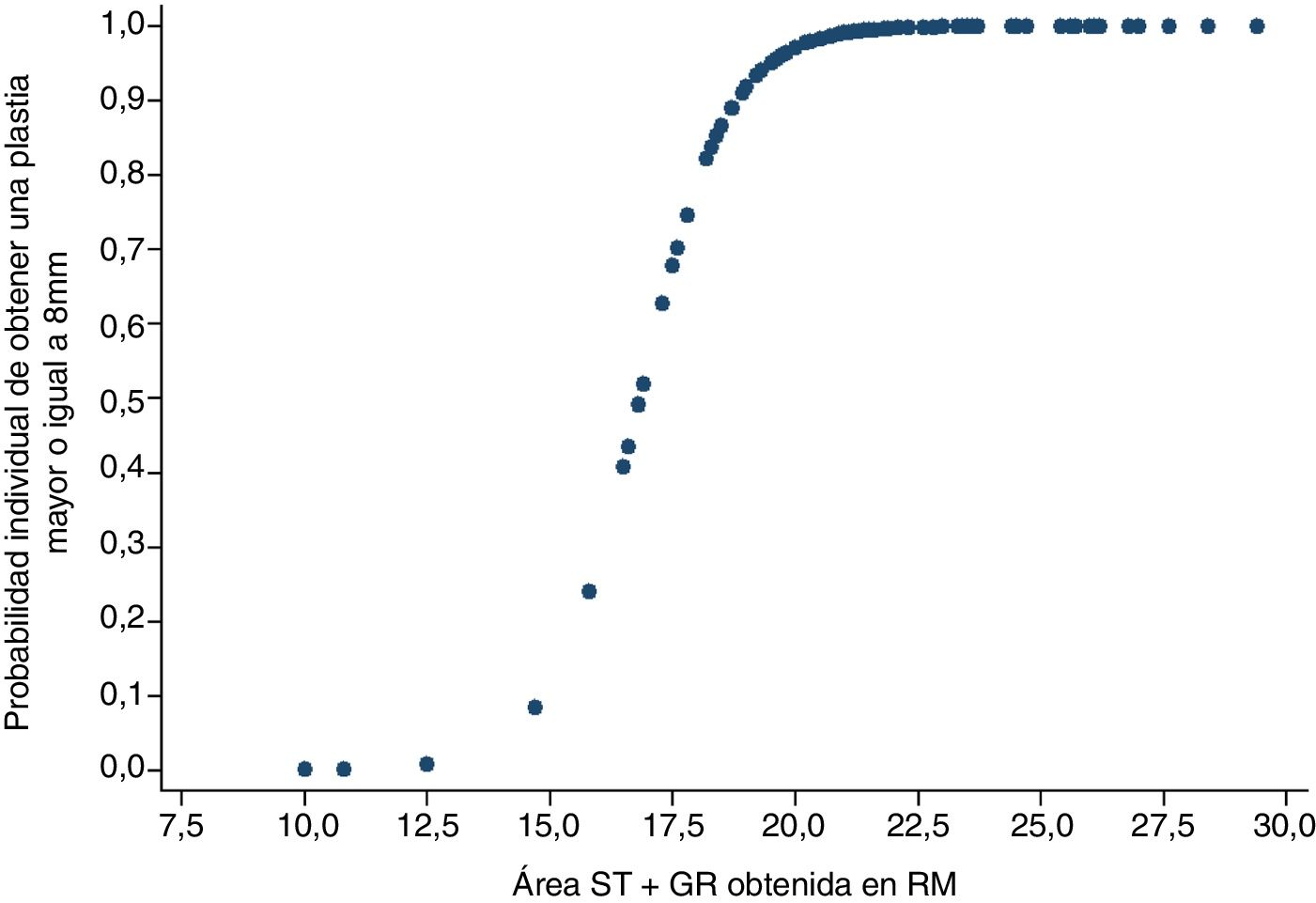
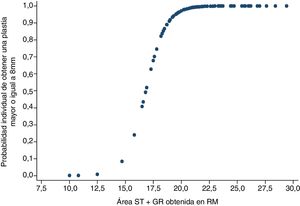
The graft diameter was dichotomised in sufficient diameter (equal to or greater than 8mm) or insufficient (under 8mm). Using a logistic regression model it was observed that when the combination of area in MRI of the semintendinosus tendon and the gracilis tendon was 15.8mm2, then the probability of obtaining a final graft equal to or greater than 8mm was 23.9%. In contrast, if the aim of the areas in MRI of both tendons measured 19.8mm2 or above, the probability of obtaining a sufficient graft would be at least 91.8% (Fig. 3).
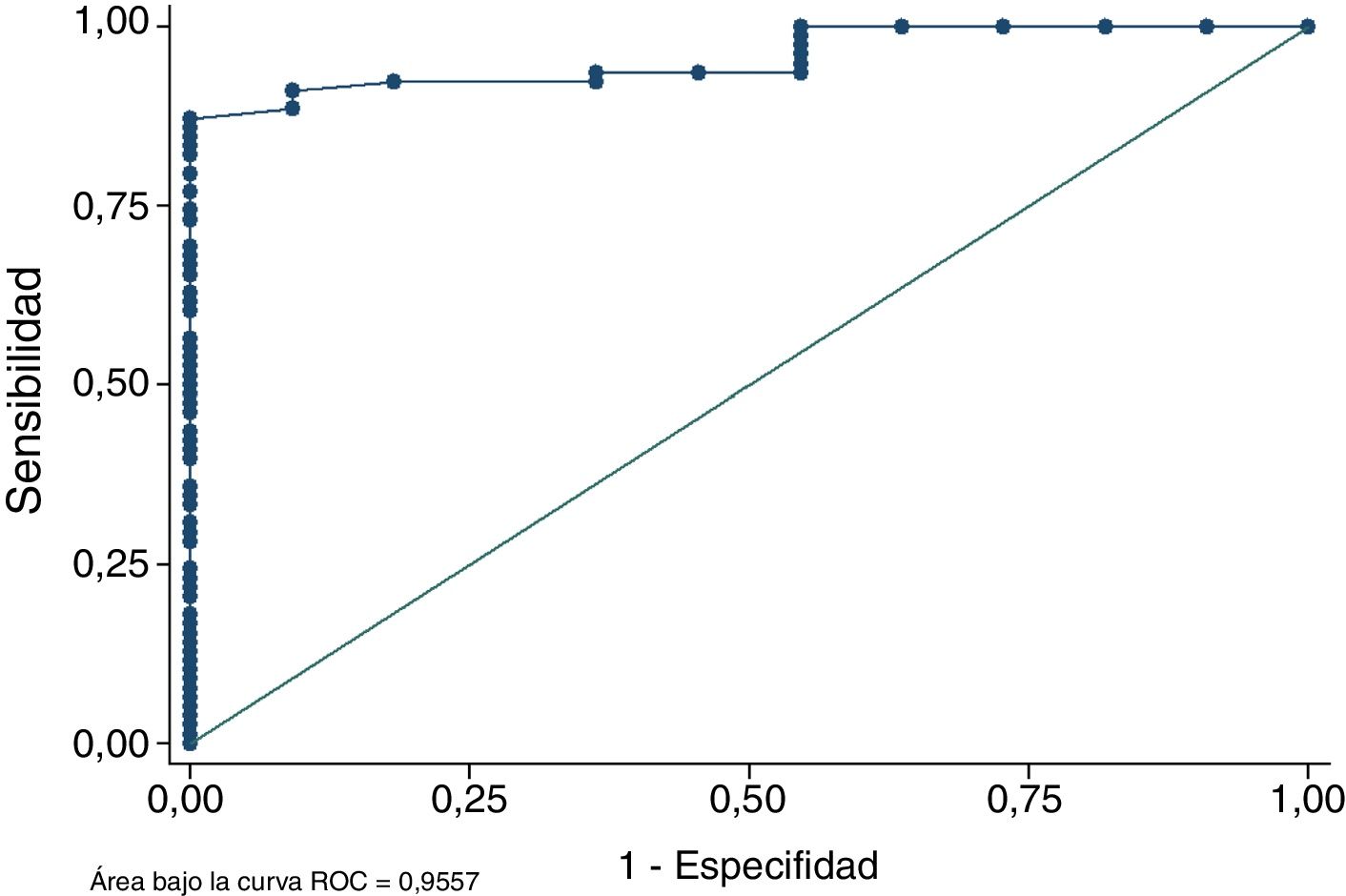
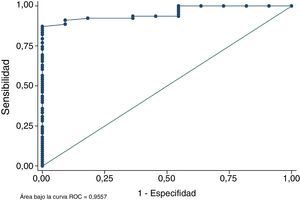
Analysis of the ROC curve demonstrated that the total area of the semintendinosus tendon and the gracilis tendon measured in MRI correctly discriminated in over 95.57% of occasions between obtaining a graft diameter equal to or above 8mm or not having it (Fig. 4). This parameter confirms that MRI measurement of the area is a reliable method for predicting whether the final diameter of the graft will be sufficient or not. The Homer–Lemeshow goodness of fit compares the probability observed from the result (final diameter of the graft equal to or greater than 8mm) with the before-mentioned probability of the result. The Homer–Lemeshow goodness of fit in the sample was .879 confirming good calibration of the model.
Out of the 78 patients whose real graft diameter was equal to or greater than 8mm, 75 were correctly classified as “sufficient graft” by adding up the MRI areas (sensitivity of 96.15%). For those whose true graft diameter was under 8mm, 5 of the 11 patients were correctly classified. Therefore, specificity was 45.45%. Positive predictive value was 75 out of 81 (92.6%), whilst the negative predictive value was 5 out of 8 (62.5%).
With regard to the differences between sexes we observed that 75.6% of the women of the cohort obtained sufficient graft (31/41) compared with 97.9% of the men (47/48), with this difference being statistically significant (p<.001, Pearson chi-squared) (Table 2).
With regard to the analysis of anthropometric variables a moderate correlation was observed between weight and final graft diameter with a Pearson correlation index of .5861 (p<.001), and also between final height and diameter of the graft (mm2), with a Pearson correction index of .5760 (p<.0001). A low correlation was found between age (Pearson correlation index of .2293, p<.001) and final graft diameter, also between BMI (.3711, p<.001) and final graft diameter (Table 3).
DiscussionThe most important finding of the study was that the hamstring autograft diameter can be predicted reliably by measuring the tendon and the gracilis tendon areas in axial cross-sections of preoperative MRI.
Several studies have reported the relationship between a graft diameter under 8mm and the higher probability of graft failure.7,14,16,17 Some authors have quantified this risk, such as the study by Snaebjörnsson et al.,18 concluding that for every .5mm of diameter increase, the risk of re-rupture dropped (it was multiplied by .86). Although groups with particularly high risk of ACL reconstruction failure have been identified, such as patients aged under 2014,19 and patients who take up practising different sports again, there are no studies which raise the suggested minimum thickness of 8mm to a higher figure. No recommendations have been reported on different diameters according to sex, height or sport demands.20,21
Despite the final diameter of the graft being a key factor in reconstructive ACL surgical success, at present there is no established model in clinical practice that enables reliable prediction to be made of final hamstring tendon graft diameters. This project confirms the validity or MRI as a prediction method for final graft diameter, providing the orthopaedic surgeon with a highly useful tool in surgical planning.
One relevant data for daily clinical practice extracted from this study is that a combined area of 19.8mm2 (the sum of the semitendinosus and the gracilis tendon area in MRI) may be used as a minimum cut-off point to obtain a graft of at least 8mm thickness. In keeping with that described by other authors22–24 this diameter cohort under 8mm has been identified with greater frequency in women than in men (24.3% of women and 2% of men) (Table 2). Jannsen et al.25 and Ma et al.26 obtained diameters under 8mm in 2.8% of men and in 11.3% of women, and in 18.4% of men and 42.3% of women respectively.
The semitendinosus tendon area measured in axial cross-sections by MRI in our population (13.28mm2) is similar to that identified in the cohort by Galanis et al.22 (13.22mm2), Beyzadeoglu et al.23 (12.9mm2) and Erquicia et al.24 (12.4mm2), but lower than the findings by Wernecke et al.17 (16.5mm2). The mean area of the gracilis tendon measured in MRI axial cross-sections is 7.63mm2, similar to the findings by Beyzadeoglu et al.23 (7.3mm2) and Erquicia et al.24 (6.4mm2), whilst that of the population studied by Galanis et al.22 presented with areas which were slightly larger (10.18mm2).
As indicated by Galanis et al.22 several causes may impact the differences found between studies, including different protocols of the position of the lower limbs during the MRI study or different MRI cut off selection criteria where calculations of the area were made. When analysing the data a correlation was found of .6911 (p<.0001) between the semitendinosus and gracilis MRI areas and the final graft diameter. Other authors have also studied this same association and obtained similar Pearson correlation indexes: .813 Galanis et al.,22 .86 Erquicia et al.24 and .641 Wernecke et al.17
Some authors previously studied the relationship between several anthropometric variables and the final diameter of the hamstring autograft,27–30 with all of them finding a low to moderate correlation between height and final diameter of the graft. Goyal et al.28 identified a Pearson correlation index of .358 (p<.001) between height and final graft diameter and Schwartzberg et al.29 of .3903. These results are in keeping with the findings from our study (Pearson correlation index of .5760; p<.001). Also, Schwartzberg et al.29 identified a moderate correlation between weight and final graft diameter (Pearson correlation index=.5118), similar to the results of our cohort (Pearson correlation index=.5861; p<.001). However, the correlation between these parameters found by Goyal et al.28 did not show any significant association (Pearson correlation index=.245; p=.060). Regarding correlation between BMI and final graft diameter none of the authors found there to be any significant relationship between both variables; in this study a low intensity correlation was found (Pearson correlation index of .3711; p<.0001).
Other authors have studied the precision of the hamstring graft diameter using ultrasound scan28–30 with differing results. Astur et al.31 and Momaya et al.32 concluded that the preoperative study with ultrasound of the hamstring tendon diameter did not reliably correlate with the final graft diameter. Erquicia et al.,24 however, found a similar correlation between ultrasound findings to those of magnetic resonance and the final graft diameter. Although this is a potentially useful method for predicting hamstring graft diameter, there could be several difficulties which limit the applicability of this method, including the availability of an ultrasound scan in medical practices, the need for specific training in ultrasound management and the technical difficulty of carrying out the study and measurements.
This study has certain limitations. Firstly is the absence of data about the length of the tendons once extracted. Depending on the length of the graft a larger diameter graft may be obtained, if a different configuration is used. In this way, by comparing the different options using the same tendon, the diameter of the graft will be higher and the final length of the graft lower if a quintupled configuration. Also, no data were collected on the situation of the graft at tibia level once the femoral and tibial component was attached (the graft exceeds the tunnel length, the totality of the graft within the tunnel, the graft does not include the total tibial tunnel).
In addition to this, is the non standardized magnification of the MRI imaging cross-section from which the semitendinosus and gracilis tendon area were to be calculated. In each case the researchers in charge of doing the measurement used magnification (zoom) with which the most precise image possible could be obtained, and with which therefore the tendon area was better marked out. Zoom usage enables enhanced visualisation of the tendon area, a more precise tracing of its perimeter and therefore more accurate final graft estimation. If the available literature is reviewed consensus may be reached in the zoom to be used: Bickel et al.33 carried out a similar study with a non standardised magnification whilst Vincent et al.34 decided to use magnification 4×, Grawe et al.9 magnification 2× and Cobanoglu et al.35 magnification 10×. In this study each researcher used magnification (always between 4 and 10) which gave the best visualisation and marked the tendon perimeter. Despite the fact that both observers used the magnification they found most appropriate, the interobserver concordance results showed a high level of agreement in excellent measurement, demonstrating that there were no differences of measurement. Furthermore, we consider that tracing the perimeter of the tendons with a blurred image, as may occur when using the same magnification systematically, would have major repercussions on the quality and precision of measurements, and therefore on the reliability and reproducibility of the proposed method.
ConclusionThe total semitendinosus and gracilis area (mm2), measured preoperatively in MRI axial cross-section, correlated with the final graft diameter and is a reliable and reproducible method of predicting autologous graft thickness of the hamstrings. Moderate correlation was found between the patient's weight and final graft diameter and also between the patient's height and final graft diameter. These data provide a useful tool for preoperative anticipation regarding the risk of obtaining a graft of insufficient diameter.
Conflict of interestsThe authors declare there is no potential conflict of interests related to this article.
Please cite this article as: Pérez-Mozas M, Payo-Ollero J, Montiel-TerrónV, Valentí-Nin JR, Valentí-Azcárate A. Predicción preoperatoria del diámetro de la plastia autóloga de isquiotibiales en reconstrucción de ligamento cruzado anterior. Rev Esp Cir Ortop Traumatol. 2020. https://doi.org/10.1016/j.recot.2020.04.009