Pelvic tilt influences the relative position between total hip arthroplasty (THA) components. Changes in lumbar spine over time may affect clinical and radiological outcomes of THA during follow-up. We assessed the evolution of pelvic tilt and cup position after THA for a minimum follow-up of five years and the possible appearance of complications.
Matherial and methodsThis retrospective study includes 48 patients operated between 2008 and 2012. Clinical data, complication and radiological analysis included sacro-femoral-pubic and acetabular abduction angles on the anteroposterior pelvic view; and cup anteversion angle on the lateral cross-table hip view according to Woo and Morrey. All assessments were done pre-operatively and at 6 weeks, one, two and five years post-operatively.
ResultsMean sacro-femoral-pubic decreased from 60.6° preoperatively to 58.8° at five years (p > .05), more in females (from 63.3 to 59.3) than males (58.7 to 58.3). Acetabular abduction increased from 47.3 at six-week postoperatively to 48.2 at five years (p > .05) and acetabular anteversion varied from 24.3° to 36.1° (p < .04). There were four dislocations: one late recurrent dislocation which required cup revision.
ConclusionDespite the sacro-femoral-pubic angle tendency to decrease and anteversion tendency to increase after five years, larger studies with longer follow-up are needed to confirm the potential increasing in long term complications.
La inclinación pélvica influye en la posición relativa de los componentes de la prótesis total de cadera (PTC) la cual a su vez se puede modificar por los cambios evolutivos que aparecen en la columna lumbar. Nuestro objetivo es estudiar la variación de la posición de la pelvis y del componente acetabular en pacientes con PTC durante 5 años y las posibles complicaciones.
Material y métodosEl actual estudio retrospectivo incluye 48 pacientes intervenidos de PTC entre 2008 y 2012. Se recogen los datos clínicos, complicaciones y los cambios radiológicos en relación a los ángulos sacrofemoropúbicos, inclinación acetabular en la radiografía anteroposterior de pelvis y la anteversión lateral según Woo-y-Morrey. Las mediciones se realizaron preoperatoriamente, a las 6 semanas, al año, a los dos años y a los cinco años de la intervención.
ResultadosEl sacrofemoropúbico disminuyó de 60,6° preoperatorio a 58,8° a los cinco años (p > 0,05), más en mujeres (de 63,3° a 59,3°) que en varones (de 58,7° a 58,3°). La inclinación acetabular aumentó de 47,3° a las seis semanas después de la PTC a 48,2° a los cinco años (p > 0,05) y la anteversión de 24,3° a 36,1° (p < 0,04). Hubo cuatro luxaciones, una recurrente con cirugía de recambio.
ConclusionesA pesar de la tendencia de la disminución del ángulo sacrofemoropúbico y del aumento de la anteversión del componente acetabular cinco años después de la PTC, se necesitan estudios de mayor número de casos y seguimiento para confirmar si aumentan las complicaciones a largo plazo.
Despite the excellent long-term results of total hip arthroscopy (THA), acetabular component replacement surgery – primarily due to wear, followed by late dislocation – remains the most frequent revision surgery.1 Although the Lewinnek safe zone has been classically established for acetabular component positioning,2 recent large case studies have fuelled further debate on the most appropriate parameters.3,4 There are more factors for us to consider such as the correct reconstruction of the anatomical centre of the hip, of the hip abduction mechanism or the influence of the spino-pelvic complex4–7 as positional changes in activities of daily living such as sitting or walking have been observed to influence the functional position of the prosthetic component.8
Spino-pelvic alignment in the sagittal plane is a parameter that has gained in importance in recent years. Sagittal balance is an adjustment of the pelvic and spinal parameters to allow a posture that presents the most physiological axis of gravity possible requiring the least energy consumption and is the result of the morphology of the spine together with compensatory mechanisms. Based on lateral radiographs, in 1998 Beaupere described the three parameters most used today and the relationship between them: pelvic incidence, sacral slope (SS) and pelvic tilt or pelvic version (PT),9 these describe the sagittal orientation of the pelvis. Pelvic incidence is a fixed anatomical parameter specific to each patient, while SS and PT vary inversely proportional to pelvic position. Among the sagittal balance compensation mechanisms that have been described, the first to be activated is a change of pelvic retroversion or increased PT. In ageing, there is a decrease in lumbar lordosis, which causes SS to decrease and PT to increase.10 This verticalization of the pelvis would result in increased anteversion of the acetabular component and affect the function of the coxofemoral joint.11 Therefore, although PT does not change significantly in the immediate postoperative period following THA,12 with the increase in PT associated with ageing, it is likely there would be an increase in anteversion of the acetabular component with respect to the femoral stem.
The main objective of our study was to test whether the variation of PT over a minimum follow-up of 5 years affects the position of the acetabular component in patients who have undergone THA. We also studied the clinical outcomes of these patients, and the onset of potential associated complications.
Material and methodsWe conducted a retrospective observational study from prospective data collection of patients undergoing THA due to coxarthrosis between 2008 and 2012. Patients undergoing surgery for femoral neck fractures, tumours or with associated neuromuscular diseases were excluded. Only patients treated with the same design of cementless THA with BiHapro cup (Zimmer-Biomet, Warsaw, IN, USA), highly cross-linked polyethylene insert and Bimetric stem (Zimmer-Biomet) were included in the analysis. All cases were implanted with a 32 mm diameter Cr-Co metal femoral head. We used a posterolateral approach with reconstruction of the capsule and external rotators, or with preservation of the piriformis, in all cases.13 The postoperative protocol included our hospital’s antibiotic prophylactic, thromboembolic and functional recovery recommendations. Ambulation with two crutches and partial weight bearing was allowed from day 2 to 6 weeks postoperatively. In addition to their demographic data, the patients were classified into three groups according to the condition of the lumbar spine at the time of surgery: group 1, no or minimal degenerative changes; group 2, moderate or advanced degenerative changes; and group 3, patients who underwent lumbar spine arthrodesis.
Of the 57 patients who underwent surgery, 48 patients were finally included with a mean age of 70.2 years (63–75) and 58.3% were male. Nineteen patients underwent bilateral THA. Although lumbar degenerative signs were observed in all cases, in 28 cases the changes were mild, they were moderate or severe in 17 cases, and 3 underwent lumbar arthrodesis.
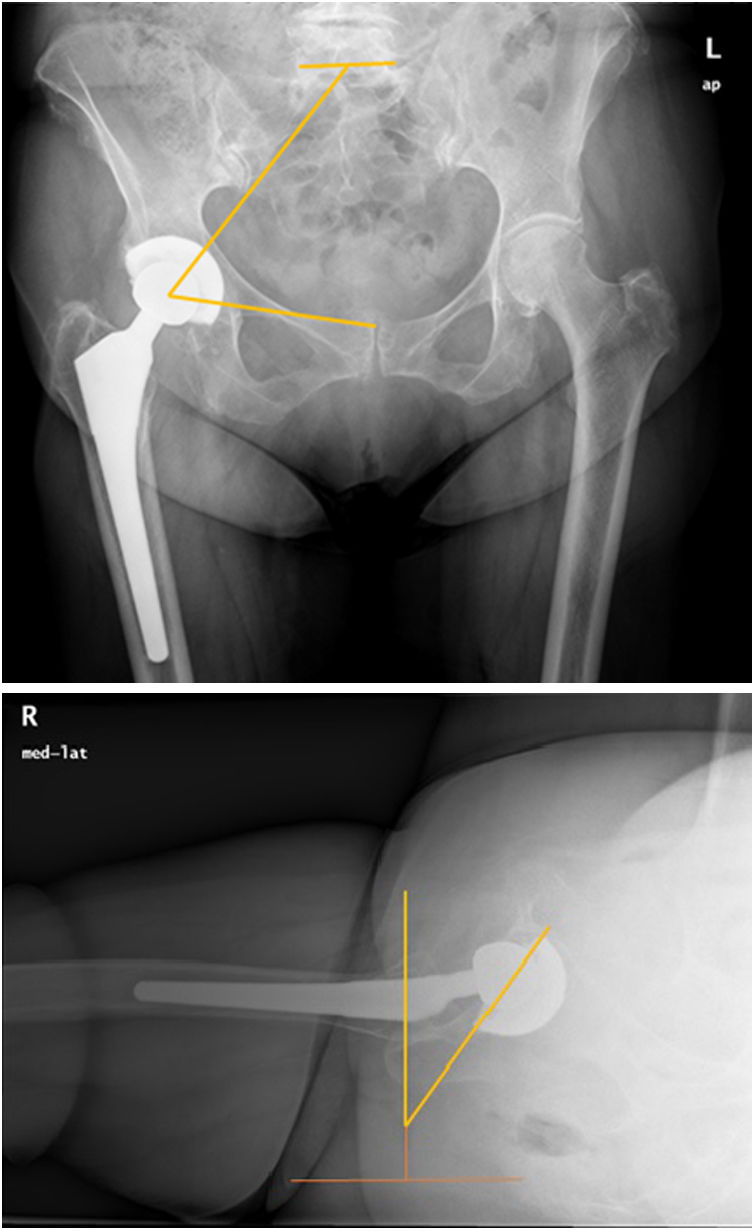
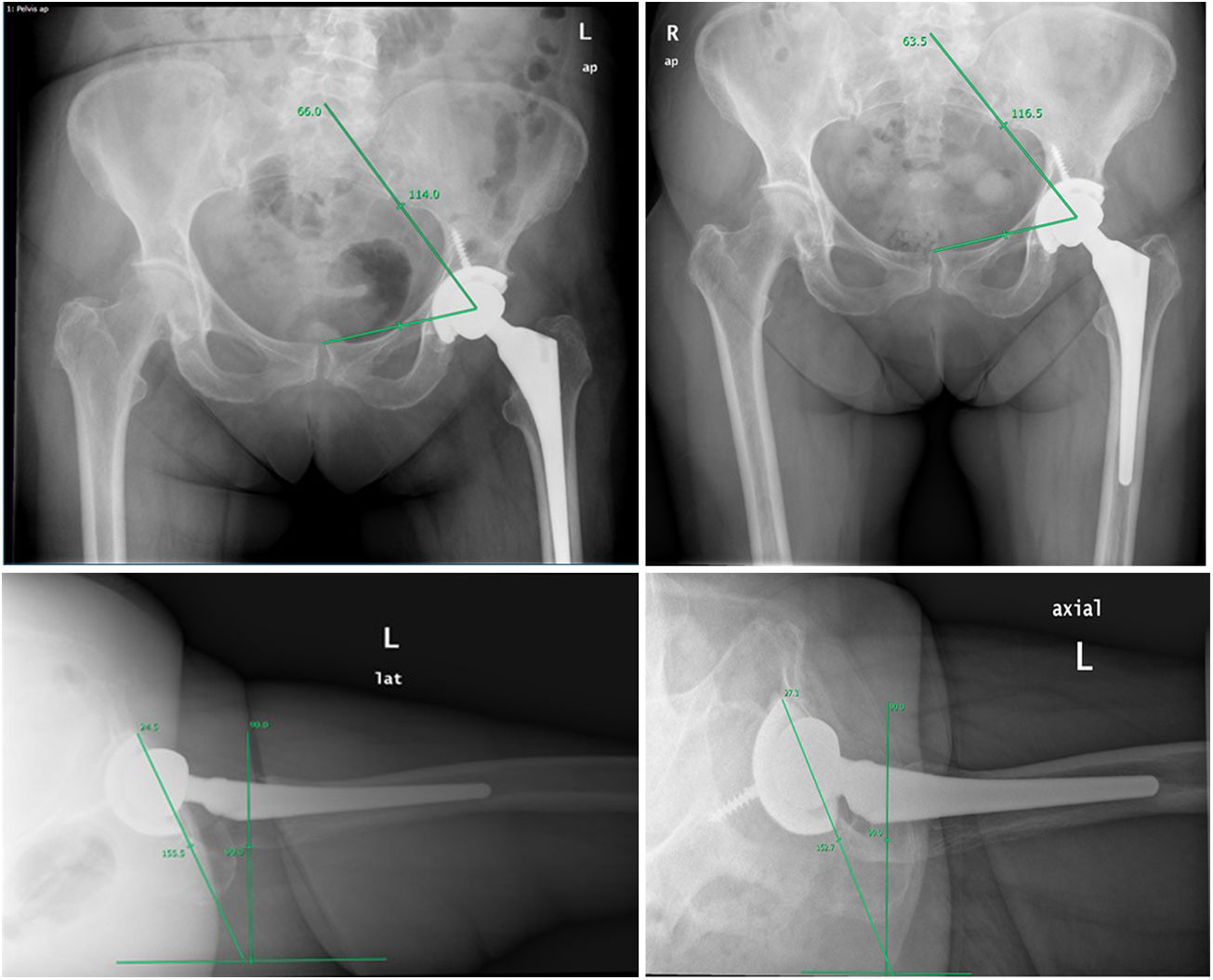
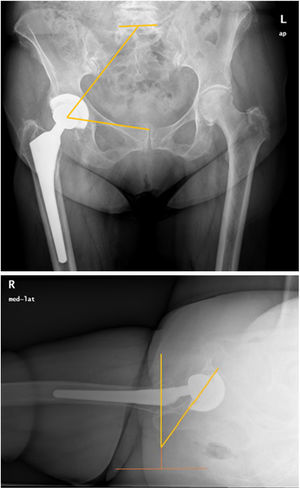
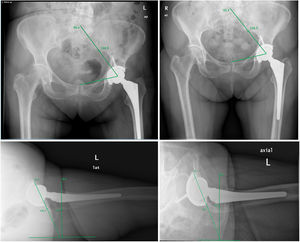
The clinical analysis of the patients included the Harris scale score (HHS), which analyses pain and functional outcomes before THA, at 3 months, at 1 year and at 5 years following the surgery. For radiological analysis, the anteroposterior (AP) projection of the pelvis was used to measure the sacro-femoral-pubic angle (SFP) and acetabular tilt (AT) and pure lateral projection for cup anteversion (AV) preoperatively, at 6 months, 1, 2 and 5 years after the surgery. Although lateral radiographs are frequently taken in spinal surgery that enable direct measurement of the sagittal parameters, the most common projection in clinical practice is the AP pelvis radiograph; therefore, new parameters have been sought to establish this relationship between the frontal plane and the sagittal plane, such as the SFP – the angle between the middle of the upper plateau of S1 and the centre of one of the acetabula, and from this to the centre of the pubic symphysis (Fig. 1A). Previous studies have validated the correlation of the SFP angle with PT, allowing one to be calculated from the other using the formula PT = 74.6 − 0.942 × (SFP).14 This method has been described as reliable and reproducible in assessing PT.15 On the lateral radiograph, we used the Woo and Morrey method to measure AV, which measures the anteversion of the cup with respect to a line perpendicular to the horizontal edge of the radiograph (the angle corresponds to the line tangential to the anterior edge of the acetabular cup and the line perpendicular to the horizontal of the radiograph)16 (Fig. 1B). The same investigator took the measurements of each angle independently from the surgery. This same observer performed the measurements a second and third time to establish intraobserver correlation.
Statistical analysisMean values (standard deviation) were used for quantitative variables and frequencies for quantitative variables. The Student's t-test and ANOVA for independent samples and the general linear model were used to analyse changes in clinical outcome over time for different factors (lumbar spine status and uni- or bilateral THA).
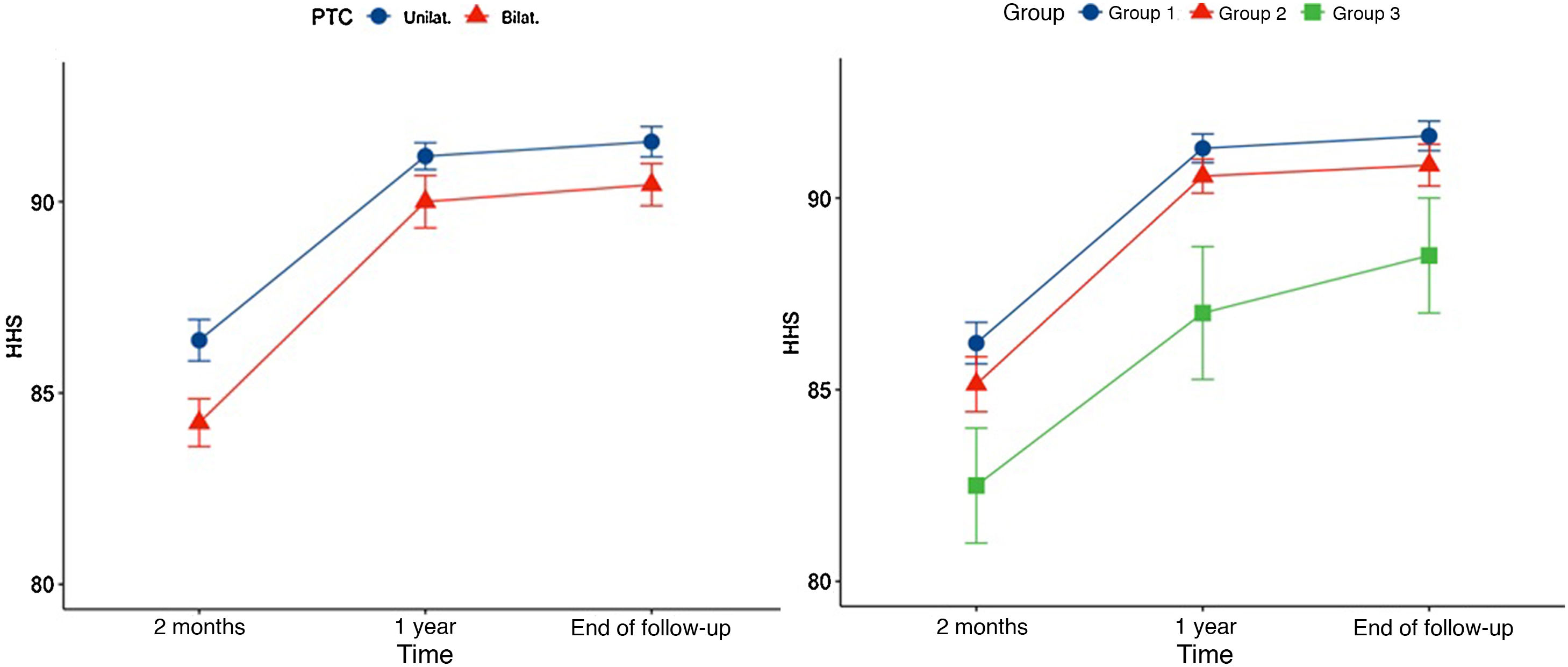
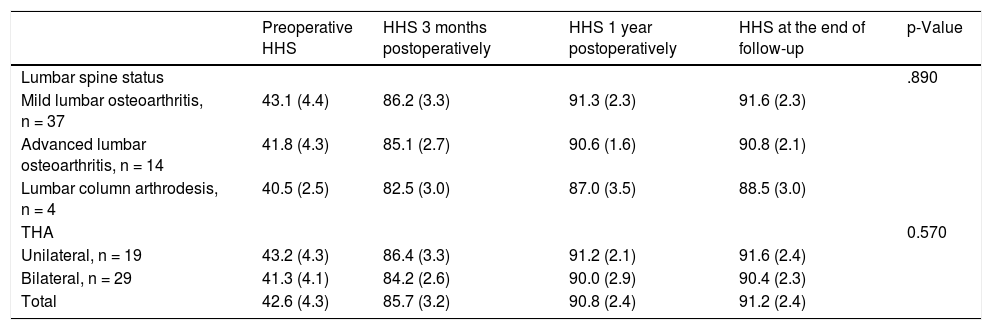
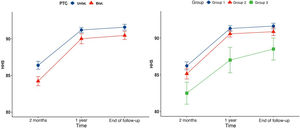
ResultsClinical outcomes improved from a mean preoperative HHS of 42.6 (SD: 4.3) to 85.7 (SD: 3.2) at 3 months following THA, 90.8 (SD: 2.4) at 1 year and 91.2 (SD: 2.4) at the end of follow-up (p < .001). Forty-four patients had an excellent outcome (HHS > 90) and the remaining four had a good outcome (80–90). Having undergone one or two THA and lumbar spine status did not influence clinical outcomes over time in general (p < .05) (Table 1). However, the overall linear model detected that the mean HHS score at three months postoperatively in patients with one THA was better than in those who had undergone surgery in both hips (p < .05) (Fig. 2). The same analysis showed that patients with mild lumbar osteoarthritis achieved a better score than patients with lumbar arthrodesis one year following THA and at the end of follow-up (Fig. 2B).
Evolution of clinical outcomes according to the Harris scale (mean SD) in relation to lumbar spine status and having undergone one or two THAs.
| Preoperative HHS | HHS 3 months postoperatively | HHS 1 year postoperatively | HHS at the end of follow-up | p-Value | |
|---|---|---|---|---|---|
| Lumbar spine status | .890 | ||||
| Mild lumbar osteoarthritis, n = 37 | 43.1 (4.4) | 86.2 (3.3) | 91.3 (2.3) | 91.6 (2.3) | |
| Advanced lumbar osteoarthritis, n = 14 | 41.8 (4.3) | 85.1 (2.7) | 90.6 (1.6) | 90.8 (2.1) | |
| Lumbar column arthrodesis, n = 4 | 40.5 (2.5) | 82.5 (3.0) | 87.0 (3.5) | 88.5 (3.0) | |
| THA | 0.570 | ||||
| Unilateral, n = 19 | 43.2 (4.3) | 86.4 (3.3) | 91.2 (2.1) | 91.6 (2.4) | |
| Bilateral, n = 29 | 41.3 (4.1) | 84.2 (2.6) | 90.0 (2.9) | 90.4 (2.3) | |
| Total | 42.6 (4.3) | 85.7 (3.2) | 90.8 (2.4) | 91.2 (2.4) |
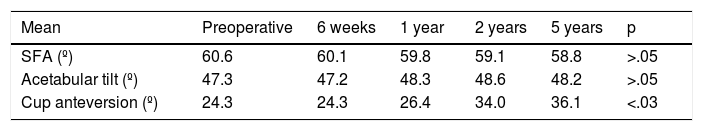
The mean pre-surgical SFP angle was 60.6°, evolving to 60.1° at 1 year and 58.8° at 5 years (p > .05) (Table 2). On analysis of the male and female data, the women had a higher initial SFP angle (63.3° vs. 58.7°; p < .02). Throughout the revisions, the SFP angle in the men changed by less than 1° (p > .05), while the women showed a tendency towards pelvic retroversion, decreasing by 2.1° at one year and up to 4.1° at five years (p < .04). Indirectly calculating PT using the formula PT = 4.6 − 0.94 × (SFP) resulted in a change in PT from 17.4° preoperatively to 19.1° postoperatively at 5 years. The AT of the acetabular component assessed in the coronal plane hardly changed throughout follow-up, from 47.3° to 48.2° (p > .05). On the lateral projection, the AV of the cup at 6 months was 24.3° and increased with follow-up over time to 36.1°, varying by 11.8° in both males and females (p < .03). Intraobserver correlation was high for all parameters. For the SFP at all stages the minimum correlation was .977 and maximum .989, in the case of lateral tilt the correlation at each stage ranged from .876 to .976, and the Woo and Morrey angle from .977 to .983.
Evolution of mean sacro-femoral-pubic (SFP) angle values, of acetabular tilt and of cup anteversion over time.
| Mean | Preoperative | 6 weeks | 1 year | 2 years | 5 years | p |
|---|---|---|---|---|---|---|
| SFA (º) | 60.6 | 60.1 | 59.8 | 59.1 | 58.8 | >.05 |
| Acetabular tilt (º) | 47.3 | 47.2 | 48.3 | 48.6 | 48.2 | >.05 |
| Cup anteversion (º) | 24.3 | 24.3 | 26.4 | 34.0 | 36.1 | <.03 |
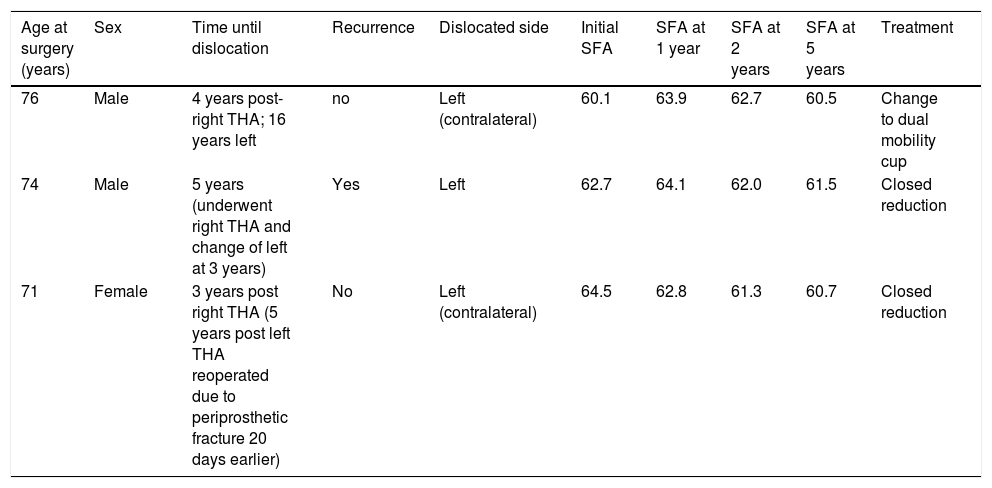
At the end of follow-up there were no cases of aseptic loosening of the prosthetic components or infections. There was one case of periprosthetic fracture one month following the surgery that required femoral stem replacement. Regarding the cases of instability (Table 3), there was one case of early dislocation before the first postoperative year, two cases of late dislocation of the hip contralateral to the hip studied and one late dislocation of the same hip, all related to traumatic events. Although in all three cases the clinical outcomes were good or excellent, the HHS scores were slightly below the mean (86, 86 and 90, respectively). Analysing the pelvic parameters of the late dislocation cases, all three had an increased SPA angle between 2 and 4 (Fig. 3). Three cases were resolved with closed reduction, but one 73-year-old male suffered further episodes at 5 and 6 years after the primary THA requiring cup replacement to a dual mobility acetabular component and no further dislocations were reported.
Clinical and radiological data of patients with delayed dislocations.
| Age at surgery (years) | Sex | Time until dislocation | Recurrence | Dislocated side | Initial SFA | SFA at 1 year | SFA at 2 years | SFA at 5 years | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| 76 | Male | 4 years post- right THA; 16 years left | no | Left (contralateral) | 60.1 | 63.9 | 62.7 | 60.5 | Change to dual mobility cup |
| 74 | Male | 5 years (underwent right THA and change of left at 3 years) | Yes | Left | 62.7 | 64.1 | 62.0 | 61.5 | Closed reduction |
| 71 | Female | 3 years post right THA (5 years post left THA reoperated due to periprosthetic fracture 20 days earlier) | No | Left (contralateral) | 64.5 | 62.8 | 61.3 | 60.7 | Closed reduction |
To maintain sagittal balance, interactions between the lumbar spine, pelvis and hip joint require correct balance and alignment.17 Therefore, if there is an imbalance in these static and dynamic parameters, compensatory mechanisms appear that attempt to change the axes at the expense of pelvic mobility.18 Physiological ageing, associated with a loss of lumbar lordosis and increased pelvic retroversion10 results in a change in the position of the lower limbs, with anteversion of the acetabulum, hip extension and knee flexion in an attempt to rebalance the sagittal profile.19 Recent research has confirmed the importance of these changes in the dynamic orientation of the acetabular components and joint mobility in THA.8,11 Although PT does not change significantly in the short term in patients undergoing THA surgery, there are few studies that assess the influence of the changes that lumbar spine ageing cause to the position of the implant.
The clinical outcomes of the patients included in our study were excellent or good in most cases, although there were interesting observations. Although we did not use a scale to assess specific outcomes in relation to lumbar pain and function, we did observe that clinical improvement was greater in patients with mild lumbar spine disease. Although poorer function could partially explain these results, we are aware that spinal pain radiating to the hip is difficult to assess.20 In most patients, low back pain improves after THA, although in a small percentage it may increase or recur. It is currently very difficult to assess the influence of clinical outcomes and sagittal imbalance associated with disease in patients undergoing THA.21
In our analysis we confirmed that the changes observed in decreased SFA and, therefore, increased PT, at a minimum follow-up of five years, affect the position of the acetabular cup. Although plain radiographs are less accurate than other techniques such as computed tomography or low-irradiation systems such as EOS that allow three-dimensional reconstructions,12,22 the method used has already been validated14,15 and radiological projections are routinely used and remain useful although performed in the supine position.23 There are other measurements that can be assessed on plain anterior pelvic radiograph that have shown varying degrees of reliability, SFP being the most reliable.24 The intra-observer correlation in our study was high, and therefore the variables chosen seem reproducible and reliable for adequate follow-up in the clinic over time. Several previous studies have validated the correlation between the SFP angle defined by Blondel with sagittal parameters, in particular with PT.9,11,12 Blondel et al. managed to define a relationship between the two following the formula PT = 74.6 − .942 × (SFP).14 In our series the SFP evolved from 60.6° to 58.8°, which if we apply Blondel's formula would imply a change in PT from 17.4° to 19.1°. This corresponds to the expected increase in pelvic retroversion. Similarly, the change in acetabular anteversion was an increase of 11.8°. There could be various explanations for these changes, either ageing which causes an increase in lumbar osteoarthritis or the possible onset of osteoporotic fractures.17 It is possible that the greater incidence of osteoporotic fractures in women25 would explain the greater pelvic retroversion observed with respect to the small change in men, although these would need to be studied during follow-up to confirm this. The decrease in LL with the consequent change in PT due to the interaction between the spine and the pelvis is probably the major factor.
Late hip dislocation is infrequent, with published rates ranging from 0% to 5%. However, when this complication does occur, it has significant morbidity as it tends to recur,26 and together with loosening, it is one of the main reasons for THA reoperation in the medium and long term.1,27 The low incidence of this event and its multifactorial origin makes study of its causality difficult and its treatment challenging. Described factors include those specific to the patient, such as age, musculature, degree of patient collaboration or previous interventions, and others specific to the surgical technique, such as the approach or the position and size of the implants.6 Lewinnek et al. proposed a "safe zone" for acetabular component placement, with a lateral tilt of 40° ± 10° with respect to the sagittal plane and an anteversion of 15° ± 10° with respect to the coronal plane to minimise the risk of dislocation of the THA.2 Nevertheless, many late dislocations occur in THA where the acetabular component is in the safety zone.28 Progressive functional anteversion of the acetabular component associated with ageing, so that it does not act dynamically in the safety zone, has been proposed as a possible cause. It has been described that in patients with degenerative disc disease, not only is there a variation of PT, but functionally the acetabulum also takes a different functional position from healthy patients and its anteversion increases.29 Pelvic imbalance is now considered one of the main factors causing dislocation from the first postoperative year onwards, once the hip joint capsule has healed.30 In our study, two males and one female between the ages of 69 and 73 years had late dislocation and they did not have a greater than average decrease in SFP angle. Patient 1, who had dislocation of the contralateral hip, had a an SFP of 62.7° which decreased to 61.5°; patient 2, also with dislocation of the contralateral hip, ranged from 64° to 60° and patient 3 from 72° to 70°. These dislocations were related to traumatic events, and therefore variation in the sagittal profile does not seem to have been the main cause of instability. However, there are case reports in which PT has varied significantly over time, mainly secondary to osteoporotic kyphotic fractures, and has been correlated with late anterior THA dislocation.31 Finally, although the incidence of prosthetic replacement surgery and dislocation is clearly related in series with large numbers of patients, in our study no patient required replacement surgery and we could not establish this relationship.32,33
Our study has several limitations. Firstly, although the tendency was as expected, the follow-up time is only 5 years. The progressive ageing of the population and longer-term follow-up would probably allow for greater variation in sagittal parameters. Secondly, as the radiographs were taken in the supine position, it is not possible to study the anteversion of the acetabular component in the patient's daily life; therefore, in future studies it would be interesting to X-ray in the standing and seated positions to better assess pelvic changes. Although classification of lumbar osteoarthritis is based on the classic criteria of osteoarthritic involvement, the category of lumbar or lumbosacral arthrodesis has been included in this study due to its clinical implications. Studies investigating more advanced imaging methods (EOS, CT) allow more specific assessment of these changes; however, this study reflects routine clinical management with conventional radiology. Similarly, a larger number of cases included in the study could provide more clinical and radiological data and more statistical power. Finally, although only patients with primary coxarthrosis who underwent the same implant and surgical technique were included, the few cases means that the findings obtained should be considered preliminary.
Taking the above limitations into account, we conclude that posterior PT increases over the years in patients who undergo THA, particularly females. These changes may increase anteversion of the acetabular component and influence the increase in the dislocation rate in the medium to long term. Studies with larger numbers of cases are needed to confirm these preliminary findings.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Maya B, Gómez Luque J, García Rey E. Evolución de la inclinación pélvica a lo largo del tiempo en pacientes intervenidos de prótesis total de cadera. Estudio clínico-radiológico con un seguimiento mínimo de cinco años. Rev Esp Cir Ortop Traumatol. 2021;65:400–406.