To establish the concordance between angulation of the femoro-tibial mechanical axis measured with X-rays and surgical navigation in both the pre and postoperative period after a total knee arthroplasty (TKA) was implanted.
Material and methodPre and postoperative measurements were analysed in 88 TKA of the same model and all performed with the same surgical navigation system. The mechanical frontal angle (MFA) and femoro-tibial anatomic angle were measured before and after the TKA. The angulation was digitally measured with a teleradiography. In the navigation, the femoro-tibial angle at rest, forced varus and valgus were registered and the average of these three measurements was calculated.
ResultsThe mean preoperative MFA measured on the radiograph was 4.55°. The mean of the same angle measured on the postoperative radiograph was 1.72°, (p=0.05). The mean of the MFA measured with navigation before TKA was 3.12° and after the implant with navigation was 0.53 (p=0.013). The concordance coefficient between the MFA in teleradiography and in navigation was 0.869 (p<0.001) preoperatively and 0.709 postoperatively (p=0.017).
ConclusionsWe found a strong concordance between radiographic and surgical navigation measurements of the MFA. This may imply that teleradiography is not necessary when using surgical navigation in TKA.
Conocer la concordancia entre el ángulo del eje mecánico femorotibial medido en radiografías y en navegación quirúrgica, tanto en el pre como en el postoperatorio al implantar una artroplastia total de rodilla.
Material y métodoSe analizaron las mediciones pre y postoperatorias en 88 artroplastias totales del mismo modelo y realizadas todas con el mismo sistema de navegación quirúrgica. Se valoró el ángulo frontal mecánico (AMFFT) y anatómico femorotibial pre y posquirúrgico. Para ello se utilizó una telerradiografía en bipedestación, donde se midió el ángulo mediante técnicas digitalizadas. En la navegación se recogió el ángulo femorotibial en reposo y en varo-valgo forzado, hallándose la media de estos 3 valores.
ResultadosLa media del AMFFT preoperatorio medido en la radiografía fue 4,55°. La media del mismo ángulo medido en la radiografía postoperatoria fue de 1,72°, con diferencias estadísticamente significativas. La media del AMFFT medido con la navegación antes de iniciar la técnica quirúrgica fue de 3,12° y tras el implante con navegación fue de 0,53°, también con diferencias estadísticamente significativas (p = 0,013). El coeficiente de concordancia entre el AMFFT preoperatorio en telerradiografía y en navegación fue de 0,869 (p < 0,001) y en el postoperatorio de 0,709 (p = 0,017).
ConclusionesHemos encontrado una fuerte concordancia en el AMFFT entre la medición con radiografías y con navegación quirúrgica. Ello puede suponer que no es necesaria la realización de una telerradiografía cuando se utiliza navegación en el implante de una artroplastia total de rodilla.
The best total knee arthroplasty (TKA) outcomes obtained in the last few decades may be attributed to the improvement in materials, to perfectionism of surgical instrumentation, study and control of ligament balance and correct alignment obtained by following the mechanical axis of the limb. There is no doubt that the improvement in instrumentation has led to gross errors in this alignment only occurring under exceptional circumstances, but it is known that a high percentage of TKA present pathological deviations of the femoro-tibial axis1 without this being directly related to the surgeon's expertise.
The use of teleradiography under load2 is recommended for measurement of the mechanical axis of the limb. This method has disadvantages: firstly because the patient is submitted to radiation, availability may be limited and there are also difficulties in following the correct technique in the radiology department on not making appropriate assessment of the leg rotation.3
The introduction of surgical navigation for the TKA implant may lead to an individualised surgery with better control of bone slices, size and position of arthroplasty and ligament balance. Better control of surgical procedures is expected to lead to an improvement in long-term clinical outcome and above all, in major deformities or complex knees, the surgeon is more secure in actions and skill.4,5
In the preoperative navigation technique without images, through collection and palpation of anatomical reference points the mechanical axis of the limb may be visualised pre-and-post operatively and is reflected on the system's computer file. It may be considered that this measurement would replace that of radiographic measurement, due to its advantages with regards to radiation and cost. There is no consensus in this regard in published literature and the aim of our study is to demonstrate that pre-and-postoperative teleradiography for finding the mechanical axis of the limb is not necessary when a TKA with navigation is introduced.
Material and methodsProspective study. The series comprised 88 TKA implanted with navigation in 82 patients (6 bilateral cases); 23 cases were male and 65 female. Mean age was 72 (SD: 9.07). The mean body mass index was 31 (SD: 3.5) in 34 cases in the initial radiography we observed. The femoro-tibial mechanical frontal angle (FTMFA) and in varus over 3°, in 31 a normal axis and in 23 an angle in valgus over 3°. The diagnosis in all cases was tricompartmental gonarthrosis in patients who had previously been administered physical and pharmacological treatment without success. Exclusion criteria were considered to be the absence of pre or postoperative radiographic measurement and difficulty in measuring the angles in teleradiography due to rotation defects.
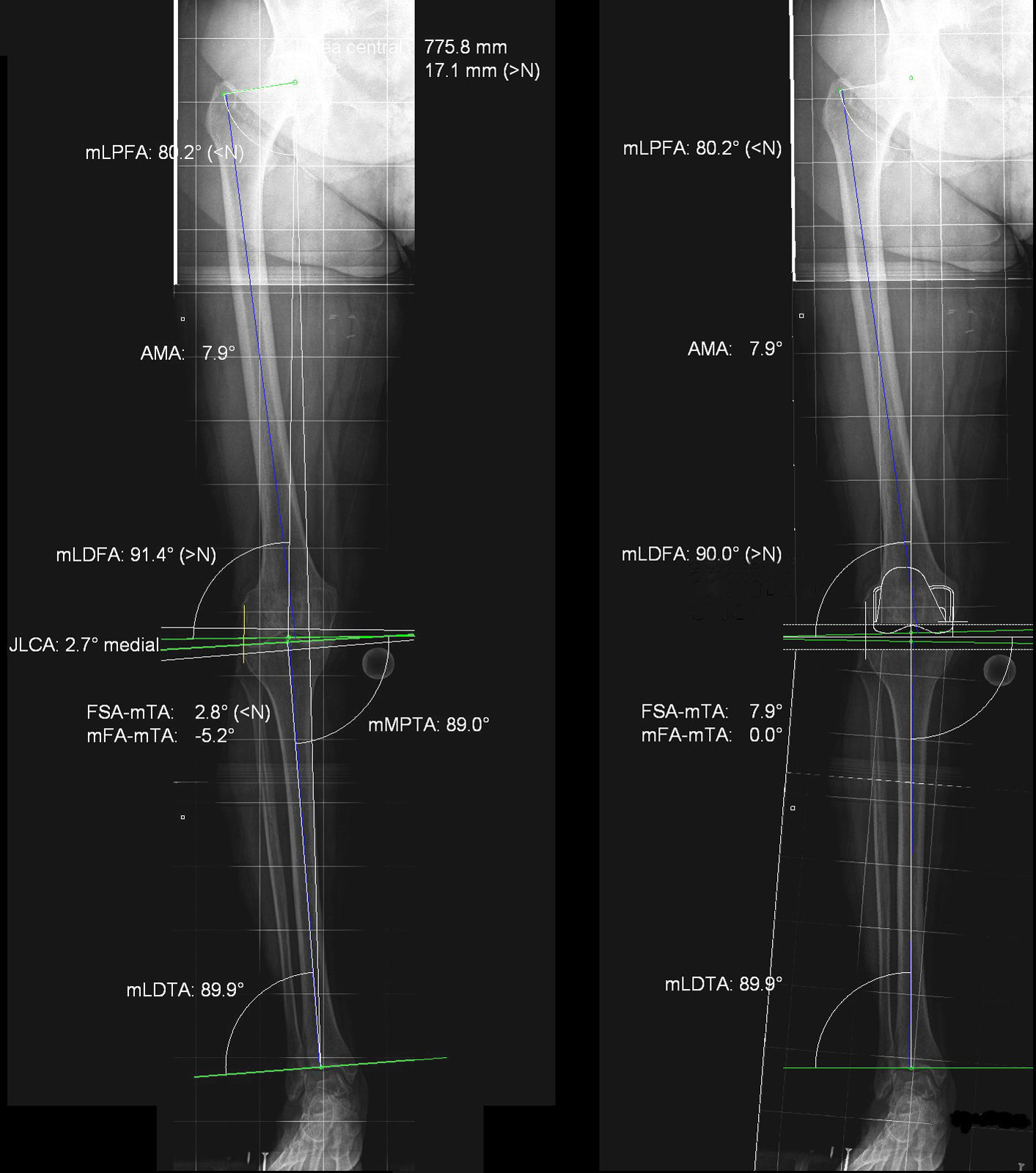
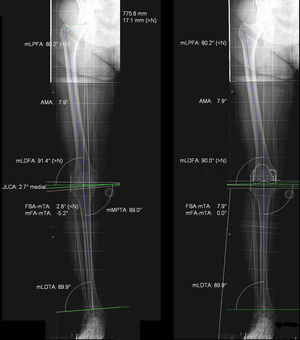
The patients adhered to the same preoperative protocol and similar surgical techniques were used. They were given an appointment in the radiology department one month prior to intervention and one month after the TKA implant. A teleradiography was performed which included hip, knee and ankle, in bipodal support, with projection focused on the knee. Teleradiographies with positional defects through alterations in rotation of the limb or knee flexion were rejected for this study. A calibrator was positioned at thigh height to take digitalised radiographic measurements. The mechanical frontal angle (MFA) and femoro-tibial anatomic angle (FTAA) were measured before and after the TKA. The measurement was made by 2 authors from this study (AAS and SR), who had considerable experience in preoperative planning. The Impax 6.3.1.2813 (Agfa Healthcare N.U. Montsel, Belgium and Agfa-Orthopaedic Tools Version 2.06) programme was used. Patients were informed about the aim and characteristics of the study through a specific informed consent form designed for this study. Authorisation was obtained from the regional ethical committee. This study formed part of the project by the Instituto de Salud Carlos III for biomedical research (Fig. 1).
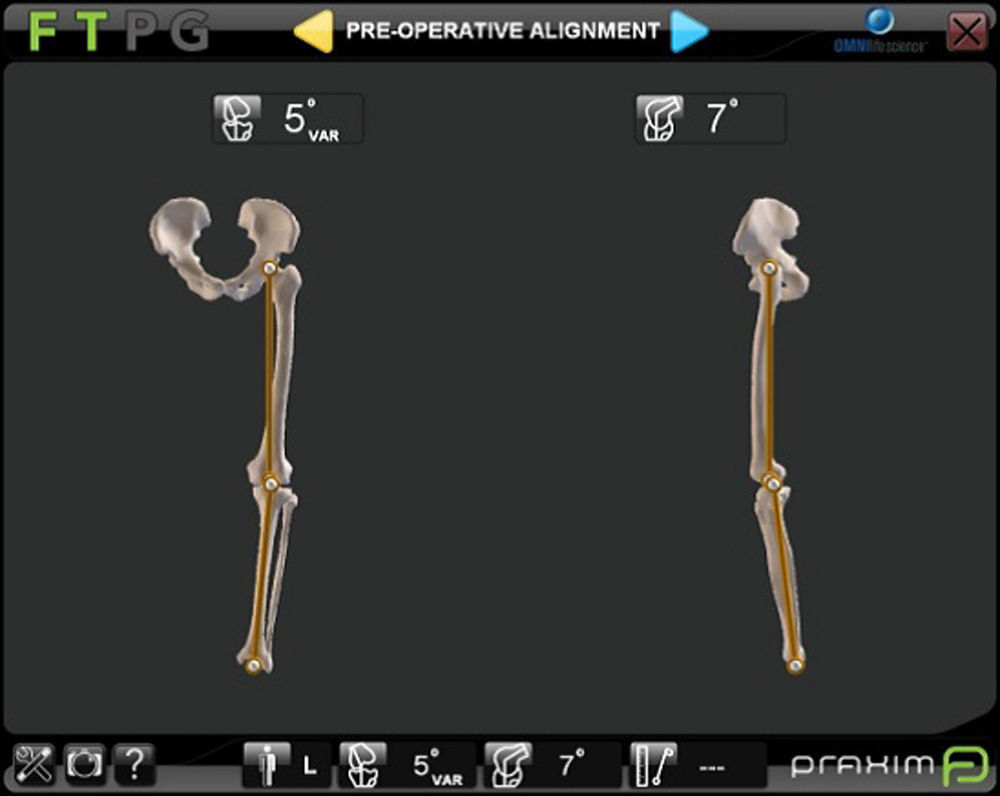
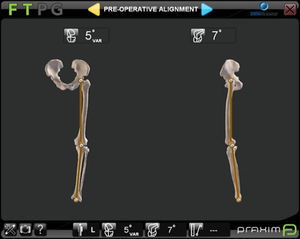
All the arthroplasties implanted were of the Apex (Omnilife Science, Massachusetts, U.S.A.) model. For navigation the Nano Station (Total Knee Surgetics, Praxim, S.A. La Tronche, France) system was always used and they were implanted by 2 surgeons (DHV and ANF). The navigator used contains a panel PC, a CD-ROM reader/recorder, a card reader and an infra-red camera. Operating it is based on ergonomic, touch screen exterior interfaces and a double order pedal. After data collection through a pointer the preoperative femoro tibial alignment was obtained (Fig. 2). Three angles were taken: at rest and in forced varus and valgus stress, with the mean of the 3 being taken. On termination of the arthroplasty implant this same information was collected through the navigator screen.
Data were statistically analysed using the general lineal model of repeated measurements (GLM) and the concordance analysis by intraclass correlation (ICC). The GLM means that differences in results may be evaluated in one or more quantitative variables between different groups and in seried measurements over time. Analysis is paired, and the change in each individual to itself is always considered. The GLM leads to evaluating the effect of interaction of one or more of the variables studied.
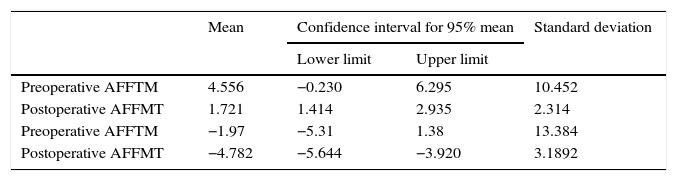
ResultsThe mean preoperative FTMFA measured on the radiograph was 4.55° (SD: 10.45). The mean of the same angle measured on the postoperative radiograph was 1.72° (SD: 2.31). Significant statistical differences were found between both angles (p=0.05) (general lineal model). The mean preoperative AAFFT on the radiograph was −1.97° (SD: 13.38), and postoperatively was −4.78° (SD: 3.19) (Table 1). The difference of the means between the FTMFA and AAFFT preoperatively was therefore 2.58° and postoperatively was −3.06°.
Pre and postoperative mechanical femoro-tibial and anatomical angle, measured in teleradiography.
| Mean | Confidence interval for 95% mean | Standard deviation | ||
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Preoperative AFFTM | 4.556 | −0.230 | 6.295 | 10.452 |
| Postoperative AFFMT | 1.721 | 1.414 | 2.935 | 2.314 |
| Preoperative AFFTM | −1.97 | −5.31 | 1.38 | 13.384 |
| Postoperative AFFMT | −4.782 | −5.644 | −3.920 | 3.1892 |
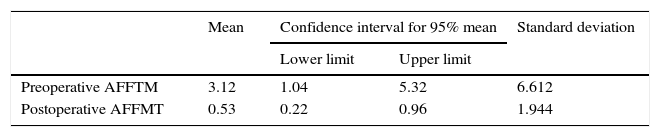
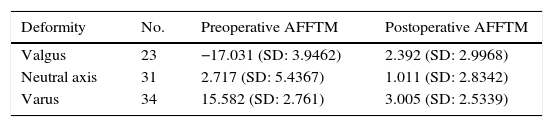
The FTMFA mean measurement with navigation before initiating the surgical technique was 3.12° (SD: 6.61) and after implant with navigation was 0.53° (SD: 1.94) (p=0.013) (general lineal model) (Table 2). When preoperative deformity of the mechanical axis was above 3° (in varus or valgus) the improvement was greater than in knees with neutral axes with no deformity (<3°) (p<0.001) (general lineal model) (Table 3).
Modification of the AFFTM depending on previous deformity (±3°).
| Deformity | No. | Preoperative AFFTM | Postoperative AFFTM |
|---|---|---|---|
| Valgus | 23 | −17.031 (SD: 3.9462) | 2.392 (SD: 2.9968) |
| Neutral axis | 31 | 2.717 (SD: 5.4367) | 1.011 (SD: 2.8342) |
| Varus | 34 | 15.582 (SD: 2.761) | 3.005 (SD: 2.5339) |
SD: standard deviation.
The concordance coefficient between preoperative FTMFA on the radiograph and in navigation was 0.859 (95% CI: 0.825–0.936) (CCI: p<0.001) and postoperative was 0.709 (95% CI: 0.678–0.896) (CCI: p=0.017).
DiscussionIn recent years there have been controversies regarding the relevance of reproducing the prior axis of the patient's limb or to search for a neutral axis of ±3°. Although this discussion is still applicable, as is the need to find the cinematic axis rather than the mechanical one, up until now it appears to have been proven that obtaining neutral mechanical axis or lightly valgus6,7 must be an essential aim in knee implants.
For this, finding the mechanical axis of the limb before and after a KA is considered as an essential measure to assess the quality and results of the technique. Radiography of the knee alone does not lead to discovery of the mechanical axis of the limb. In a recent study8 it was confirmed that in the preoperative study there was discordance in the mechanical axis measured on the teleradiograph or in the X-rays of the knee of 14%, which increased to 33% in the postoperative measurement. The knee X-ray can measure the anatomical axis, but not the mechanical one, and protocols and clinical guides should therefore be excluded from the request for this radiograph if we wish to know the mechanical axis before or after TKA.
Notwithstanding, measuring the mechanical axis in teleradiography is subject to errors particularly due to inaccurate positioning of the leg, defects in radiographic projection or flexion of the knee. The greatest difficulty is in achieving correct rotation of the knee, and formulas have even been described to achieve it, supporting the head of the fibula in association with the tibia.3,9 Correct rotational positioning will show the head of the fibula superimposed exactly 1/3 over the tibia. External rotation is considered if the head of the fibula is superimposed over 1/3 over the tibia. A marked external rotation show a superimposition above 2/3 and an exaggerated internal rotation will show the head of the fibula as completely visible (Fig. 3). In our series these misalignments were avoided by always positioning the foot at 10° of external rotation and discarding the radiographs where the ball joint was not centred and the head of the fibula superimposed at 1/3 to the tibia. Other possible causes of errors are an inappropriate radiographic projection (it has to be perpendicular to the articular space between the joint and the femoral condyles) or the wrong positioning of the calibrator. This calibrator, 25mm in diameter, must be attached to the skin of the patient when performing the radiography and must be positioned close to the knee. There is discussion in the literature on the convenience of performing the radiograph of one or both lower limbs.10
The difference between the mechanical and anatomical axis of the femur is around 7±2°, which does not occur in the tibia, where the mechanical and anatomical axis are parallel and similar. The femoro tibial axis crosses the knee at 5–8mm medial to its centre, which is called mechanical axis deviation. There is also a physiological deviation in valgus between the anatomical axis of the femur and the tibia.11 According to that described in the literature the anatomical femoro tibial axis forms an angle of 6.8±1.4° and the mechanical one of 1.2±2°.12,13 In our series the difference between the anatomical and mechanical axis of the limb had similar figures to those reported in the references. After the TKA implant the mechanical axis was regularised both in measurements with teleradiography and in navigation.
Computer-assisted surgery has demonstrated its use with regards to the best mechanical axis found.14 One reported disadvantage in navigation is the imprecision of references. In contrast to several studies we believe that data collected in navigation is precise and independent from the surgeon's expertise.15 This technique provides better clinical results in the medium and short term,16 and although these findings have not yet been corroborated long term, it is expected that better alignment in all axes, a better ligament balance and finally personalised surgery such as that performed with navigation, would lead to a better outcome and better implant survival. A recent study reported survival of 87% in standard surgery compared with 98% in navigation at 10 years,17 and in another18 a lower number of reviews from misalignment were reported when surgery was computer-assisted. In our series a FTMFA proximal to neutral axis was obtained with navigation.
Great controversy exists in the literature regarding concordance between the pre and post operative mechanical axis measured with radiographs and navigation. Several authors19,20 do not find this and attribute it to the fact that the mechanical axis cannot be the same in bipedestation, as performed by teleradiography, as in navigation with the patient on the surgical table. In other articles8,21 this relationship is found provided that the radiography has been correctly performed, especially regarding the limb rotation since it is known that in almost 10% of radiographies an unacceptable rotation of the leg is shown, which alters the measurement of the mechanical limb axis.22 Our results show an acceptable concordance between the FTMFA measurement in teleradiography and in navigation. We attribute this fact to several factors. Firstly, with the accurate positioning of the limb, which has forced us to exclude erroneous X-rays. Secondly, because we have found the FTMFA mean in navigation using a resting position and in forced varus–valgus position. This manoeuvre, which we systematically practice on initiating navigation for assessing the need for ligament liberation, also offers the advantage of discovering real FTMFA.
As a result of our study we believe that concordance between measurements taken in the radiography and in navigation lead to the prevention of systematic teleradiography in patients who will or who have undergone surgery with navigation technique. This restriction would result in reducing costs, lowering radiations for the patient and avoiding overburdening radio diagnostic services.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjectsThe authors declare no experiments have been performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare they have adhered to the protocol of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflict of interests to declare.
This study was conducted with aid from the Sanitary Research Fund, FIS (Instituto de Salud Carlos III) with FEDER funds (PI12/01098).
Please cite this article as: Hernandez-Vaquero D, Noriega-Fernandez A, Suarez-Vazquez A, Roncero-Gonzalez S, Sierra-Pereira AA, Gil-Martinez L, et al. Alineación frontal en la artroplastia total de rodilla. Estudio comparativo entre medición radiográfica y con navegación quirúrgica. Rev Esp Cir Ortop Traumatol. 2017;61:313–318.