The anatomical anterior cruciate ligament (ACL) reconstruction attempts to, by reproducing the natural orientation of its fibres, achieve a better rotational stability of the knee. The aim of this paper is to quantify the anteroposterior and rotational laxity of the knee before and after an anatomic ligamentoplasty using the Orthopilot® navigation system as a supporting tool.
Material and methodWe describe the distinctive steps of Orthopilot® navigation as well as conducting a retrospective cross-sectional study on a cohort of 20 patients operated in our hospital for chronic primary ACL rupture from January 2010 to May 2011. The precise location of the tunnels was defined with the help of the navigator and the intra-articular landmarks and stability tests were performed in both the sagittal and axial planes.
ResultsIn our technique for anatomical ACL reconstruction placed the tibial tunnel at a mean distance of 16.8±4.92mm from the posterior cruciate ligament in a position that represented 44.1±4.35% of the total width of the tibial plateau. The average distance from the centre of the femoral tunnel to the posterior cortex of the lateral condyle was 7.89±2.78mm. Intra-operatively and before ACL reconstruction, the mean (±SD) anteroposterior movement, internal rotation and external rotation of the tibia at 30° position were 15.5mm (±5.11), 19° (±3.62) and 19.65° (±3.26), respectively. After reconstruction these values decreased to 5.6mm (±1.72°), 12.17° (±3.76) and 16.9° (±4.42), respectively.
ConclusionsThe use of navigation systems supporting the surgery allows the systematic positioning of bone tunnels and standardises the procedures for the desired reconstruction. ACL reconstruction using the technique described, improves the anteroposterior and rotational stability compared to preoperative status, to a stability state that could be considered physiological according to current scientific knowledge.
La técnica de reconstrucción anatómica del ligamento cruzado anterior (LCA) persigue, reproduciendo la orientación nativa de sus fibras, alcanzar una mejor estabilidad rotacional en la rodilla. El objetivo principal del presente trabajo es la evaluación cuantitativa intraoperatoria, mediante el uso del sistema de navegación de Orthopilot®, de la laxitud anteroposterior y rotacional de la rodilla antes y después de una ligamentoplastia anatómica.
Material y métodoDescripción de la técnica de navegación y estudio transversal sobre una cohorte de 20 pacientes intervenidos en nuestro centro por rotura primaria crónica del LCA desde enero de 2010 hasta mayo de 2011. Con la ayuda del navegador se definió la posición exacta de los túneles en base a referencias anatómicas intraarticulares y se realizaron pruebas de estabilidad, tanto en el plano sagital como en el axial.
ResultadosNuestra técnica de reconstrucción anatómica del LCA situó el túnel tibial a una distancia media de 16,8±4,92mm del ligamento cruzado posterior y a un 44,1%±4,35% de la anchura total del platillo tibial. La distancia media del centro del túnel femoral a la cortical posterior del cóndilo lateral fue de 7,89±2,78mm. Intraoperatoriamente y antes de la reconstrucción, los valores medios (±DE) de traslación anteroposterior, rotación interna y rotación externa de la tibia a 30° fueron de 15,5mm (±5,11); 19° (±3,62) y 19,65° (±3,26) respectivamente. Tras la reconstrucción dichos valores disminuyeron a 5,6mm (±1,72); 12,17° (±3,76) y 16,9° (±4,42).
ConclusionesEl empleo de sistemas de navegación como apoyo al cirujano permite sistematizar la posición de los túneles óseos y estandarizar el procedimiento en relación a la reconstrucción deseada. La reconstrucción del LCA según la técnica descrita, mejora la estabilidad anteroposterior y rotacional monoplanar respecto al estado preoperatorio pudiendo restablecer los valores de laxitud a los considerados como fisiológicos acorde al conocimiento científico actual.
Computer-assisted surgery was first used in the reconstruction of the anterior cruciate ligament (ACL) in the year 1990.1 Since then, different navigation software has been developed in an attempt to make ACL surgery more reproducible and quantifiable. While early navigators focused on locating and making bony tunnels,2–4 current software includes tools capable of measuring the stability of the knee in different planes, before and after ligament reconstruction, behaving as highly reliable intraoperative arthrometers.5,6
Recent biomechanical studies have indicated that reconstruction of a single bundle (or fascicle) and anatomical tunnels restore knee stability to levels similar to those of double bundle reconstruction.7
The aim of this work was to quantify anteroposterior and rotational stability pre- and postreconstruction using a monofascicular anatomical reconstruction technique, with the help of a navigator. A second aim was to describe the exact position of the tibial and femoral tunnels according to data collected by the navigator. The study hypothesis was to assume that the help of the navigator would improve the final intraoperative stability of the intervened knees.
Material and methodClinical seriesThis was a cross-sectional study on a cohort of 20 patients undergoing primary reconstruction of the anterior cruciate ligament between January 2010 and May 2011. All patients were diagnosed with chronic tears and the following inclusion criteria were established: patients with closed physis and no more than 50 years old, primary ligamentoplasties, use of any type of graft and use of navigator during surgery. The exclusion criterion established was the presence of associated lesions diagnosed by MRI or exploratory arthroscopy prior to reconstruction.
The series consisted of 15 males and 5 females with a mean age of 33.5±9.03 years. The mean period elapsed between injury and surgery was 185±34.35 days.
The operations were performed by the same surgeon in all cases. The predominant type of graft was the quadruple semitendinous plasty/gracilis muscle, which was used in 13 cases (males and females >35 years who did not practice pivoting sports), the bone–tendon–bone technique was employed in 4 males who were usual soccer players and allografts were used in 3 cases (2 males and 1 female >40 years), with the personal choice of each patient being the sole selection criterion.
Femoral tunnels were performed in all cases through the standard medial portal or an accessory medial portal, and fixation techniques used were the Retrobutton® system (Arthrex, Naples, Florida, USA) as cortical fixation in the fibula and PLLA Bio-interference Screws® (Arthrex, Naples, Florida, USA) in the tibia. We used screws which were 1mm larger than the diameter of the tunnel in the case of tendon plasties and of the same diameter in the case of bone–tendon–bone plasties.
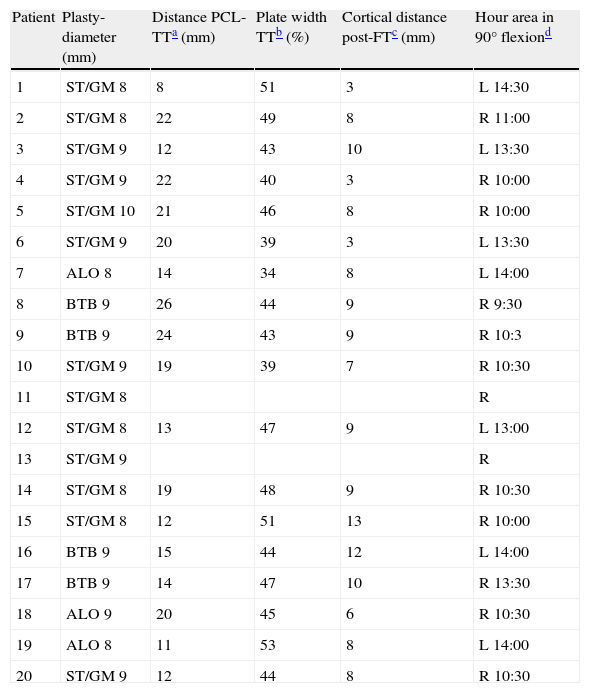
For the collection of data, we used the documentation recorded by the navigator software during the surgery of each patient. We studied the position of the tunnels in relation to intraarticular anatomical landmarks and the kinematic data concerning anterior tibial translation, external tibial rotation and internal tibial rotation at 30° flexion. Navigation of the tibial and femoral tunnels was not possible in 2 patients (11 and 13) due to errors in data collection of intraarticular anatomical landmarks. The anatomical position of these tunnels was visually verified based on previously marked bone landmarks. In these 2 patients it was possible to conduct navigator-assisted stability tests (Table 1).
Type of plasty and location of tunnels.
| Patient | Plasty-diameter (mm) | Distance PCL-TTa (mm) | Plate width TTb (%) | Cortical distance post-FTc (mm) | Hour area in 90° flexiond |
| 1 | ST/GM 8 | 8 | 51 | 3 | L 14:30 |
| 2 | ST/GM 8 | 22 | 49 | 8 | R 11:00 |
| 3 | ST/GM 9 | 12 | 43 | 10 | L 13:30 |
| 4 | ST/GM 9 | 22 | 40 | 3 | R 10:00 |
| 5 | ST/GM 10 | 21 | 46 | 8 | R 10:00 |
| 6 | ST/GM 9 | 20 | 39 | 3 | L 13:30 |
| 7 | ALO 8 | 14 | 34 | 8 | L 14:00 |
| 8 | BTB 9 | 26 | 44 | 9 | R 9:30 |
| 9 | BTB 9 | 24 | 43 | 9 | R 10:3 |
| 10 | ST/GM 9 | 19 | 39 | 7 | R 10:30 |
| 11 | ST/GM 8 | R | |||
| 12 | ST/GM 8 | 13 | 47 | 9 | L 13:00 |
| 13 | ST/GM 9 | R | |||
| 14 | ST/GM 8 | 19 | 48 | 9 | R 10:30 |
| 15 | ST/GM 8 | 12 | 51 | 13 | R 10:00 |
| 16 | BTB 9 | 15 | 44 | 12 | L 14:00 |
| 17 | BTB 9 | 14 | 47 | 10 | R 13:30 |
| 18 | ALO 9 | 20 | 45 | 6 | R 10:30 |
| 19 | ALO 8 | 11 | 53 | 8 | L 14:00 |
| 20 | ST/GM 9 | 12 | 44 | 8 | R 10:30 |
ALO: allograft; BTB: bone–tendon–bone; FT: femoral tunnel; L: left; PCL: posterior cruciate ligament; R: right; ST/GM: semitendinous/gracilis muscle; TT: tibial tunnel.
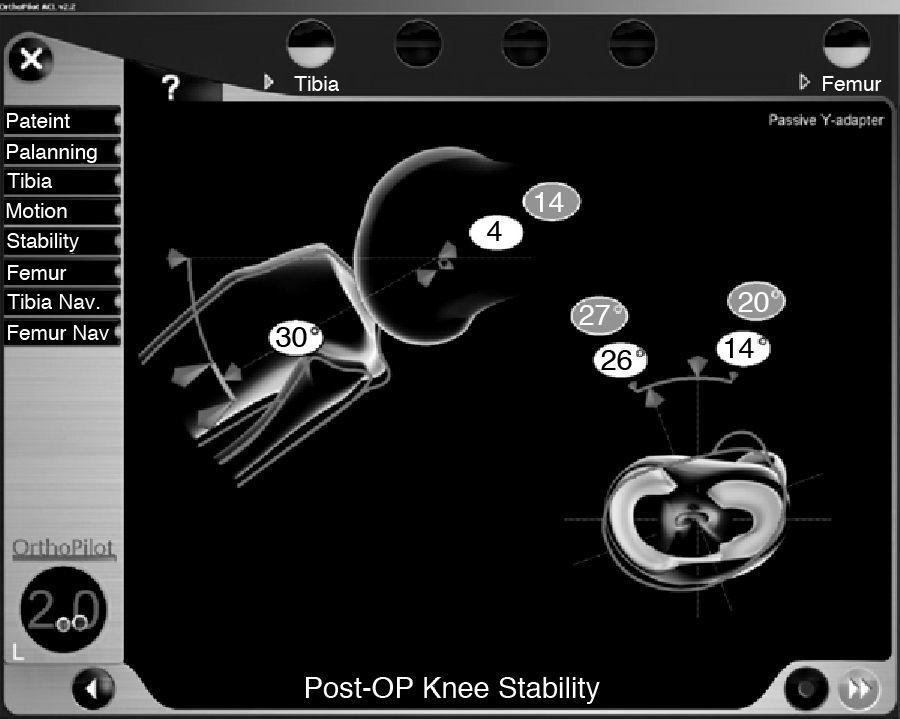
The Orthopilot® navigation system (v.2.1, B. Braun-Aesculap, Tuttlingen, Germany) for ACL reconstruction can be used with any type of graft and fixation technique as the software does not require preoperative radiological data input. This is a passive navigation system using infrared sensors and emitters, of which 2 are fixed to the fibula and tibia using Kirschner wires and 1 is used freely in the various hand tools. Navigation in ACL reconstruction consisted of 4 phases:
Marking of extraarticular anatomical landmarks: the anterior tibial tuberosity, the anterior tibial crest in its middle-distal third and the medial and lateral edges of the tibial plate were located with a straight pointer and its corresponding emitter. Subsequently, a kinematic registry of the knee between 0° and 90° was carried out (Fig. 1).
Preligamentoplasty stability test: the anterior and rotational displacements of the tibia at 30° flexion were recorded in the computer under maximum manual force.
Marking of intraarticular anatomical landmarks and location of tunnels: the anterior edge of the posterior cruciate ligament, anterior horn of the lateral meniscus, medial tibial spine, anterior edge of the notch, the insertion area of the cruciate in the medial wall of the lateral condyle, the “over the top” position at 12 O’clock on the posterior edge of the notch (time reference provided by the software taking into account the position of the knee at 90° flexion and a frontal plane cutting transversally across the distal fibula) and the posterior cortex in the time zone selected for the femoral tunnel were palpated with different types of pointers and visualised through the arthroscope. Once the intraarticular references had been marked, the tibial tunnel was made with a special guide on which the mobile emitter was placed. The exit point of the guide wire from the tibial tunnel was located according to the data provided previously. Similarly, with the aid of the pointer, we located the centre of the femoral tunnel in the wall of the condyle.
Postligamentoplasty stability test: after the plasty was introduced and fixed we assessed the quality of reconstruction by quantifying anteroposterior and rotational stability of the tibia at 30° knee flexion once again (Fig. 2).
Statistical studyData regarding the position of the tunnels, as well as the results of stability tests before and after reconstruction were collected using a database created for this purpose. All results are shown as mean±standard deviation. This documentation was processed by the Department of Clinical Research at our centre, using the nonparametric Wilcoxon test for the comparison of pre–post values in the different stability tests. Statistical significance was considered at P<.05.
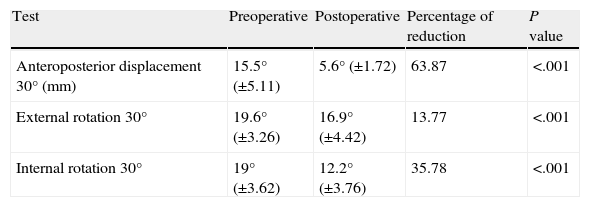
ResultsThe results are shown in Table 2. The mean value of anteroposterior displacement of the tibia at 30° before reconstruction was 15.5±5.11mm. After fixation of the plasty, this value was reduced to 5.6±1.72mm (P<.001). Starting from a neutral rotation to 30° flexion, the maximum displacement in internal rotation preligamentoplasty was 19±3.62° and in external rotation it was 19.65±3.26°. After anatomical reconstruction, rotational laxity was fundamentally reduced at the expense of internal rotation with values of 12.17±3.76° versus 16.9±4.42° external rotation (P<.001 for both values).
Pre- and postreconstruction laxity of the anterior cruciate ligament.
| Test | Preoperative | Postoperative | Percentage of reduction | P value |
| Anteroposterior displacement 30° (mm) | 15.5° (±5.11) | 5.6° (±1.72) | 63.87 | <.001 |
| External rotation 30° | 19.6° (±3.26) | 16.9° (±4.42) | 13.77 | <.001 |
| Internal rotation 30° | 19° (±3.62) | 12.2° (±3.76) | 35.78 | <.001 |
Regarding the position of the tunnels, the tibial tunnel was located at a mean distance of 16.8±4.92mm from the posterior cruciate ligament and 44.1±4.35% (medial) of the total width of the plate. The femoral tunnel was located at a mean distance of 7.89±2.78mm from the posterior femoral cortex of the lateral condyle. Considering the time reference of the software with the knee at 90° flexion, the femoral tunnels in right knees were placed at 09:30 and in left knees at 14:30.
There were 2 complications related to the navigation technique described: 1 first-degree burn in the middle third of the anterior tibial region due to the heat produced by the Kirschner wire of the emitter and 1 breakage of the threaded needle tip during extraction, which became included within the tibia.
DiscussionIn the present study we noted mean values of anterior translation, internal rotation and external rotation at 30° flexion after reconstruction of 5.6mm, 12.2 and 16.9°, respectively, compared to 15.5mm, 19 and 19.6°, as mean preoperative values in knees without ACL. Quantification of the final stability of the knee after ligamentoplasty enables us to compare these values with those previously reported in healthy and stable knees. Using the Orthopilot® navigator and the same software version, Song et al. performed stability tests in knees with ACL injury before and after reconstruction and compared them with the same test performed in healthy contralateral knees. Regarding anterior tibial translation at 30° in healthy knees, they obtained values of 6.7mm vs 14.7mm in injured knees.8 These findings were similar to those observed by Daniel MD et al. in 1985 using different measuring instruments, but obtaining anterior displacements at 30° of 7.5mm in healthy knees compared to 13mm in ACL deficient knees under loads of 89 newtons.9 In our work, we obtained a reduction of internal rotation of 36% versus 14% external rotation compared to preoperative values. The correction of rotational instability (kinematic function of ACL, along with AP translational control) observed was in accordance with the current work of Miura et al. and Song et al.8,10 Both studies compared stability test results with the healthy contralateral knee. The overall rotation (internal rotation+external rotation) in healthy knees in both studies was 36.4±2.7° and 31.4±4.2°, respectively. In our study, the mean overall rotational stability after reconstruction was 29.1±2.6°, a value similar to those observed earlier in healthy knees.
The anatomical monofascicular technique achieves a more horizontal, superficial and lower placement of the plasty than that obtained with conventional techniques, in which the femoral tunnel is created through the tibial tunnel, thus obtaining central and more vertical plasties. Recent biomechanical studies have shown that the monofascicular anatomical reconstruction technique restores anteroposterior and rotational stability to the same levels as the bifascicular technique.7,11,12 The residual rotational instability after ACL reconstructive surgery is a subject of debate. Several authors have shown how single bundle reconstructions with kinematically lower femoral insertions perform better than traditional plasties placed in a higher position in the intercondyle. Loh et al. compared various plasty sites with femoral tunnels at 11h versus tunnels at 10h. The latter resisted anterior translation better in response to rotatory loads.13 Similarly, Scopop et al. compared kinematic measurements in bone–tendon–bone (BTB) reconstructions and traditional femoral tunnels (high) versus lower tunnels and found that, at 30° flexion, knees with lower femoral tunnels presented a correction of tibial internal rotation to near normal values, compared with the traditional technique.14
New software from different manufacturers allows us to perform stability tests including translational and rotational measurements, thus enabling us to assess the effect of different surgical procedures on knee stability and better describe specific laxity in each patient. There have been comparative studies with other kinematic measurement systems, such as the KT-1000 (MEDmetric Corp, San Diego, California), Rolimetro (Aircast Europe, Neubeuern, Germany), etc., which have demonstrated the reliability, accuracy and inter- and intraobserver reproducibility of measurements obtained with the different navigators.15,16 In a series of 79 patients, Martelli et al. have shown an intrasurgeon variability of kinematic measurements navigated in knees before and after ACL reconstruction below 1mm for anteroposterior translations and below 1.6° for external and internal rotations.17
In our study we used a vaporiser to mark the area of insertion for the creation of tunnels. However, in the medial wall of the femoral condyle and after cleaning the ligament remains from the anatomical insertion, we often navigated based on the bone ridges described in the work of Fu et al.18,19 The navigator only recorded the position of the centre of these tunnels (guide needles) in relation to intraarticular anatomical landmarks marked previously with the pointer. That is, in our work we did not use navigation as an aid in the location of the tibial and femoral tunnels, but only as a way to record them. However, the navigator quantified the exact distance from the centre of the femoral tunnel to the posterior cortex with more precision, thus offering greater safety for the drilling of tunnels. As an interesting fact, the tibial tunnel was located about 16mm from the edge of the posterior cruciate ligament (PCL), a more anterior point than that obtained with most of the guides that rely on this ligament. The femoral tunnel always respected 3–4mm of the posterior cortex, with a tendency to get closer to the condylar insertion of the anteromedial bundle. In agreement with current works, we believe that in experienced hands navigation does not provide benefits for the performance of the tibial tunnel,20,21 but its use may represent an effective support tool for surgeons lacking sufficient experience. Most articles report a better positioning of the femoral tunnel in reconstructions assisted by navigation compared to standard ones.22,23 Navigation of the tunnels in our study was only a secondary objective, aimed at quantifying their position with the future objective of systematising our surgical technique.
It must be noted that navigators require an invasive technique with fixation of the emitters to the bone through the use of Kirschner wires, thus involving potential complications. In our series, we only noted 2 complications: 1 first-degree burn in the tibial region caused by the heat transmitted by the Kirschner needle upon entry (this was easily resolved with local cures in consultation) and 1 patient in whom the threaded tip of the needle broke during its removal, becoming included within the tibia, and without complications during the postoperative or follow-up periods. In the future, the development of less invasive techniques will enable intraoperative kinematic comparison with the healthy knee and even the possibility of using navigators in consultation for follow-up.
Our work presents 2 types of constraints: some linked to the navigation tool itself and others related to the study design. The Orthopilot® navigator uses software which allows us to perform uniplanar stability tests: either anterior translation of the tibia in the sagittal plane or rotational manoeuvres in an axial plane. Recently, Bull et al.24 published how these clinical tests assess 2 types of joint instability: static and dynamic. Static measurements are generally associated with uniplanar laxity tests, whereas patients with symptoms refer dynamic knee instability. We attempted to reproduce the latter through multiplanar exploratory tests with pivot shift. At present, various navigation software for ACL surgery are working on quantifying the pivot shift manoeuvre intraoperatively, with promising results and potential future application in knee surgery.25–27 Another limitation of the navigator is the use of manual forces to carry out stability tests, decreasing the reproducibility of such measurements and generating a source of bias. In our study, examinations were performed by the same surgeon in all cases, attempting to simulate the manoeuvres performed in consultation. Future studies should use quantitative systems to ensure a constant external force, in order to improve the reproducibility of laxity measurements. As for the limitations of study design, these include its descriptive character, the small sample size, the use of different types of plasties and the absence of comparisons with the healthy contralateral knee. Future prospective and comparative studies may demonstrate how navigation could make anterior cruciate ligament surgery a more reproducible and individualised technique, tailored to the anatomical and kinematic characteristics of each patient. Similarly, future comparative studies will be needed to demonstrate, firstly, the better kinematic control of plasties placed with computer-assisted surgery and, secondly, its clinical usefulness, obtaining better functional results in the medium and long term.
ConclusionsACL reconstruction using the technique described improves monoplanar anteroposterior and rotational stability with respect to the preoperative condition and may restore these values to those observed in healthy knees.
Level of evidenceLevel of evidence IV.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: García-Bógalo R, et al. Evaluación mediante navegación intraoperatoria de la laxitud del ligamento cruzado anterior en su reconstrucción anatómica monofascicular. Rev Esp Cir Ortop Traumatol. 2012; 56:267–73.