The aim of this study was to assess the rate of discrepancies in medication reconciliation on admission patients in a trauma unit, and identifying potential risk factors associated with these discrepancies.
Materials and methodsA cross-sectional, observational study was carried out to identify reconciliation errors in a tertiary hospital during the period from May 1 to July 16 of 2012. Medication history of the patient was compared with home medication data collected on admission, to identify reconciliation errors. These were classified according to the type and severity of the discrepancies. Statistical analysis by logistic regression was performed, using the presence of discrepancies as dependent variable.
ResultsThe study included 164 patients, and reconciliation errors were found in 48.8%, of which 14.4% were considered highly relevant. Around two-thirds (66.7%) of the patients admitted to the emergency department showed unjustified discrepancies compared to 44.8% in scheduled patients. In total, 153 reconciliation errors were identified, being omitted drug the most frequent type of discrepancies (72%). The risk of discrepancies increases by 33% for each drug added to the usual home treatment.
ConclusionThis study demonstrates the lack of quality in home medication recording in patients admitted to the trauma unit.
El objetivo del estudio fue evaluar la tasa de discrepancias en la conciliación de la medicación realizada al ingreso de los pacientes en una Unidad de Traumatología, identificando los posibles factores de riesgo asociados a los errores de conciliación.
Material y métodosSe trata de un estudio observacional transversal realizado en un hospital de tercer nivel durante el periodo comprendido entre el 1 de mayo y el 16 de julio del 2012, en el que se elaboró un listado del tratamiento domiciliario del paciente contrastándose con la historia farmacoterapéutica recogida al ingreso en dicha unidad, para identificar los errores de conciliación. Estos se clasificaron en función del tipo y la relevancia de la discrepancia. Se realizó un análisis estadístico por regresión logística, utilizando como variable dependiente la existencia de discrepancias.
ResultadosCiento sesenta y cuatro pacientes fueron incluidos en el estudio, hallándose errores de conciliación en el 48,8%, de las cuales el 14,4% fueron considerados muy relevantes. De los pacientes ingresados de forma urgente, el 66,7% presentó discrepancias frente al 44,8% en pacientes programados. En total, se identificaron 153 errores de conciliación, siendo el tipo más frecuente el de omisión de algún medicamento (72%). Se detectó que por cada fármaco añadido al tratamiento domiciliario habitual el riesgo de presentar discrepancias aumenta en un 33%.
ConclusiónEste estudio pone en evidencia la falta de exhaustividad en la recogida de la historia farmacoterapéutica de los pacientes al ingreso en la Unidad de Traumatología.
According to data from the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), medication errors represent one of the main causes of death and permanent loss of function among hospitalized patients. Nearly half of these errors are associated with care transition and changes in the person responsible for the patient, and it has been calculated that over 50% of admitted patients have at least 1 non-justified discrepancy between their medication prior to admission and hospital prescription. In Spain, it has been estimated that between 23% and 37.4% of adverse effects (AE) found among admitted patients are related to their medication.1–6
The reconciliation of medication is a formal and protocolized process which consists in compiling a full list of the medication taken by a patient prior to hospital admission and comparing it with the drug therapy prescription after a care transition, admission into hospital, following a change in the person medically responsible or upon hospital discharge. It has been proven as a key process in the prevention of AE caused by medication errors, as it has managed to reduce these errors by up to 70%.4,5
The present study aims to assess the collection of pharmacotherapeutic information carried out during hospital admission as a key step in medication reconciliation of patients at the Traumatology Service of a tertiary hospital. In addition, the study also aims to determine the possible risk factors associated to reconciliation errors.
MethodsThis was an observational and transversal study, conducted at the Traumatology Service of a tertiary hospital over the period between 1 May and 16 July, 2012.
We included all patients aged over 18 years of age who were admitted at the Unit during the study period, whose hospital stay was over 24h and who presented chronic drug treatment at the time of admission. We excluded those patients whose medical history could not be obtained.
Patients were analyzed 24–48h after admission, performing a review of their pharmacotherapeutic history prior to admission, using the following sources of information: clinical history of the patient, evaluation file completed upon admission by nursing staff, daily medication administration chart, recent discharge reports, Emergency Unit reports, information from prescriptions invoiced by the pharmacy office to the Aragon Healthcare Service through the Farmasalud® database and the Pharmacy Service Management program (FarmaTools®), where both the medication prescribed during admission and the records of dispensation of hospital medication through the unit to outpatients were reviewed.
Using the information gathered, we compiled a list of home treatment for each patient excluding drugs for the treatment of acute processes, such as antibiotics and analgesics, dietary supplements and medicinal plants, as well as all drugs not financed by the National Healthcare System, for which no information could be obtained. This list was compared with the treatments recorded upon admission at the Traumatology Service in order to identify any possible discrepancies.
For each patient, we registered the following variables: demographics (gender, age), information related to care (type of admission: scheduled/urgent, hospital stay), clinical (diagnosis, comorbidities), pharmacotherapeutic and reconciliation (professional carrying out the reconciliation, number, type and severity of the discrepancies, number of drugs involved in the discrepancies and therapeutic groups).
This study only analyzed non-justified discrepancies, that is, errors of reconciliation; classifying them based on the type of discrepancy (according to the criteria of the consensus document on terminology, classification and evaluation of medication reconciliation programs supported by the Spanish Society of Hospital Pharmacology, SEFH7).
The relevance of discrepancies was assessed according to the time when the medication should be reconciled after admission, following the recommendations of the Guide for reconciliation of medication at Emergency Services of the FASTER group. Relevance was graded as highly relevant (before 4h), moderately relevant (<24h) and scarcely relevant (after 24h).8
We conducted a descriptive analysis of the studied variables. Qualitative variables were presented as frequencies and proportions, whilst quantitative variables were presented using central tendency and dispersion measurements.
Qualitative variables were contrasted by applying the chi squared test. For the comparison of means we applied the Student t test or Mann–Whitney U test (according to the Kolmogorov–Smirnov normality test) for quantitative variables.
We also performed a logistic regression analysis for the multivariate study, applying the enter method. The adjustment of the model was verified through the Hosmer–Lemeshow test. As dependent variable we defined the presence or absence of non-justified discrepancies, and as independent variables we used those with clinical and/or statistical relevance.
We established a level of statistical significance of P<.05. Data analysis was carried out using the software package SPSS® statistics v15.0 (licensed to the University of Zaragoza).
ResultsA total of 221 patients were monitored during the study period, of which only 77.8% (n=172) were taking chronic medication. Thus, after applying the exclusion criteria we finally included a total of 164 patients. Of these, 58.5% (n=96) were female, and the mean age at the time of admission was 66.70±13.29 years.
Regarding the type of admission, 18.3% (n=30) of patients were admitted through the Emergency Service, whilst 81.7% (n=134) did so in a programmed manner from the Traumatology Service of the hospital. The mean stay at the Traumatology Service was 7.64±7.49 days (median: 7 days; range: 1–53 days).
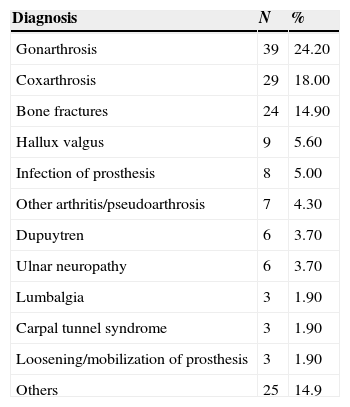
As shown in Table 1, the main diagnoses upon admission were gonarthrosis, coxarthrosis and bone fractures. Up to 93.1% (n=149) of patients presented some type of comorbidity, with mean 1.94±1.19 concomitant pathologies per patient, and with the most frequent being arterial hypertension (31.5%), dyslipidemia (14.8%) and diabetes mellitus (8%).
Diagnoses of the study population.
| Diagnosis | N | % |
|---|---|---|
| Gonarthrosis | 39 | 24.20 |
| Coxarthrosis | 29 | 18.00 |
| Bone fractures | 24 | 14.90 |
| Hallux valgus | 9 | 5.60 |
| Infection of prosthesis | 8 | 5.00 |
| Other arthritis/pseudoarthrosis | 7 | 4.30 |
| Dupuytren | 6 | 3.70 |
| Ulnar neuropathy | 6 | 3.70 |
| Lumbalgia | 3 | 1.90 |
| Carpal tunnel syndrome | 3 | 1.90 |
| Loosening/mobilization of prosthesis | 3 | 1.90 |
| Others | 25 | 14.9 |
Reconciliation of medication upon admission at the Traumatology Service was carried out by the nursing staff in 80.4% (n=127) of cases. Out of the patients with a scheduled admission, 93.9% (n=123) were reconciled by nursing staff, whereas 85.2% (n=23) of emergency patients were reconciled by physicians (P<.001).
Reconciliation upon admission registered a total of 600 drugs, with a mean 3.66±2.66 drugs per patient. However, after analyzing the different data sources, the mean number of drugs as home treatment per patient increased to 4.59±3.00 (total: 753 drugs). In total, 56.3% (n=76) of patients were habitually taking 5 or more drugs, with patients older than 65 years taking the most (mean: 5.17±2.96 vs 3.65±2.84; P<.001).
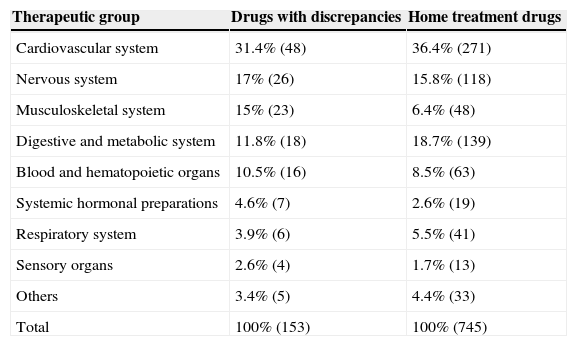
As shown in Table 2, in general, drugs targeting the cardiovascular system were the most common in home treatment among the studied population, present in up to 75% (n=123) of patients, followed by those acting on the metabolism/digestive system (57.3% [n=94]) and the nervous system (42.1% [n=69]).
Therapeutic groups of medication with discrepancies and home medication.
| Therapeutic group | Drugs with discrepancies | Home treatment drugs |
|---|---|---|
| Cardiovascular system | 31.4% (48) | 36.4% (271) |
| Nervous system | 17% (26) | 15.8% (118) |
| Musculoskeletal system | 15% (23) | 6.4% (48) |
| Digestive and metabolic system | 11.8% (18) | 18.7% (139) |
| Blood and hematopoietic organs | 10.5% (16) | 8.5% (63) |
| Systemic hormonal preparations | 4.6% (7) | 2.6% (19) |
| Respiratory system | 3.9% (6) | 5.5% (41) |
| Sensory organs | 2.6% (4) | 1.7% (13) |
| Others | 3.4% (5) | 4.4% (33) |
| Total | 100% (153) | 100% (745) |
Up to 48.8% (n=80) of the patients included in the study presented at least 1 non-justified discrepancy between the medication registered upon admission at the Traumatology Service and their chronic home treatment. We noted that belonging to the group of advanced age patients (>65 years) significantly influenced the presence of discrepancies (OR=1.92 [95% CI: 1.01–3.66]).
We also noted that those patients who presented ≥5 drugs in their usual treatment presented discrepancies in 67.1% (n=51) of cases, compared to 33% (n=29) among those whose home treatment included less than 5 drugs (OR=4.15 [95% CI: 2.16–7.97]).
On the other hand, 66.7% (n=20) of the patients who were admitted through the Emergency Service presented some discrepancy in the reconciliation of medication upon admission, whilst patients with scheduled admissions presented discrepancies in 44.8% (n=60) of cases (OR=0.405 [95% CI: 0.176–0.932]). Regarding patients who were reconciled by nursing staff, 42.5% (n=54) presented non-justified discrepancies, compared to 71% (n=22) of those reconciled by medical staff (OR=3.3 [95% CI: 1.410–7.744]).
In total, we identified 153 reconciliation errors, representing a mean value of 1.91±1.093 discrepancies per patient. The most frequent error was omission of a necessary drug for the patient (72%), followed by commission (11%) (i.e. starting a new treatment which the patient was not following before admission with no clinical justification), incomplete prescription (9%), different dosage (5%), different frequency (2%) and wrong medication (1%).
Regarding the relevance of the discrepancies, 14.4% of them (n=22) were considered highly relevant, where the drugs should have been reconciled in the first 4h after admission, 50.3% (n=77) moderately relevant, where the drugs should have been reconciled in the first 24h after admission, and 35.3% (n=54) scarcely relevant, where the drugs should have been reconciled at some point during admission.
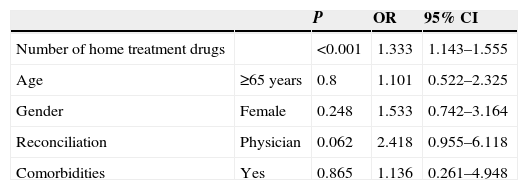
Lastly, in order to determine the influence of the different variables on the presence of discrepancies, we conducted a logistic regression analysis, with the best model showing an explanatory capacity of 23.5% (patients included in the analysis: 154). As dependent variable we used the existence of discrepancies, whilst the independent variables were: gender, age group, professional who carried out the reconciliation, presence of comorbidities and number of drugs being taken as habitual treatment, considering the latter as a quantitative variable. As shown in Table 3, an increasing number of drugs in the usual home treatment of patients was associated with a significantly higher risk of presenting discrepancies, with the probability of presenting a discrepancy increasing by 33% for each drug added to the usual treatment.
Multivariate analysis.
| P | OR | 95% CI | ||
|---|---|---|---|---|
| Number of home treatment drugs | <0.001 | 1.333 | 1.143–1.555 | |
| Age | ≥65 years | 0.8 | 1.101 | 0.522–2.325 |
| Gender | Female | 0.248 | 1.533 | 0.742–3.164 |
| Reconciliation | Physician | 0.062 | 2.418 | 0.955–6.118 |
| Comorbidities | Yes | 0.865 | 1.136 | 0.261–4.948 |
95% CI: 95% confidence interval; OR: odds ratio; P: statistical significance.
Dependent variable: presence of discrepancies (yes).
Nagelkerke R squared=0.23.
Published studies on discrepancies in reconciliation of medication are not plentiful, mainly conducted upon hospital admission. The majority, both national and international, were carried out at medical services, with a different patient profile (more advanced age and higher rate of urgent admissions) or else including only patients aged over 65 years.9–14
There are very few national studies which include only surgical and/or traumatology patients with a similar gender and age distribution (60–70% females and 61–75 years mean age) to those included in the present study, where the majority of patients aged over 65 years were female. This fact could be explained by the higher risk by females of presenting bone pathologies and arthropaties, particularly after the age of 50 years.15–18
The percentage of patients with home medication among the selected population confirmed the data obtained in previous studies, which showed that over 70% of surgical patients admitted to hospital were taking chronic medication. However, the mean drug intake per patient was lower than that registered in most studies (around 7 drugs/patient) conducted at medical services and including older patients.9,10,13,16
Regarding the rate of discrepancies in the reconciliation of medication, the published data varied widely: from 25.9% to 65% of patients with discrepancies, even reaching 70% of the prescribed medication. These differences could be due both to the different methodologies used and to the lack of homogeneity in terms of the criteria used to define discrepancy, as reported by a meta-analysis conducted in 2005.5,12,19
This variability was maintained in studies conducted in recent years in Spanish Traumatology and Orthopedic Surgery Services. Thus, the results of the present study, which showed that nearly half of patients presented reconciliation errors, agreed with those obtained by Franco et al. However, Moriel et al. obtained higher figures, finding discrepancies in up to 71% of patients, although it is worth noting that this last study only included patients aged over 65 years.15,17,20
The bivariate analysis showed that being over 65 years had a statistically significant influence on the presence of discrepancies. Some studies have established that age represents a risk factor for the presence of errors in the reconciliation of medication. However, other authors have argued that this fact is probably due to a higher susceptibility toward presenting comorbidities and, therefore, a greater consumption of medication, particularly if we take into account that, in our country, patients aged over 65 years consume between 25% and 50% of the total drugs prescribed.14,21 In this regard, it was observed that those patients who took ≥5 drugs presented a significantly higher number of discrepancies, as the increase in the number of drugs favored the risk of errors during pharmacotherapeutic anamnesis, particularly among patients with cognitive problems.6,9,13,14,22
Although emergency patients accounted for a minimal proportion of the total included, compared to other studies where such patients accounted for nearly 80% of the total, the higher rate of discrepancies observed among patients admitted through the Emergency Service could be justified by the idiosyncrasy of the Service itself: an environment with constant interruptions, where decisions need to be taken rapidly, with high healthcare pressure and with an acute problem as main priority. In addition, patients with programmed admissions often provide their usual home medication, which contributes to establish their current treatment with greater reliability.14,23 In any case, regardless of the type of admission, the guidelines recommend having an established circuit which specifies the person responsible and the process of gathering the pharmacotherapeutic history of patients, in order to avoid medication errors and guarantee healthcare continuity for patients, as required by JCAHO.6,8
We identified a total of 153 discrepancies in 80 of the patients included, a result which agreed with that obtained by other studies (1.3–2 reconciliation errors/patient).15,22 The profile of discrepancies was similar in most of the published studies, with omission being the most frequent error and, as shown in Table 2, the highest percentage of drugs involved in these errors affecting those acting on the cardiovascular system, accounting for 40% of home medication.9,15,16,24
Regarding the relevance of the discrepancies, these data were not comparable with the rest of studies, which show that 5.7% of reconciliation errors could have caused significant damage to patients, since most evaluate the severity of discrepancies according to the classification of the National Coordinating Council for Medication Error Preventions, based on the potential damage caused by these errors on the health of patients, whilst in our study they were classified according to the time of reconciliation (maximum time which should elapse from patient admission until a specific drug is reconciled), according to the consensus document on reconciliation of medication at emergency services.8–10,24
Lastly, coinciding with other studies conducted at emergency and medical services, after adjusting for the different variables through logistic regression we detected that polymedication was the only factor which affected the presence of discrepancies in a statistically significant manner.11,13
The results obtained showed some limitations due to the design of the study. The main such limitation was that being a transversal study made it impossible to know the time sequence of events. Another important limitation was the absence of a clinical interview with patients to obtain more detailed information (adherence to treatment, adverse effects, non-financed drugs).
This study reveals a lack of exhaustiveness during the elaboration of the pharmacotherapeutic history of patients upon admission at the Traumatology Service, highlighting this as a weakness of the healthcare system. The proportion of cases with non-justified discrepancies was greater among patients admitted through the Emergency Service.
It would be necessary to conduct studies with a larger number of patients in order to increase the statistical power, as other variables (age, gender, presence of comorbidities, type of admission and professional conducting the reconciliation) could also be possible risk factors associated to discrepancies during reconciliation. It would also be necessary to identify these factors in order to optimize the resources available and prioritize reconciliation programs with a greater impact on results for patient safety.
Furthermore, it would be interesting to conduct further studies which evaluated the effects of reconciliation errors, both in terms of the severity of adverse effects for patients and of their economic repercussions.
Level of evidenceLevel of evidence II.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Pascual O, Real JM, Uriarte M, Larrodé I, Alonso YM, Abad MR. Evaluación de la conciliación de la medicación en una Unidad de Traumatología. Rev Esp Cir Ortop Traumatol. 2015;59:91–96.