Non-traumatic limping is a common reason for consultation in paediatric emergencies. Although transient synovitis of the hip (TS) is the most frequent diagnosis, there are cases of limping secondary to serious pathologies. The aim of this review is to describe the variables related to non-traumatic limp that come to the Paediatric Emergency Department to establish the best management protocol, making the most of resources and speeding up emergency care.
Material and methodA prospective study was conducted, selecting all children less than 15 years old who consulted as paediatric emergencies for non-traumatic limping during the 2014. Clinical variables, complementary examinations and diagnoses were collected in the emergency room consultation and 6 months after the consultation.
ResultsDuring 2014, 146 patients (0.69% of the emergencies) were included in the non-traumatic limping study. Four cases of severe limping were diagnosed: 2 leukaemias, 1 septic arthritis and 1 acetabular bone tumour. The most frequent diagnosis was TS (53.16%). At 6 months, 135 children (92.4%) had resolved lameness. The diagnosis was changed in 9 children (6.1%). Children with TS had fewer days of evolution, and 77% were between 3 and 10 years old. Children with a final diagnosis of severe pathology had a limp for longer, fever and did not weight bear on ambulation.
ConclusionsIn limping of probable hip origin, at the ages of between 3 and 10, without fever or systemic symptoms and of less than one week's onset, it is possible to make a clinical diagnosis of TS limiting the use of complementary examinations.
La cojera no traumática es un motivo frecuente de consulta en urgencias pediátricas (UPED). Aunque el diagnóstico más frecuente es la sinovitis transitoria de cadera (STC), existen cojeras secundarias a patologías graves. El objetivo de este estudio es describir las variables relacionadas con las cojeras no traumáticas en UPED, las características clínicas, las pruebas complementarias y el diagnóstico final para establecer el mejor protocolo de manejo, rentabilizando recursos y agilizando la asistencia en urgencias.
Material y métodoEstudio prospectivo, en niños<15 años que consultaron en UPED por cojera no traumática durante el año 2014. Se recogieron variables clínicas, exploraciones complementarias, diagnóstico en urgencias y a los 6 meses.
ResultadosDurante el 2014 se incluyó en el estudio por cojera no traumática a 146 pacientes, el 0,69% de las urgencias atendidas. Se diagnosticaron 4 casos de cojera grave: 2 leucemias, una artritis séptica y un tumor óseo acetabular. El diagnóstico más frecuente fue la STC (57,53%). A los 6 meses, 135 niños (92,4%) habían resuelto la cojera. Se modificó el diagnóstico en 9 pacientes (6,1%). Los niños con STC presentaban menos días de evolución y el 77% tenían entre 3 y 10 años. Los niños con diagnóstico final de cojera grave presentaban una cojera más prolongada, fiebre y no apoyo en la deambulación.
ConclusionesEn las cojeras con probable origen en la cadera en niños entre 3 años y 10 años, con ausencia de fiebre o síntomas sistémicos y evolución menor de una semana es posible realizar un diagnóstico clínico de STC limitando las exploraciones complementarias.
Gait alterations in children without a history of trauma are a frequent cause of consultation in Paediatric Emergency Departments (PED), with an incidence of from 1.5 to 3.6 cases per every 1000 children.1,2 Although in the majority of cases non-traumatic lameness is caused by a slight event that is self-limiting in functional terms, such as transient synovitis of the hip (TSH), there is a broad list of possible differential diagnoses and lameness may be a sign of serious disease such as osteomyelitis, septic arthritis or neoplasias.3–5
Diagnosis will usually be guided by a full history and complete clinical examination. It is rare for laboratory tests or imaging studies to be required, although sometimes complementary tests are indispensable to rule out severe lameness.
The majority of the studies published to date are retrospective and centre on specific diseases.6–8 Nevertheless, children do not go to a PED with a diagnosis, so that emergency paediatricians see a lame child and have to rule out severe causes, deciding whether or not to request complementary tests and which of the latter are the most indicated given the available resources.9 A swift and accurate diagnosis without using complementary tests excessively is desirable in PED for cases of severe lameness in children.
The aim of this study is to describe the variables which are associated with non-traumatic lameness in children who visit a PED, identifying their clinical characteristics, the complementary tests which are requested, clinical evolution and the initial and final diagnoses of these patients, to establish the best protocol for the management of these cases and to also expedite care in the Emergency Department.
Material and methodsThis is a prospective observational study that was undertaken in the PED of a tertiary hospital. It covers a population that was estimated in December 2014 to stand at 345,354 patients, of whom 52,126 (15.4%) are children under the age of 15 years old. Patients aged from 0 to 15 years old who visited the PED from 1 January to 31 December 2014 due to non-traumatic lameness were included. This study excluded children with a history of trauma or a known diagnosis as the cause of their lameness.
Data were gathered systematically in the PED including the following variables: age, sex, referral by paediatrician, month of the year in which they consulted, days of evolution, respiratory infection up to 15 days beforehand, fever (temperature ≥38°C) and/or systemic symptoms, weighting, the location of pain, external signs of inflammation, blood analysis, ultrasound examination, radiography, diagnosis in the PED and admission to hospital. The children's age was stratified in 3 groups of <3 years old, from 3 to 10 years old and ≥10 years old. 6 months after the visit to the PED the outpatient and hospital clinical history of the case was revised to evaluate the resolution of the lameness and the definitive diagnosis.
There was no protocol for the management of severe lameness in the PED during the study period. The decision to request additional tests and the initial diagnosis of patients were based on the individual criterion of the paediatrician who saw the child in the PED. The patients diagnosed osteomyelitis, septic arthritis or tumours were defined by this study as cases of severe lameness.
Statistical analysisCategorical variables are described using percentages and are analysed by the χ2 test or Fisher's exact test. Continuous variables are described using their average and standard deviation (SD) or median with their interquartile range (95% intervals of confidence, minimum and maximum) and they were analysed using non-parametric tests (Mann–Whitney's U test). Statistical analysis was performed using the Epidat 4.2 programme for Windows®. Epidat is an open distribution programme developed by the Epidemiology Department of the Dirección Xeral de Saúde Pública da Consellería de Sanidade (Xunta de Galicia) with the help of the Organización Panamericana de la Salud (OPS-WHO) and CES University, Colombia. Version 4.2 of Epidat was made available from 29 July 2016 onwards (email: soporte.epidat@sergas.es; www.sergas.es/Saude-publica/EPIDAT).
ResultsA total of 20,960 children aged from 0 to 15 years old were seen in 2014, 54% boys and 46% girls. 158 children were seen due to non-traumatic lameness, of whom 12 were excluded from the study as no lameness was found at the time of clinical examination and they were discharged with the diagnosis of normality. This study therefore includes 146 patients, 0.69% of all cases seen and corresponding to an incidence of 2.8 cases per every 1000 children <15 years old.
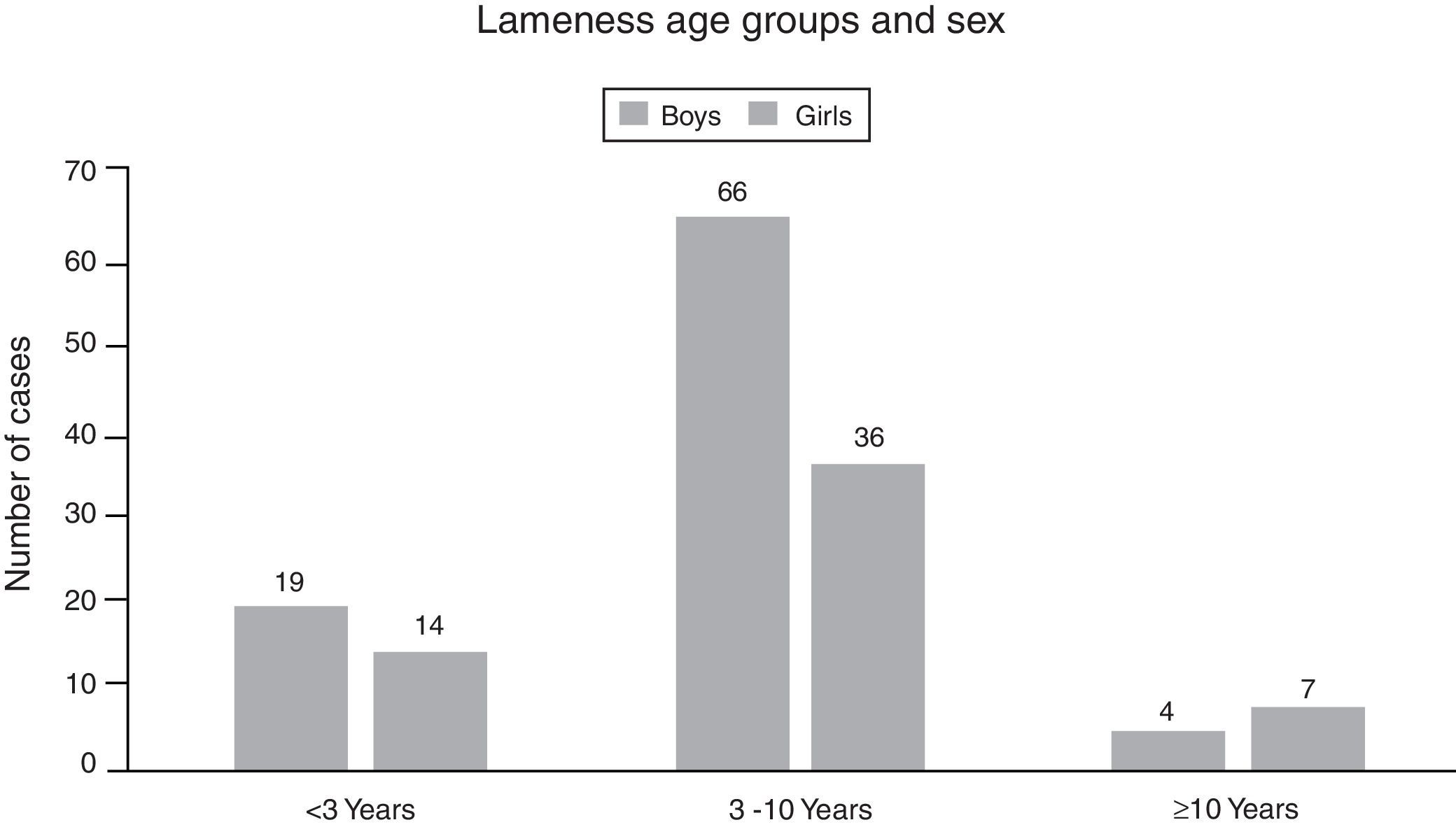
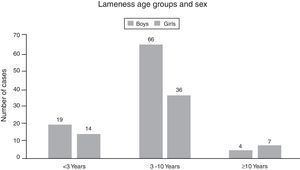
The average age of the children who consulted due to lameness was 5.2 years old (p25 3 p75 8, SD 3.38). There were more boys than girls (60.9% vs 39%) (Fig. 1). Their condition had evolved for an average of 5.4 days before they were seen (median 2 days, p25 0 p75 5), while 27 children (18.5%) were seen in the A&E department after referral from primary care.
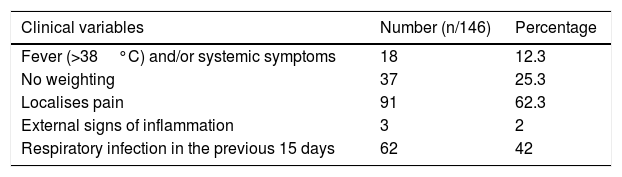
37% of the children could not locate or did not refer to a specific painful point as the cause of their lameness. However, following clinical examination this was attributed to hip pain in 79% of cases. The clinical variables recorded are shown in Table 1.
Clinical variables of lame children in the PED.
| Clinical variables | Number (n/146) | Percentage |
|---|---|---|
| Fever (>38°C) and/or systemic symptoms | 18 | 12.3 |
| No weighting | 37 | 25.3 |
| Localises pain | 91 | 62.3 |
| External signs of inflammation | 3 | 2 |
| Respiratory infection in the previous 15 days | 62 | 42 |
PED: Paediatric Emergency Department.
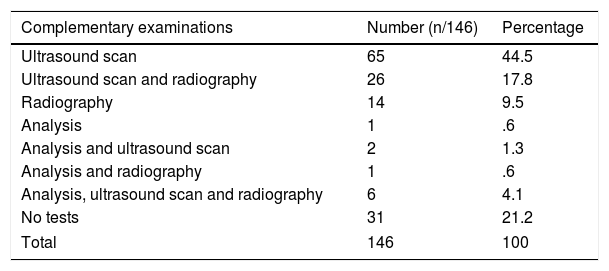
Ultrasound scan was the imaging test that was requested the most often (n=99/146, 67.8%), either alone or together with radiography or analysis. Of the 99 ultrasound scans requested, 97 were of the hip and 2 were of the knee. 47 radiographies were requested (n=47/146, 32.1%), 28 of the hip while the others were of different locations: the spinal column, knee, ankle and foot. Radiography detected pathology in 8 patients, showing increased space within joints except for those patients with bone lesion. The average age of the children for whom radiography was requested is 7.1 years old (median 7.5 years old) while those who were not X-rayed had an average age of 4.5 years old (median 3 years old). The complementary tests requested in the PED are shown in Table 2.
Complementary examinations requested in the PED for lame children.
| Complementary examinations | Number (n/146) | Percentage |
|---|---|---|
| Ultrasound scan | 65 | 44.5 |
| Ultrasound scan and radiography | 26 | 17.8 |
| Radiography | 14 | 9.5 |
| Analysis | 1 | .6 |
| Analysis and ultrasound scan | 2 | 1.3 |
| Analysis and radiography | 1 | .6 |
| Analysis, ultrasound scan and radiography | 6 | 4.1 |
| No tests | 31 | 21.2 |
| Total | 146 | 100 |
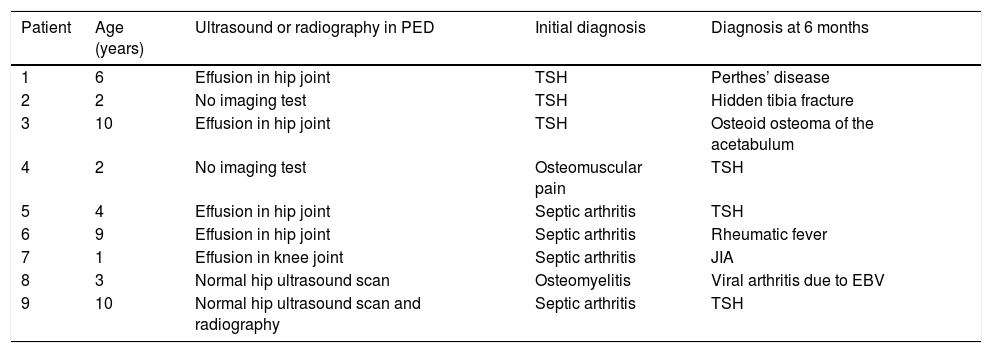
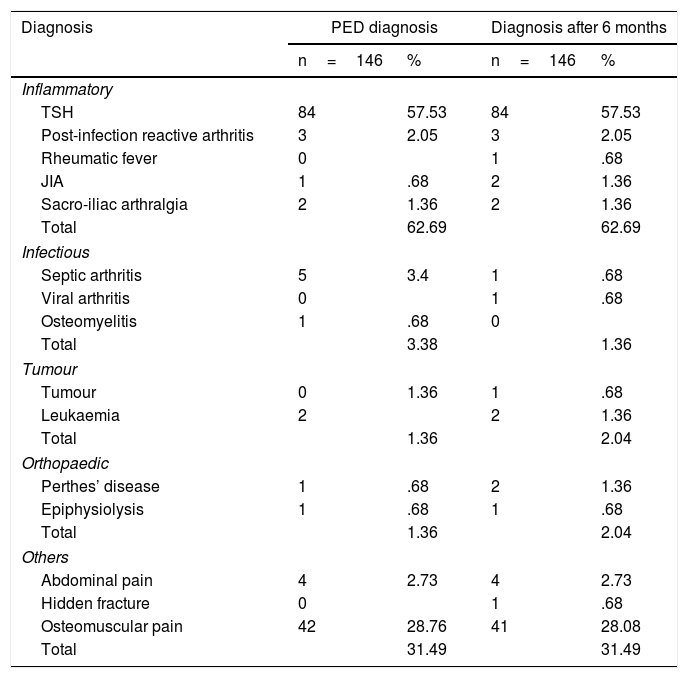
TSH was the most frequent diagnosis in the PED, and 8 patients (5.48%) were hospitalised due to the suspicion of severe lameness. 6 months after the visit to the PED, the lameness in 135 children (92.4%) had resolved while the other 11 remained with symptoms justified by their final diagnosis. The diagnosis was changed in 9 patients (6.1%), 5 of them during hospitalisation and the other 4 after further evaluation due to persistent lameness (Table 3). The most frequent final diagnosis was still TSH (n=84/146, 57.5%), followed by osteomuscular pain (n=41/146, 28.08%). 4 cases of severe lameness were finally confirmed (2.7%): 2 cases of type B acute leukaemia, one case of septic arthritis of the left hip and one osteoid osteoma of the acetabulum (Table 4).
Characteristics of the patients whose diagnosis changed.
| Patient | Age (years) | Ultrasound or radiography in PED | Initial diagnosis | Diagnosis at 6 months |
|---|---|---|---|---|
| 1 | 6 | Effusion in hip joint | TSH | Perthes’ disease |
| 2 | 2 | No imaging test | TSH | Hidden tibia fracture |
| 3 | 10 | Effusion in hip joint | TSH | Osteoid osteoma of the acetabulum |
| 4 | 2 | No imaging test | Osteomuscular pain | TSH |
| 5 | 4 | Effusion in hip joint | Septic arthritis | TSH |
| 6 | 9 | Effusion in hip joint | Septic arthritis | Rheumatic fever |
| 7 | 1 | Effusion in knee joint | Septic arthritis | JIA |
| 8 | 3 | Normal hip ultrasound scan | Osteomyelitis | Viral arthritis due to EBV |
| 9 | 10 | Normal hip ultrasound scan and radiography | Septic arthritis | TSH |
JIA: juvenile idiopathic arthritis; TSH: transient synovitis of the hip; PED: Paediatric Emergency Department; EBV: Epstein–Barr virus.
Diagnoses in PED and 6 months after consulting due to lameness.
| Diagnosis | PED diagnosis | Diagnosis after 6 months | ||
|---|---|---|---|---|
| n=146 | % | n=146 | % | |
| Inflammatory | ||||
| TSH | 84 | 57.53 | 84 | 57.53 |
| Post-infection reactive arthritis | 3 | 2.05 | 3 | 2.05 |
| Rheumatic fever | 0 | 1 | .68 | |
| JIA | 1 | .68 | 2 | 1.36 |
| Sacro-iliac arthralgia | 2 | 1.36 | 2 | 1.36 |
| Total | 62.69 | 62.69 | ||
| Infectious | ||||
| Septic arthritis | 5 | 3.4 | 1 | .68 |
| Viral arthritis | 0 | 1 | .68 | |
| Osteomyelitis | 1 | .68 | 0 | |
| Total | 3.38 | 1.36 | ||
| Tumour | ||||
| Tumour | 0 | 1.36 | 1 | .68 |
| Leukaemia | 2 | 2 | 1.36 | |
| Total | 1.36 | 2.04 | ||
| Orthopaedic | ||||
| Perthes’ disease | 1 | .68 | 2 | 1.36 |
| Epiphysiolysis | 1 | .68 | 1 | .68 |
| Total | 1.36 | 2.04 | ||
| Others | ||||
| Abdominal pain | 4 | 2.73 | 4 | 2.73 |
| Hidden fracture | 0 | 1 | .68 | |
| Osteomuscular pain | 42 | 28.76 | 41 | 28.08 |
| Total | 31.49 | 31.49 | ||
JIA: juvenile idiopathic arthritis; TSH: transient synovitis of the hip; PED: Paediatric Emergency Department.
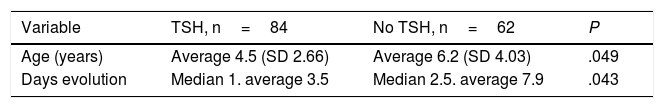
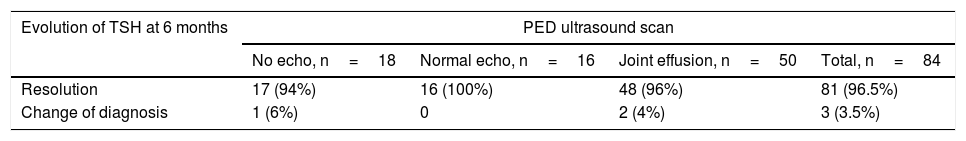
The 84 patients with a final diagnosis of TSH were analysed independently, and they were compared with the children with other diagnoses (Table 5). 77% of the children were aged from 3 to 10 years old, 18 patients were under the age of 3 years old and one patient was older than 10 years old. The cases of TSH were not associated with any season of the year, and they were constantly distributed over all 12 months. An ultrasound scan was performed on the majority of the children diagnosed with TSH (n=66/84, 78.57%) although TSH was also diagnosed without any imaging test and in the absence of synovitis in the ultrasound scan in 18 of them (21.04%) (Table 6).
Comparative table of PED variables in the patients finally diagnosed TSH or no TSH.
| Variable | TSH, n=84 | No TSH, n=62 | P |
|---|---|---|---|
| Age (years) | Average 4.5 (SD 2.66) | Average 6.2 (SD 4.03) | .049 |
| Days evolution | Median 1. average 3.5 | Median 2.5. average 7.9 | .043 |
| n (%) | n (%) | P | |
|---|---|---|---|
| Age 3–10 years old | 65 (77%) | 37 (59%) | .021 |
| Referred by paediatrician | 17 (20.24%) | 10 (16.13%) | .527 |
| Fever (>38°C) and/or systemic symptoms | 7 (8.33%) | 11 (17.74%) | .087 |
| No weighting | 22 (26.19%) | 15 (24.19%) | .784 |
| Localisation of pain | 55 (65.48%) | 36 (58.06%) | .361 |
| Previous respiratory infection | 33 (39.20%) | 29 (46.77%) | .366 |
TSH: transient synovitis of the hip; PED: Paediatric Emergency Department.
PED ultrasound scan result in children with TSH and evolution at 6 months.
| Evolution of TSH at 6 months | PED ultrasound scan | |||
|---|---|---|---|---|
| No echo, n=18 | Normal echo, n=16 | Joint effusion, n=50 | Total, n=84 | |
| Resolution | 17 (94%) | 16 (100%) | 48 (96%) | 81 (96.5%) |
| Change of diagnosis | 1 (6%) | 0 | 2 (4%) | 3 (3.5%) |
TSH: transient synovitis of the hip; PED: Paediatric Emergency Department.
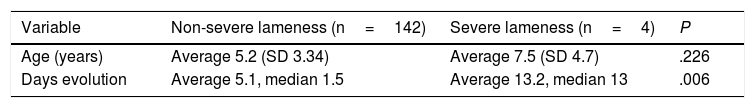
The variables corresponding to the children with a final diagnosis of severe lameness were also analysed independently, and their data were compared with those of the other patients (Table 7).
Comparative table of PED variables of the patients finally diagnosed severe or non-severe lameness.
| Variable | Non-severe lameness (n=142) | Severe lameness (n=4) | P |
|---|---|---|---|
| Age (years) | Average 5.2 (SD 3.34) | Average 7.5 (SD 4.7) | .226 |
| Days evolution | Average 5.1, median 1.5 | Average 13.2, median 13 | .006 |
| n (%) | n (%) | P | |
|---|---|---|---|
| Referred by paediatrician | 24 (16.9%) | 3 (75%) | .003 |
| Fever (>38°C) and/or systemic symptoms | 16 (11.27%) | 2 (50%) | .020 |
| No weighting | 34 (23.94%) | 3 (75%) | .021 |
| Localisation of pain | 89 (62.68%) | 2 (50%) | .601 |
PED: Paediatric Emergency Department.
Although there are works that set protocols involving multiple complementary examinations for children with severe lameness,2,10,11 and even puncture-aspiration of all hip effusions,12,13 TSH is the most frequent cause of lameness in the PED. This pathology is benign and self-limiting, and it mainly affects children aged from 3 to 10 years old.14
As could be expected, in our study TSH was the most frequent diagnosis in the PED, with a good result 6 months after the episode: there were few errors in the initial diagnosis, the benign cases resolved and all of the severe cases were detected.
TSH was diagnosed based on the detection of effusion by ultrasound scan, after normal ultrasound scan results and without ultrasound scan. The use or result of ultrasound scan did not change therapeutic attitude: all of the patients were prescribed rest and anti-inflammatory medication, so that the lameness was resolved in a similar way in children diagnosed clinically or by ultrasound scan. Only one patient who was not subjected to ultrasound scan was erroneously diagnosed TSH. He was a 2-year-old boy with a fracture arising from his first steps. On the contrary, the opposite occurred in 2 cases; the presence of effusion led to the erroneous diagnosis of TSH: a 6 year old boy with Perthes’ disease, and another aged 10 years old who was diagnosed osteoid osteoma of the acetabulum by computed tomography scan.
The lack of effusion in ultrasound scans of children with TSH may be explained by early stage TSH with a very small amount of fluid that may go unnoticed. The origin of the lameness may also another benign cause such as osteomuscular pain. In a broad prospective study of children clinically diagnosed TSH (471/500 cases of lameness, 94%) Miralles et al.15 observed effusion in only 46% of cases. They followed up 202 patients, of whom only 9 (4%) had a different diagnosis, although this was after an abnormal clinical course.
Although ultrasound scan is a useful technique in ruling out or confirming the presence of effusion in a joint, it does not irradiate patients and is available in the majority of hospitals. If it does not detect effusion this does not always justify performing other tests, while the presence of effusion in a joint does not discriminate the cause of the same. The correct diagnosis arises from the associated clinical symptoms, analytical data and evolution.16 In 1999 Kocher et al.17 developed a model that was validated in 200418 to differentiate septic arthritis from TSH in case of effusion in a joint. This includes 4 parameters: fever, rejection of or inability to place weight on the leg, globular sedimentation rate ≥40mm/h and leukocytes >12,000mm−3. In recent years publications have indicated that reactive C protein is a factor that is strongly associated with the diagnosis of septic arthritis.19 The function of ultrasound scan here is to confirm the presence of effusion within a joint and, if indicated, to guide the puncture-aspiration of fluid from the joint for analysis.
Radiography was not found to be a worthwhile diagnostic test, as it only detected pathology in 8 children. It was requested for the older children as well as when the initial suspicion was of a bone lesion. Baskett et al.20 studied 306 children aged 2–11 years old to evaluate the diagnostic worth of routine hip radiography in children who were seen in an Emergency Department for non-traumatic recent hip pain. They found that in those younger than 9 years old this technique was not useful, while in those over the age of 9 years old it could be useful in ruling out epiphysiolysis of the femoral head. In this study, fever, not weighting the leg while walking and age were the main predictors for severe pathology.
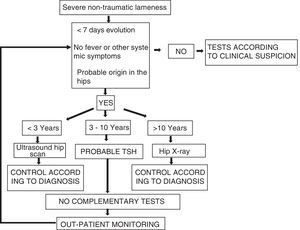
When the variables are analysed according to the final diagnoses it is found that lameness over a short period of time, above all less than one week, the absence of fever and/or systemic symptoms in children aged from 3 to 10 years old indicate the most frequent diagnosis of TSH. On the contrary, prolonged lameness, fever or not weighting the limb while walking, showing major pain, are associated with severe lameness.
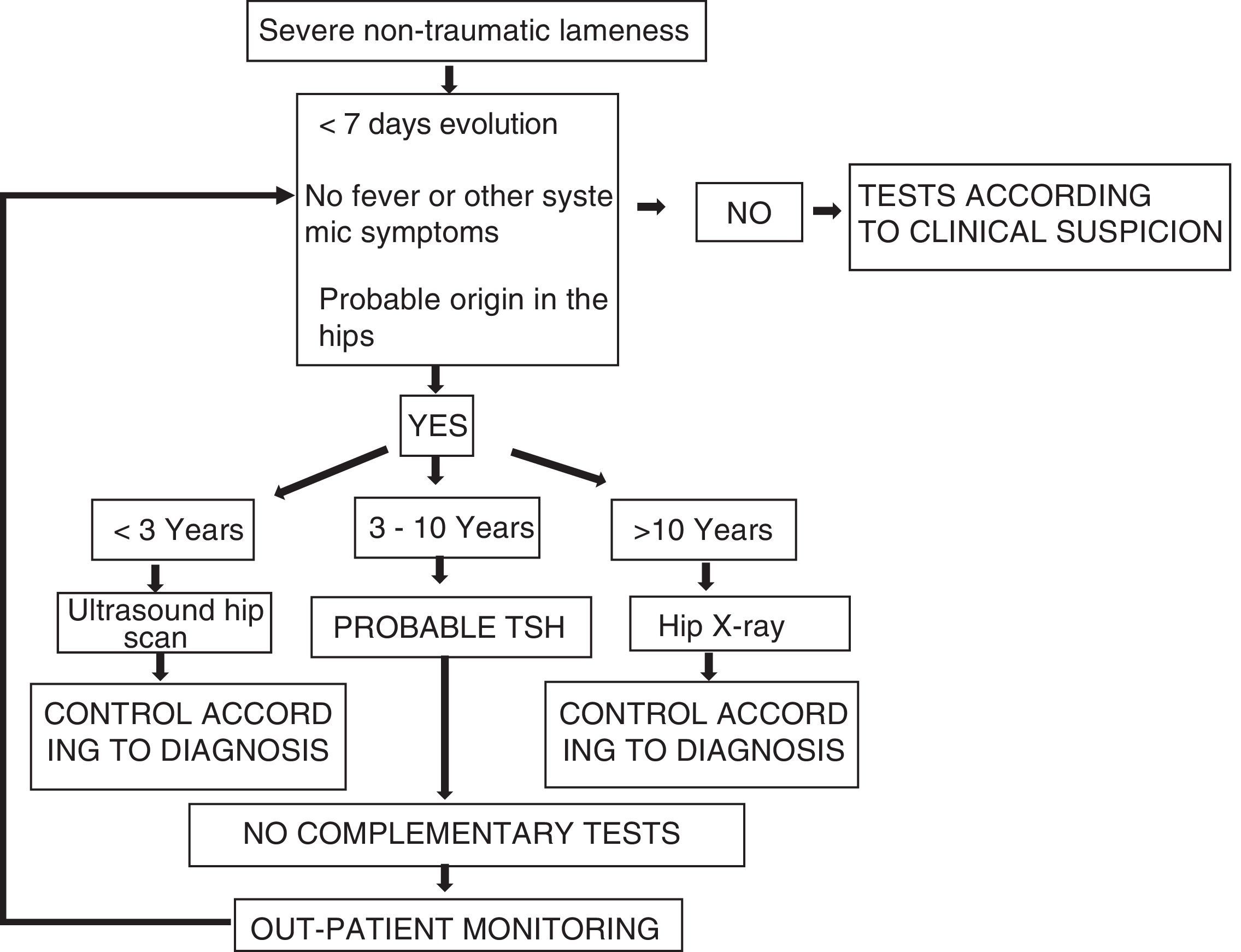
Based on our results it is possible to ask whether lameness is due to the hip by using a simple initial algorithm. This makes it possible to make the clinical diagnosis of TSH outside the typical age using an initial imaging test: an ultrasound scan in children <3 years old, or radiography in children >10 years old (Fig. 2). In any case, a systematic and individualised approach together with the thoughtful use of imaging tests and analysis form the basis for correct clinical evaluation.21
ConclusionsIn the majority of cases the cause of lameness has its origin in the hips, and TSH is the most frequent diagnosis. When faced with a case of non-traumatic lameness with a probable origin in the hips, in a child aged from 3 to 10 years old, without fever and/or systemic symptoms and with an evolution of less than one week, it is possible to make a clinical diagnosis of TSH and monitor the case on an out-patient basis. An ultrasound scan of the hips should only be performed in selected cases, rather than as a routine means of diagnosing TSH. Appropriate monitoring of the patient will permit the re-evaluation the subsequent indication or not for such examinations.
Level of evidenceLevel of evidence II.
Ethical responsibilitiesProtection of people and animal subjectsThe authors declare that no experiments were performed in human beings or animals for this research.
Confidentiality of dataThe authors declare that no patient data appear in this paper.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestsThe authors have no conflict of interests to declare and received no financing.
Please cite this article as: Lázaro Carreño MI, Fraile Currius R, García Clemente A. Cojera no traumática en Urgencias de Pediatría. Epidemiología, valoración y resultados. Rev Esp Cir Ortop Traumatol. 2018;62:127–133.